Type 2 Diabetes Mellitus - quality prescribing strategy: improvement guide 2024 to 2027
This quality prescribing guide is intended to support clinicians across the multidisciplinary team and people with Type 2 Diabetes Mellitus (T2DM) in shared decision-making and the effective use of medicines, and offers practical advice and options for tailoring care to the needs and preferences of individuals.
14. National Therapeutic Indicators
National Therapeutic Indicators (NTIs), use prescription data to provide a measure of prescribing activity in specified therapeutic areas and a comparison across NHS Boards, Health and Social Care Partnerships (HSCPs), GP clusters and GP practices. The online tool shows a number of NTIs across varying localities.[70]
Polypharmacy in Diabetes (see section 2)
This NTI highlights individuals prescribed three or more categories of anti-diabetic drugs. These patients may also be prescribed additional medication for other comorbidities, further increasing the risks associated with polypharmacy.
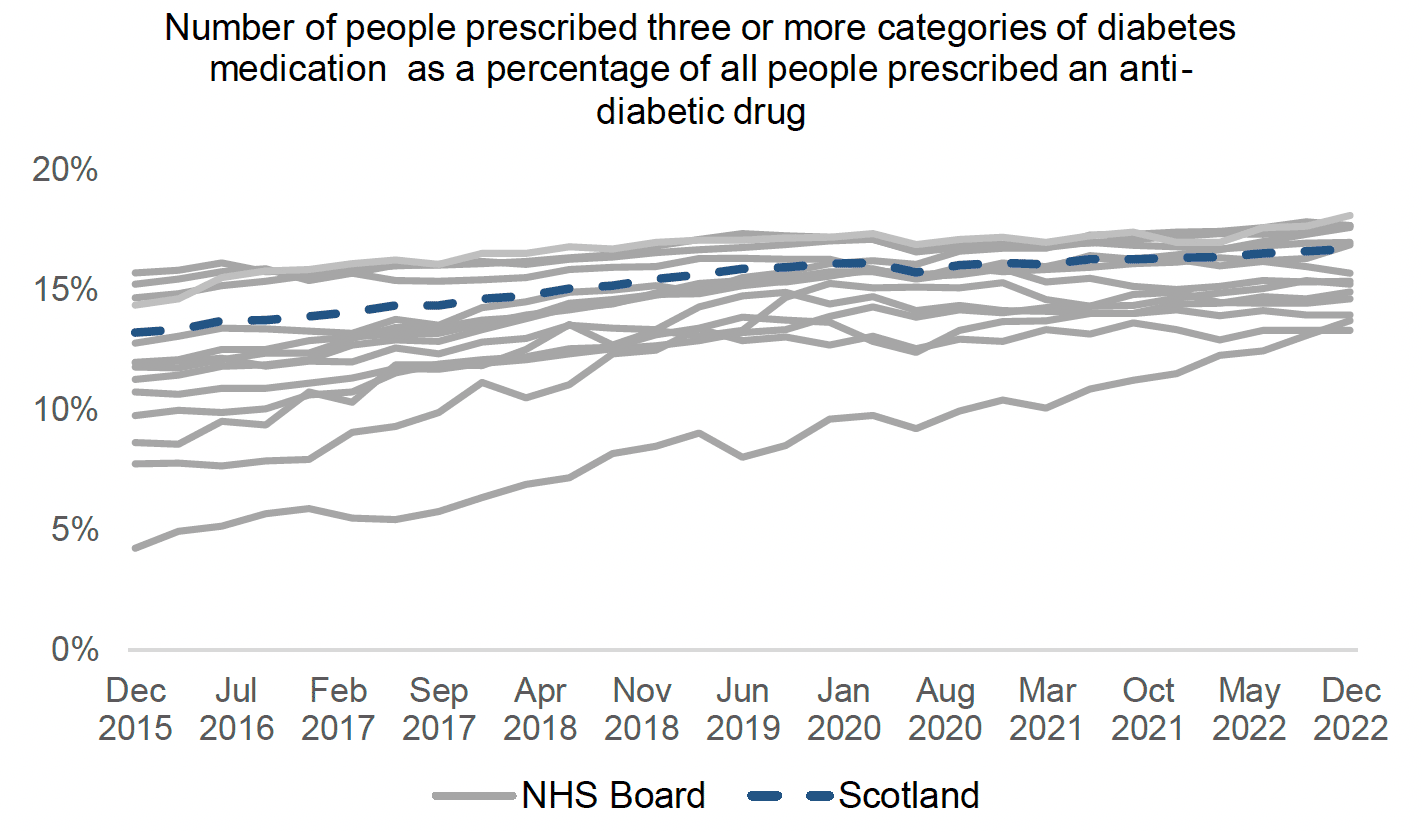
- Polypharmacy can be appropriate, ensuring that people with diabetes achieve target HbA1c levels.
- Polypharmacy can also be inappropriate either;
- due to over treatment, e.g., increasing risks of hypoglycaemia and falls;
- ineffective polypharmacy resulting in increased risks of adverse effects, but no benefit in treatment outcomes.
- The various categories of anti-diabetic medication have differing effects on glycaemic control and therefore those less effective in achieving the target HbA1c should be reviewed.
- Polypharmacy increases the risk of adverse drug reactions.
- The 7-Steps medication review process should be used during medicine reviews.
- Prescribers should work with patients to develop an understanding of the importance of self-management and the successful achievement of goals. This will include aspects such as Medication sick day guidance and lifestyle changes.
Action required by NHS boards/clusters/practices:
- It is currently possible to identify people on triple therapy in GP practice and it is recognised that many people with T2DM will require triple therapy for disease control. However, the risks associated with this increase with age/frailty and comorbidity.
- GP Clusters and practices can review their data with others in the board and consider what quality improvement projects may be suitable based on available data.
- Identify individuals who are:
- prescribed more anti-diabetic medication than required to meet target glycaemic control and reduce therapy
- Safety issue: no evidence to support co-prescribing of DPP-4i/gliptins and GLP-1RA and this should be avoided. Action to stop gliptin
- within target HbA1c range but prescribed medication with less efficacy– stop less/ ineffective therapies
- not at target HbA1c despite polypharmacy. Action change in therapy to achieve target glycaemic control, especially less efficacious medication. Prioritise younger individuals for more aggressive treatment
- prescribed selected anti-diabetic medication less suitable/contra-indicated for comorbidities and prescribe suitable alternative
- NHS Boards should review formulary treatment algorithms.
- Utilise clinical decision support tools to aid prescribers in treatment choices including Manage Medicines app/website.
- Review people with dual diagnosis of T2DM, depression and poor glycaemic control.
Metformin as percentage of all people prescribed an anti-diabetic drug (see section 5)
Metformin remains first line treatment for majority of patients. This NTI should have a high percentage for this indicator.
- Metformin should be prescribed first line unless there is a contraindication (eGFR<30ml/min, or lactic acidosis) or true intolerance (which can be reduced by prescribing sustained release preparations).
- There should be a high percentage of patients who are prescribed metformin.
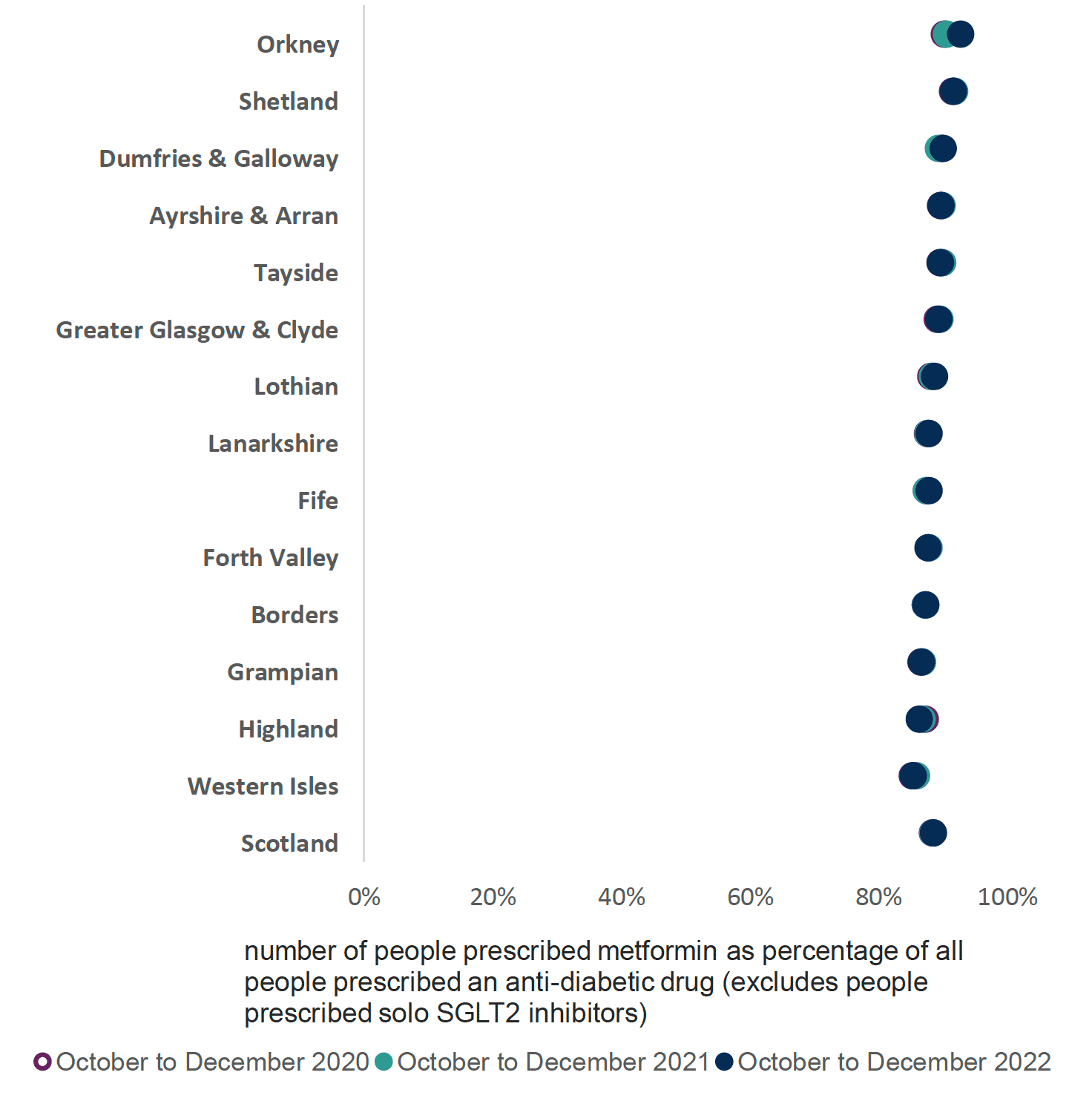
Action required by NHS boards/clusters/practices:
- NHS Boards/MCNs/Prescribing groups should review their data in comparison to other boards to determine areas of unwarranted variation.
- GP Clusters and practices can review their data with other practices or cluster regions to show variation in their prescribing practices.
- Identify missing individuals: Clusters and practices should identify those who are suitable for metformin but not currently prescribed this. Prioritise younger individuals for more aggressive treatment.
- Safety consideration: Ensure appropriate dosage in line with renal function, e.g. metformin dose should be reduced if eGFR falls below 45 and stopped if eGFR<30.
Medication should be reviewed in line with the 7-Steps.
Individuals with Type 2 diabetes and existing atherosclerotic cardiovascular disease (ASCVD) who may benefit from treatment with SGLT-2i and/ or GLP-1RA. (see Section 6)
This indicator should have a high level of SGLT-2i and/or GLP-1RA prescribing, indicating good practice, with suitable patients receiving appropriate medication.
- These medicines have positive evidence for cardiovascular and renal outcomes and additional indications for use – ASCVD, HF, CKD – (independent of glycaemic control).
- Due to these comorbidities, there may be individuals with T2DM who may benefit from these therapies, especially if glycaemic control not at target.
- A higher level of SGLT-2i and/or GLP-1RA indicates good practice, with suitable patients receiving appropriate medication.
- Prioritise younger individuals for more aggressive treatment.
N.B. PIS prescribing data is unable to directly identify those with a read code diagnosis of ASCVD, chronic HF or CKD. Therefore, a surrogate marker of those co-prescribed nicorandil and/or GTN/ISMN for ASCVD is utilised.
The NTI identifies individuals prescribed SGLT-2i and/or GLP-1RA in the same quarter as a nitrate and/or nicorandil, aspirin or clopidogrel, as a proportion of people prescribed anything from BNF 060102 in the same quarter as a nitrate and/or nicorandil, aspirin or clopidogrel. This surrogate marker indicates there is a proportion of those with T2DM who may benefit from treatment with SGLT-2i* or GLP-1RA, irrespective of glycaemic control.
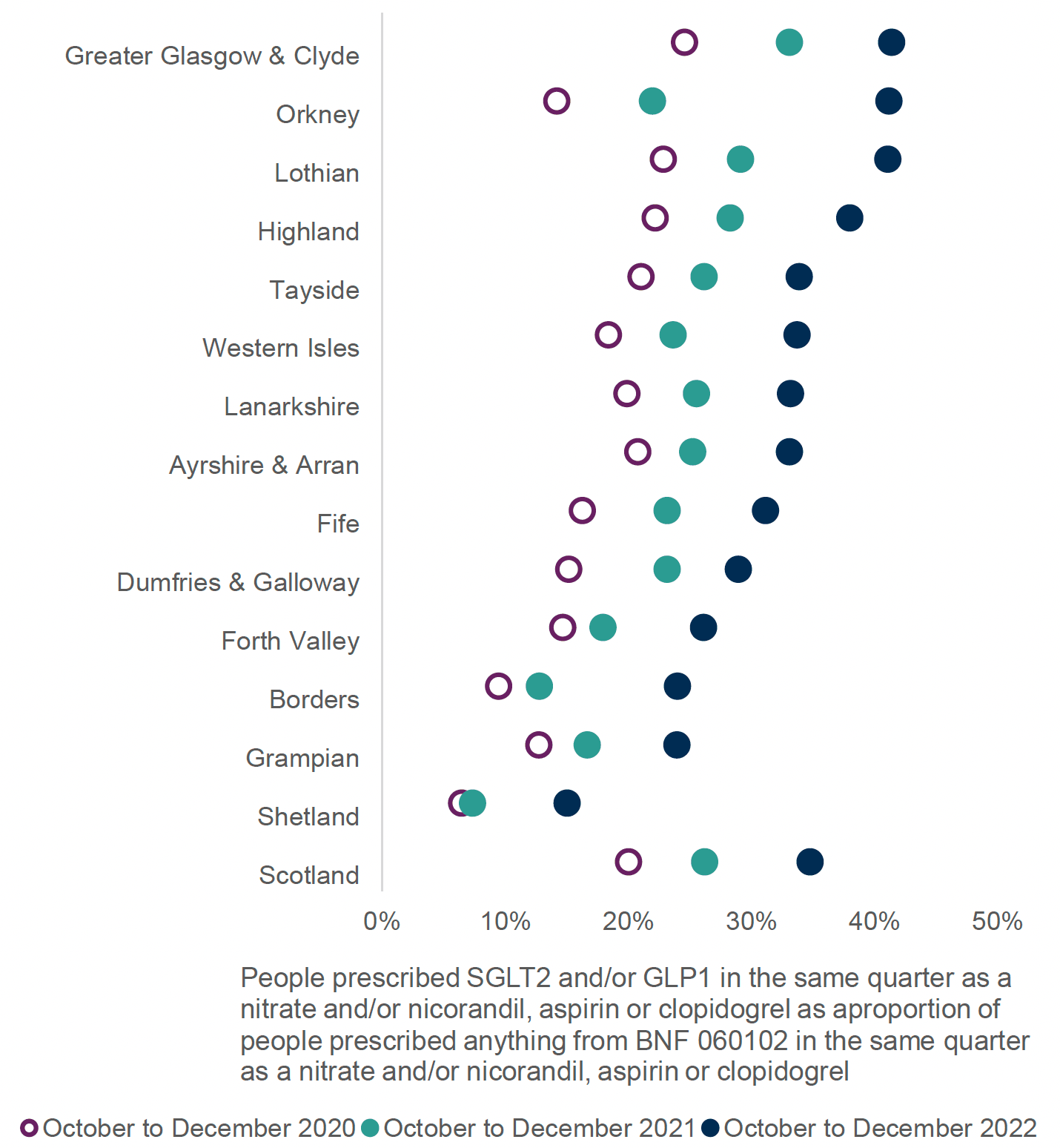
GP Clusters should identify practices which are lower users of SGLT-2i/GLP-1RA and consider if there may be unwarranted variation.
Action required by NHS boards/clusters/practices:
- Identify individuals who would benefit from prescribing of SGLT-2i* or GLP-1RA:
- Individuals with T2DM with existing CVD but not prescribed SGLT-2i*/GLP-1RA.
- Individuals with T2DM with high ASSIGN/QRISK2 score not on SGLT-2i*/GLP-1RA.
- Individuals with T2DM with renal disease, based on (eGFR and) ACR values – identified individuals should have all meds reviewed to ensure doses appropriate for degree of renal impairment. NB it is acknowledged that many people will not have an ACR recorded and therefore to aid identification of suitability for SGLT-2i*/GLP-1RA prescribing, screening with eGFR may be required initially, with an ACR recorded thereafter.
- Target younger individuals with T2DM as priority candidates for more aggressive treatment.
- Boards to review formularies/treatment algorithms to ensure prescribing in line with current guidance.
- The 7-Steps medication review process should be used.
Self-monitoring of glucose: proportion of people prescribed glucose self-monitoring products in combination with antidiabetic medication excluding insulin and/or sulfonylurea, as a proportion of all people prescribed antidiabetic medication excluding insulin and/or sulfonylurea (see section 8).
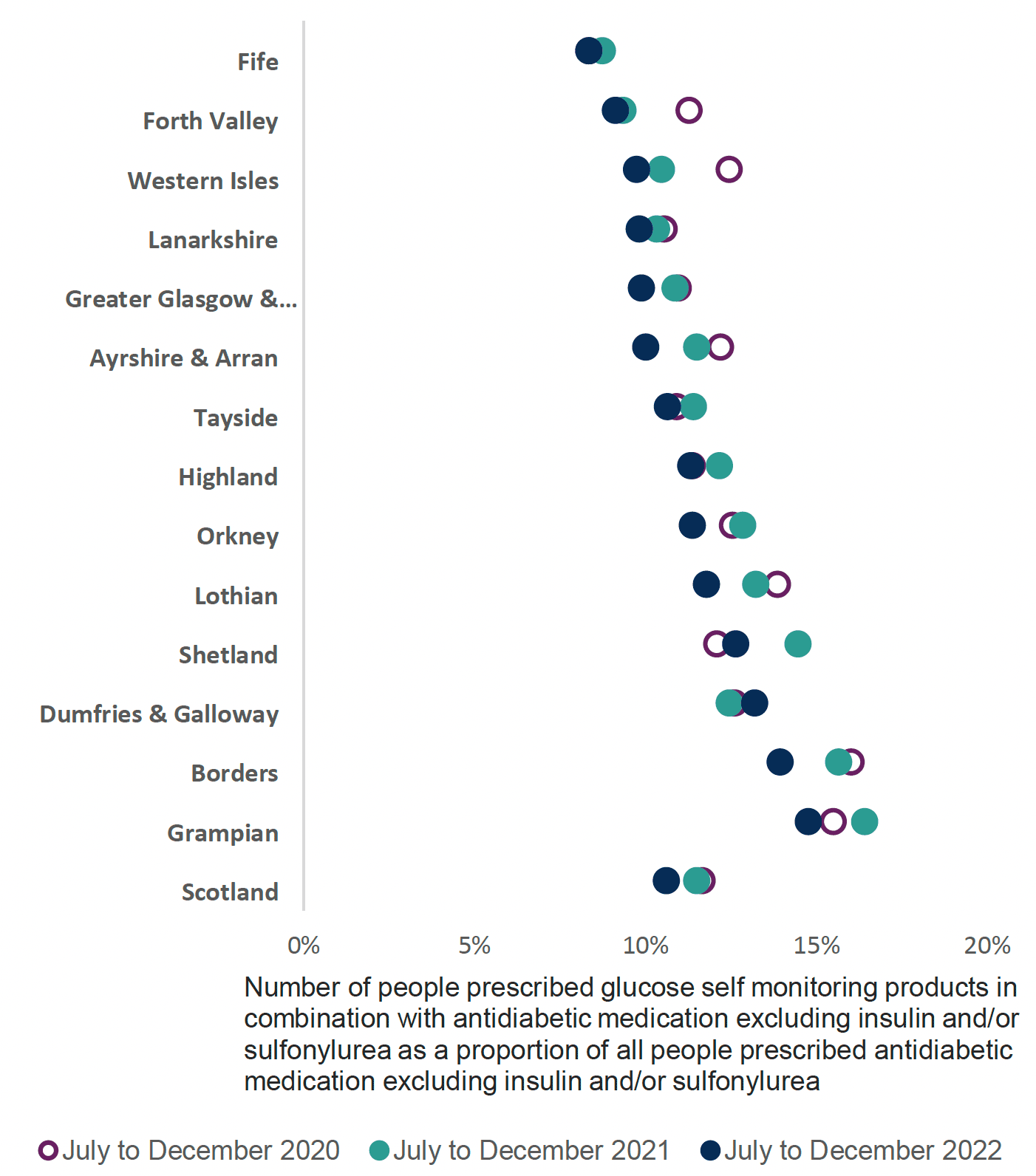
Self-Monitoring Glucose (SMG) is not generally recommended in management of type 2 diabetes.
This indicator should have a low value.
Do not routinely offer SMG for adults with type 2 diabetes unless the person is prescribed insulin, there is evidence of hypoglycaemic episodes, the person is on oral medication that may increase their risk of hypoglycaemia while driving or operating machinery, the person is pregnant or is planning to become pregnant.
Action required by NHS boards/clusters/practices:
- SMG should be prescribed in line with local MCN guidance and formulary recommendations. There is no evidence to suggest greater clinical benefit is achieved by using more expensive test strips over the less costly ones and therefore NHS Boards should select appropriate formulary products.
- GP Clusters and practices should review their data with others in the board and down to practice level, considering practices with higher level of SMG prescribing.
- Identify individuals prescribed SMG and review to ensure if ongoing use is required.
Number of people aged ≥ 75 years prescribed sulfonylureas as a percentage of all people aged ≥ 75 years prescribed an anti-diabetic drug (see Section 9).
This current indicator continues to show that there are high levels of SU prescribing in those aged 75 years or over.
A low percentage in this indicator would indicate alignment with current best practice prescribing guidance.
Although this has reduced, most recent data shows that across Scotland there is a significant proportion over those aged 75 years or over are still being prescribed an SU, increasing their risks of hypo glycaemia and subsequent falls and hospitalisation.
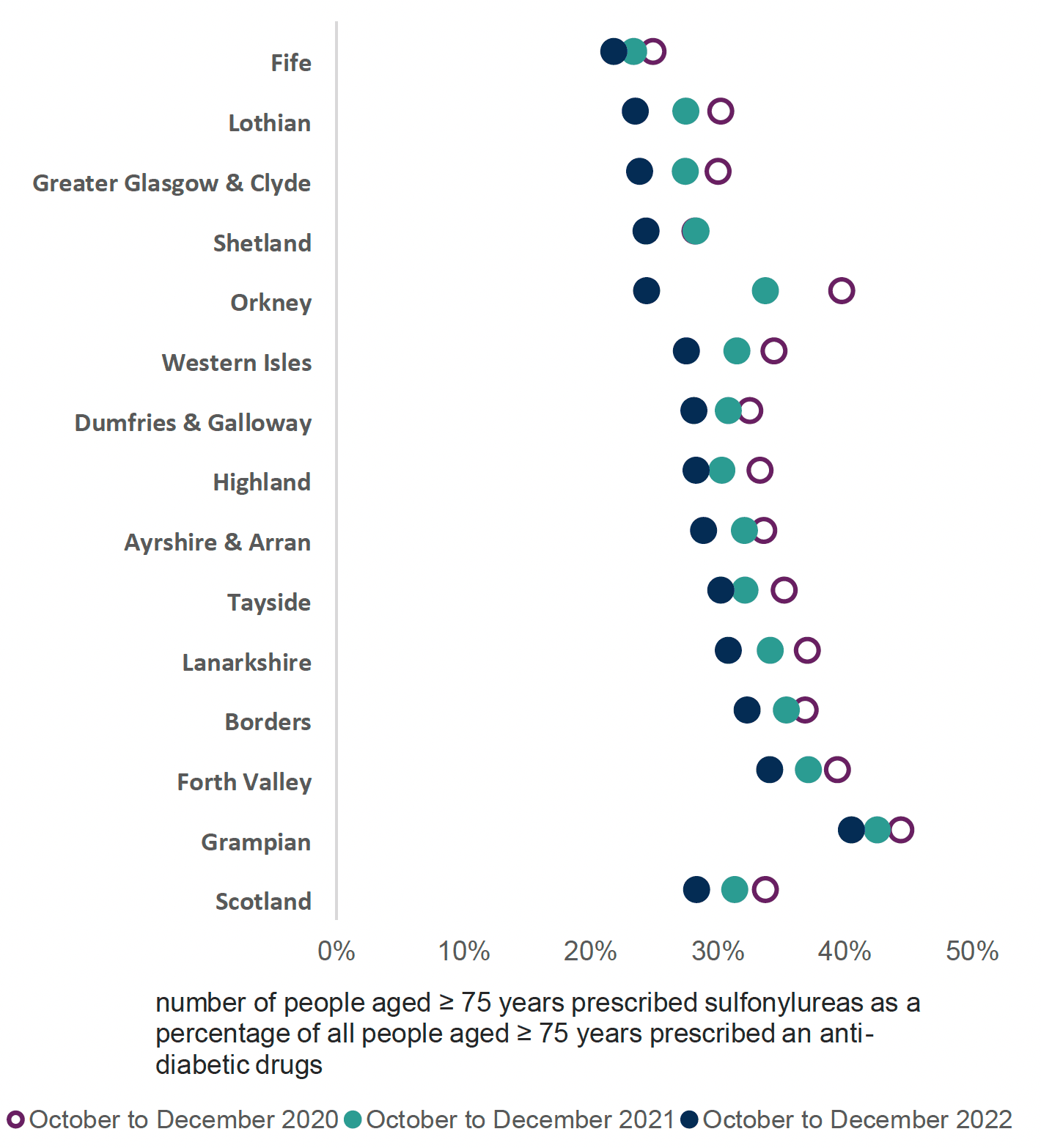
Action required by NHS boards/clusters/practices:
- GP Clusters and practices can review their data in comparison to other board regions to determine areas of unwarranted variation.
- GP Clusters and practices can review their data with others in the board down to individual practice level, considering practices with higher percentage of SU prescribing and why these may be outliers in prescribing.
- Other therapies are available with long term outcome data and lower risk of hypoglycaemia that may be more appropriate.
Contact
Email: EPandT@gov.scot
There is a problem
Thanks for your feedback