Type 2 Diabetes Mellitus - quality prescribing strategy: improvement guide 2024 to 2027
This quality prescribing guide is intended to support clinicians across the multidisciplinary team and people with Type 2 Diabetes Mellitus (T2DM) in shared decision-making and the effective use of medicines, and offers practical advice and options for tailoring care to the needs and preferences of individuals.
3. What to consider when individualising a care plan using a person-centred approach
Multimorbidity (with polypharmacy)
Multimorbidity is defined by the World Health Organization as the co-occurrence of two or more chronic medical conditions in one person.[21] Multimorbidity increases markedly with age. In a Scottish study, multimorbidity was prevalent in 81.5% of individuals aged 85 years and over, with a mean number of 3.62 morbidities[22] (see Figure 4).
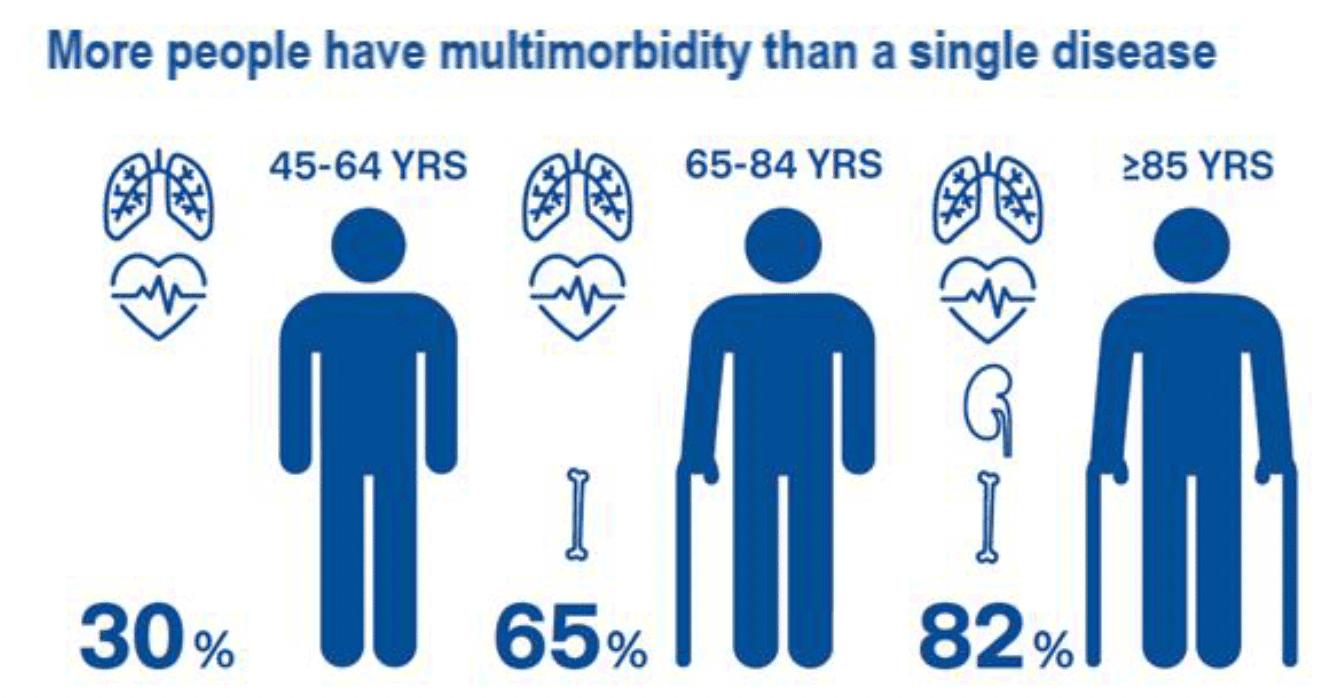
Graphic text below:
More people have multymorbidity than a single disease
- 30% in 45-64 years
- 65% in 65-84 years
- 82% in over 85 years
The most prevalent chronic conditions in primary care were hypertension (33.5%), hyperlipidemia (33.0%), and depression (18.7%).[23] The presence of multiple long-term conditions results in a combined negative effect on physical and mental health, and can affect a person’s quality of life, limiting daily activities and reducing mobility.[24]
The over 60-year-old population uses nearly three times more medicines as the general population, with adherence to long-term medication ranging between 25-70%.[25]
The major predictors of risk of experiencing medication-related harm[26] are age, number of long-term conditions and number of medications taken. People with multiple long-term conditions utilise primary care services twice as much, and are three times as likely to be hospitalised, than those without multiple long-term conditions.[8],[26] This carries with it a large economic burden[27] for health care services.
Care should be person-centred and coordinated to ensure the greatest possible individual outcomes. This is most achievable when there is integrated care approach that places the individual at the centre. Scottish Government has various work streams driving the improvement in person-centred care at national, board and patient level including Person-centred Care,[28]Polypharmacy Guidance[8] and Realistic Medicine.[9]
Person-centred care
The person should be at the centre of every consultation, to ensure a holistic approach to care. There are several models of care which can be adopted, e.g. House of Care.[29]
The decision cycle for person-centred glycaemic management in T2DM[3] summarised below in Figure 5. This based on a full version produced by the American Diabetes Association and European Association for the Study of Diabetes.
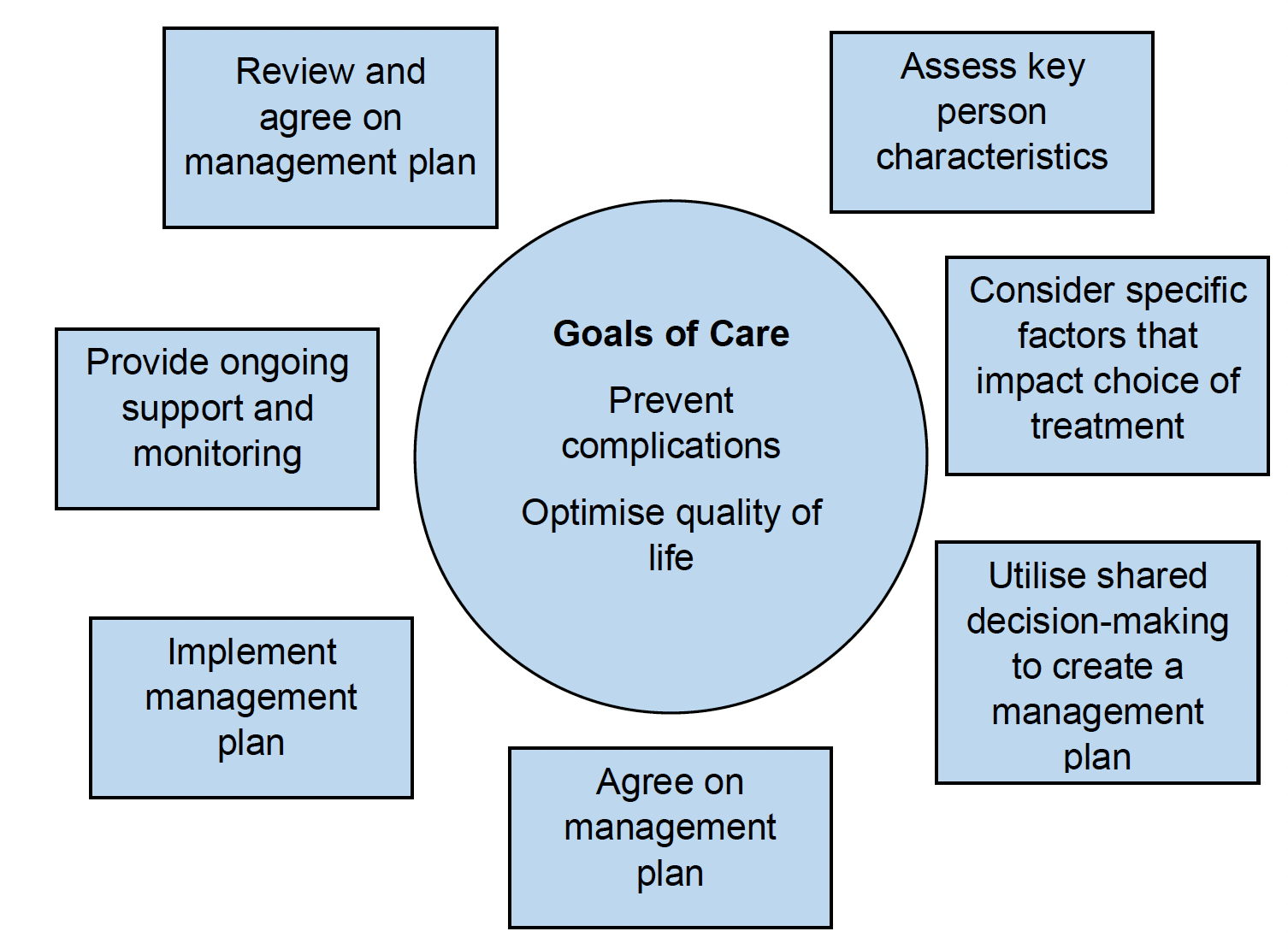
Graphic text below:
Goals of Care:
- Prevent complications
- Optimise quality of life
- Assess key person characteristics
- Consider specific factors that impact choice of treatment
- Utilise shared decision-making to create a management plan
- Agree on management plan
- Implement management plan
- Provide ongoing support and monitoring
- Review and agree on management plan
Each section should be viewed with the person at the centre of decision-making. Focusing on the whole person alongside their medication during the review will ensure the person remains central in the decision-making process and is not a passive recipient of care. This in turn encourages self-care and an understanding of how their condition/s impacts on their life.
This multifaceted approach is in line with Scottish Government’s Realistic Medicine Approach to care. The medication algorithm allows individualised choice and firmly focuses on the evidence from long-term outcome trials and the benefits seen with newer agents (section 6), asking clinicians to decide at an early stage whether a person will gain from these benefits independent of HbA1c. The person-centred 7-Steps medication review process can be used at initiation and review of medication to support shared decision-making throughout the process.
Benefits of improved glycaemic control
Hyperglycaemia is central to development and progression of microvascular and macrovascular disease.
The epidemiological analysis of the UK Prospective Diabetes Study (UKPDS)[30] demonstrated a strong relationship between diabetes complications including mortality and blood glucose levels (see Table 3).
| End point | Percentage reduction |
|---|---|
| Microvascular complications | 37% |
| Any endpoint or death related to diabetes | 21% |
| Diabetes-related mortality | 21% |
| Myocardial infarction | 14% |
Factors which may lead to loss of adequate glycaemic control
When creating and reviewing individual care plans, the following factors should be considered that may lead to loss of adequate glycaemic control:
- lifestyle and diet
- raised BMI
- medication non-adherence
- depression
- musculoskeletal injury or worsening arthritis
- competing illnesses perceived as more important by the individual
- social stress/anxiety at home or at work
- substance misuse
- infections
- use of medications (such as corticosteroids, certain depression medications [paroxetine], mood stabilisers, or atypical antipsychotics) that elevate weight or glucose
- other endocrinopathies such as Cushing's disease
Individualisation of glycaemic control
Good glycaemic control is valuable in promoting fewer complications in patients with T2DM, but good individualised glycaemic control is a based on an appreciation of the below factors:
- life expectancy
- disease duration
- important comorbidities, including frailty
- established vascular complications
- patient preference
- resources and support system
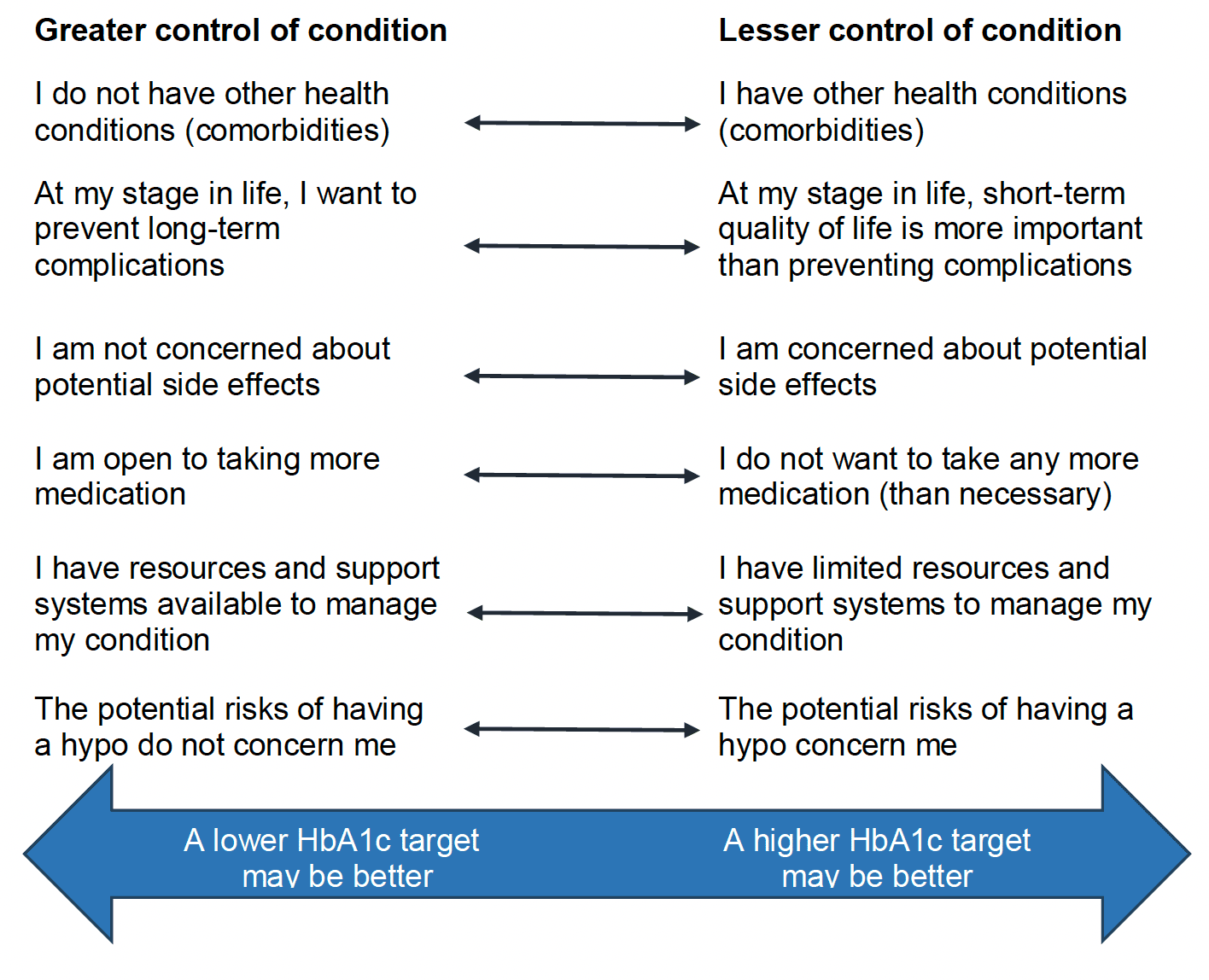
Graphic text below:
Greater control of condition
- I do not have other health conditions (comorbidities)
- At my stage in life, I want to prevent long-term complications
- I am not concerned about potential side effects
- I am open to taking more medication
- I have resources and support systems available to manage my condition
- The potential risks of having a hypo do not concern me
- A lower HbA1c target may be better
Lesser control of condition
- I have other health conditions (comorbidities)
- At my stage in life, short-term quality of life is more important than preventing complications
- I am concerned about potential side effects
- I do not want to take any more medication (than necessary)
- I have limited resources and support systems to manage my condition
- The potential risks of having a hypo concern me
- A higher HbA1c target may be better
Figure 6 (based on ADA[31] and NICE,[2] and supported by SIGN 154[1]) shows characteristics and considerations that individuals and clinicians can consider together to assess “what matters to me” (step 1 of the 7-Steps medicine review process) when determining individual glycaemic control.
People with T2DM should consider their options for controlling their blood glucose in order to reduce the long-term risks of diabetes.
Table 4 illustrates an alternative individualised approach to diabetes care should be adopted that is tailored to the needs and circumstances of people with T2DM, accounting for personal preferences.
| A | Age | Less stringent HbA1c targets with increasing frailty. |
|---|---|---|
| B | Body weight | Be aware of which drugs affect body weight.
|
| C | Complications | Co-incident complications will impact drug selection e.g., patient with eGFR< 30ml/min/1.73m[2] should avoid metformin. |
| D | Duration |
|
Reassess the individual’s needs and circumstances at each review and consider discontinuing any medicines that are not effective in line with polypharmacy guidance.
Contact
Email: EPandT@gov.scot
There is a problem
Thanks for your feedback