Type 2 Diabetes Mellitus - quality prescribing strategy: improvement guide 2024 to 2027
This quality prescribing guide is intended to support clinicians across the multidisciplinary team and people with Type 2 Diabetes Mellitus (T2DM) in shared decision-making and the effective use of medicines, and offers practical advice and options for tailoring care to the needs and preferences of individuals.
8. Which individuals with T2DM should have glucose monitoring?
Blood glucose monitoring
Self-management by regular blood glucose monitoring is not routinely recommended in people with T2DM[1] as it does not significantly improve glycaemic control, health-related quality of life, or hypoglycaemia rates.
However, self-monitoring of blood glucose is recommended for those who:
- are on insulin
- have had prior hypoglycaemic episodes
- drive or operate machinery and use oral medications, such as sulfonylureas, that increase their risk of hypoglycaemia (see DVLA guidance)
- are pregnant, or planning to become pregnant, or
- those undergoing significant changes in pharmacotherapy, e.g. on high dose oral steroids or oral hypoglycaemic agents such as sulfonylureas that require dose adjustment.
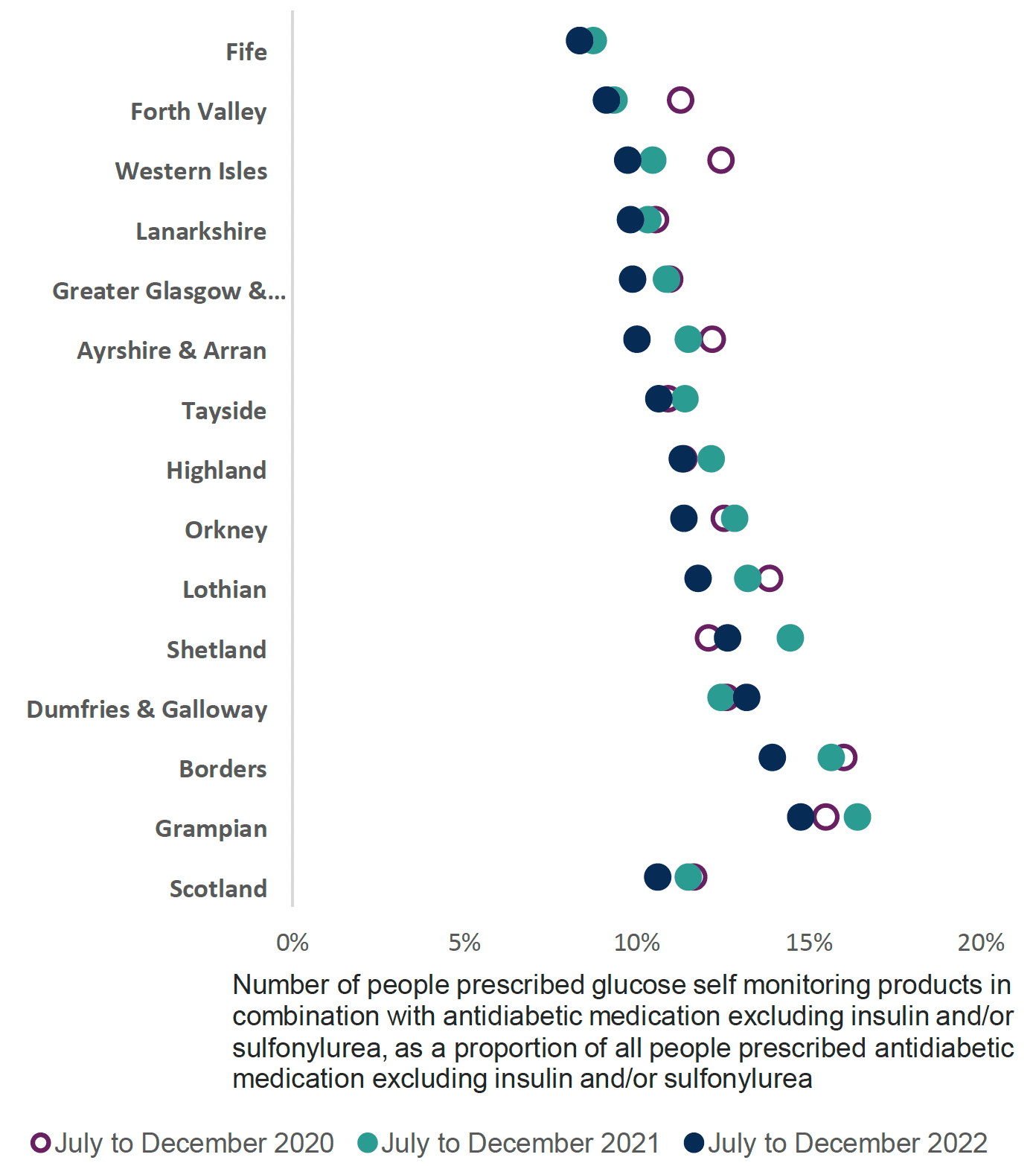
National Therapeutic Indicator
Proportion of those prescribed glucose self-monitoring products in combination with antidiabetic medication excluding insulin and/or sulfonylurea, as a proportion of all people prescribed antidiabetic medication excluding insulin and/or sulfonylurea.
This indicator (Chart 6) should have a low value, because self-monitoring glucose (SMG) is not generally recommended in management of T2DM, unless therapy includes insulin and/or sulfonylureas.
For those who require self-monitoring of blood glucose, there is no evidence to suggest greater clinical benefit from using more expensive test strips over less costly ones and therefore NHS Boards should select appropriate formulary products.
The Scottish Therapeutic Utility (STU) supports the NTI’s and has prescribing indicators that can be used to identify individuals with T2DM at GP practice level who would benefit from review.
Intermittently Scanned (Flash) Glucose Monitoring
The Scottish Health Technologies Group (SHTG) advice[49] in 2018 recommended the availability of flash glucose monitoring for individuals with diabetes who are actively engaged in the management of their condition and who intensively manage their disease with multiple daily insulin injections or insulin pump therapy, with some restrictions. NICE define multiple daily injections as ‘two or more daily insulin injections, which could either be a basal-bolus regimen or more than one daily insulin injection.’
NICE guidance[2] supports the pre-existing guidance from SHTG and recommends offering intermittently scanned continuous glucose monitoring (isCGM), commonly referred to as 'flash' glucose monitoring, to adults with T2DM on multiple daily insulin injections if any of the following situations apply:
- recurrent hypoglycaemia or severe hypoglycaemia
- impaired hypoglycaemia awareness
- a condition or disability (including learning disability or cognitive impairment) where the individual cannot self-monitor blood glucose using capillary blood glucose monitoring but could use an isCGM device (or have it scanned for them)
- would otherwise be advised to self-measure at least eight times a day (SHTG recommend at least six times per day)
Additionally, adults with insulin-treated type 2 diabetes who would otherwise need help from a care worker or healthcare professional to monitor their blood glucose, should be offered isCGM.
Good practice point:
Those prescribed flash glucose monitors only require two sensors per 28 days (26 within a year). If the sensors become detached or are faulty, people should contact the manufacturer directly for replacements. It is good practice to utilise prescribing data to identify patients who may be over-ordering and/or put in place mechanisms to prevent this, such as annual serial prescription for 26 sensors, to reduce inappropriate prescribing and associated costs.
For all individuals requiring glucose monitoring there should be a documented plan outlining frequency and duration of testing, along with what to do with results. Most people require diabetes assessments every three to six months and this should be tailored according to the individual needs to improve care. Use of diabetes digital resources to support self-management are recommended, such as My Diabetes My Way (see List 1 for further resources).
Blood ketone testing in T2DM
- People with Type 1 diabetes (insulin dependent) will test for ketones if their blood glucose levels are significantly high to alert to the risk of ketoacidosis
- Blood ketone testing in T2DM is not normally necessary and individuals are not routinely provided with self-monitoring equipment
- However due to the risk of eDKA, if a person displays symptoms of DKA (including rapid weight loss, nausea or vomiting, abdominal pain, fast and deep breathing, sleepiness, a sweet smell to the breath, a sweet or metallic taste in the mouth, or a different odour to urine or sweat) ketone testing should occur[45],[46]
- Clinicians should be aware of this recommendation and have access to the necessary equipment
Contact
Email: EPandT@gov.scot
There is a problem
Thanks for your feedback