Older adults' mental health before and during the COVID-19 pandemic: Evidence paper
Evidence review of older adults’ mental health in Scotland and the access to and delivery of older adults’ mental health services.
Older adults’ mental health
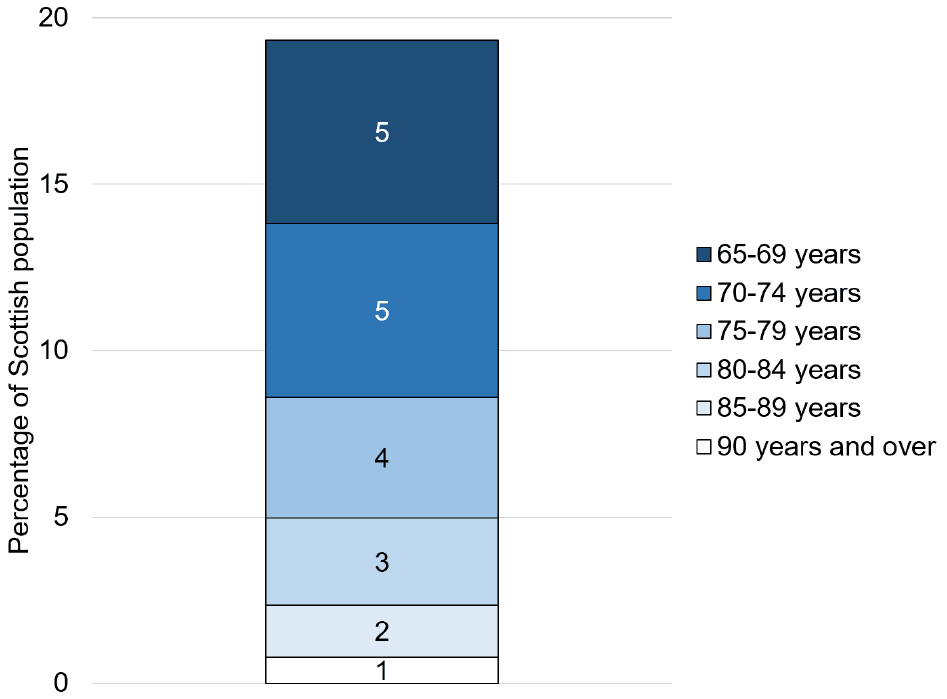
This section focuses on findings related to older adults’ mental health. Evidence presented in this section has defined and grouped older adults differently. Figure 1 presents National Records of Scotland data[16] concerning the proportion of older adults in Scotland in 2020 in narrower age ranges. The proportion of older adults within each age range decreases as age increases. For example, there are a smaller proportion of older adults aged 90 years and over (1%) than 65 to 69 years (5%)
Compared with other age groups
This section presents evidence that makes comparisons between older adults and other age groups (e.g., adults aged 18-64), and comparisons between older adults of different ages (e.g., 65-69, 70-74, 75+). These comparisons of mental health are presented in relation to the following: mental wellbeing and related aspects of mental health (e.g., life satisfaction, happiness, optimism); loneliness; mental ill-health, anxiety and depression; and suicidal thoughts and attempts, and incidences of self-harm. Evidence collected before and during the COVID-19 pandemic is presented in this section. However, as this section focuses on comparisons on the basis of age, no evidence is presented regarding comparisons across time, which is the focus of the next section.
Mental wellbeing
Survey-based evidence appears to show that older adults consistently report better mental wellbeing (and related factors, such as life satisfaction and happiness) than younger adults:
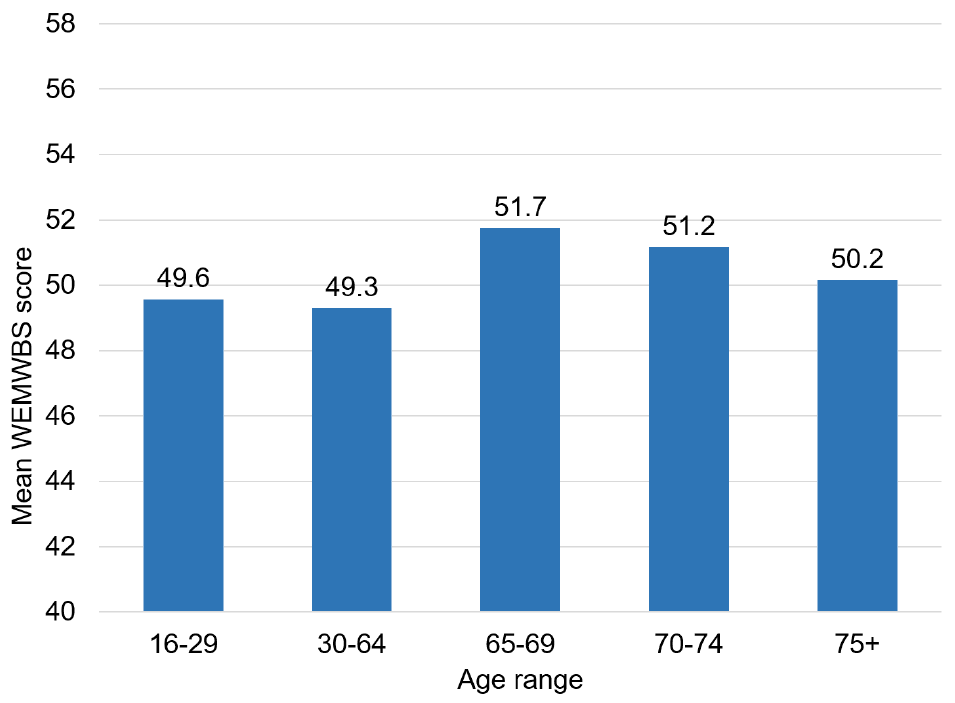
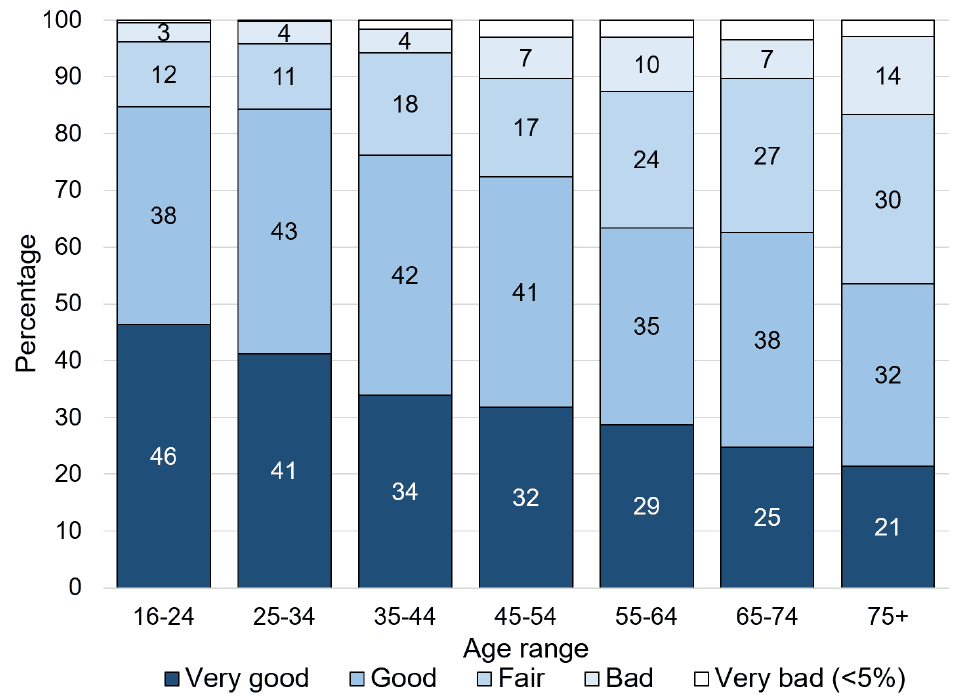
- Analysis of SHeS 2016-2019 data indicated that older adults aged between 65 and 74 years old reported the highest mental wellbeing of all age groups (Figure 2).
- The SHeS telephone survey conducted between August and September 2020[17] reported similar findings – older adults aged between 65 and 74 years reported higher mental wellbeing compared with adults aged between 16 and 64.
- In each of the first four survey waves of the Scottish COVID-19 Mental Health Tracker study (conducted at several points during the pandemic) [18] older adults (defined as 60+) reported better mental wellbeing (assessed by the short version of WEMWBS) than adults aged between 18 and 59.
- A Scottish Government survey conducted at several points during the pandemic[19] found that a higher proportion of adults aged 55-69 and 70+ reported being ‘completely happy’ in Spring 2020 than younger adult age groups (e.g., 35-54). Similarly, in Spring 2021, adults aged 55+ reported higher levels of happiness than younger adults.
- A survey conducted for The Scottish Wellbeing Index report published in November 2021[20] found that, on average, adults aged 65+ reported a higher mental wellbeing than younger age groups (e.g., 55-64). The same pattern of results was also found for specific aspects of wellbeing: life satisfaction, feelings of worth, and happiness.
- Findings from a 2017 survey by researchers at the University of Dundee[21] found that higher life satisfaction was reported by adults aged 65+ compared with those aged 50 to 64.
The previous findings concern fairly broad age ranges, such as older adults being defined as anyone 65+. However, these broader age ranges might conceal differences between, for example, older adults aged 65-69, and those aged 70-74.
Findings comparing mental wellbeing across narrower age ranges are less consistent than those based on broad age ranges:
- The following research suggests that older adults experience poorer mental wellbeing as their age increases:
- In contrast to the previous findings, the following studies suggested that older adults’ mental wellbeing improves (or is similar) with increasing age:
Loneliness
Compared with younger adults, older adults appeared to report better or similar outcomes in relation to loneliness[28]:
- Across the first four waves of the Scottish COVID Mental Health Tracker study[29], older adults (defined in the study as 60+) reported feeling less lonely than younger adults.
- Scottish Government survey-based research conducted during the pandemic[30] found that similar proportions of older adults (70+) reported experiencing at least some loneliness compared with adults aged 35 to 54, and 55 to 69.
When comparing older adults in narrower age groupings (e.g., in their 60s, 70s, 80s), findings suggest a higher likelihood of experiencing loneliness with increasing age in older adulthood:
- The Scottish Household Survey 2018[32] found that a larger proportion of older adults aged 75+ reported experiencing at least some loneliness in the previous week compared with adults aged 60-74 (26% and 18%, respectively).
- At different points during the pandemic, two surveys of Generation Scotland participants[33] found that a higher proportion of participants aged 80+ experienced some loneliness in the previous week compared with participants in their 70s.
Mental ill-health, anxiety and depression
When compared with younger adults, research evidence tends to indicate that older adults are less likely to report poor mental health, or report better average mental health (e.g., possible psychiatric disorder, anxiety, depression):
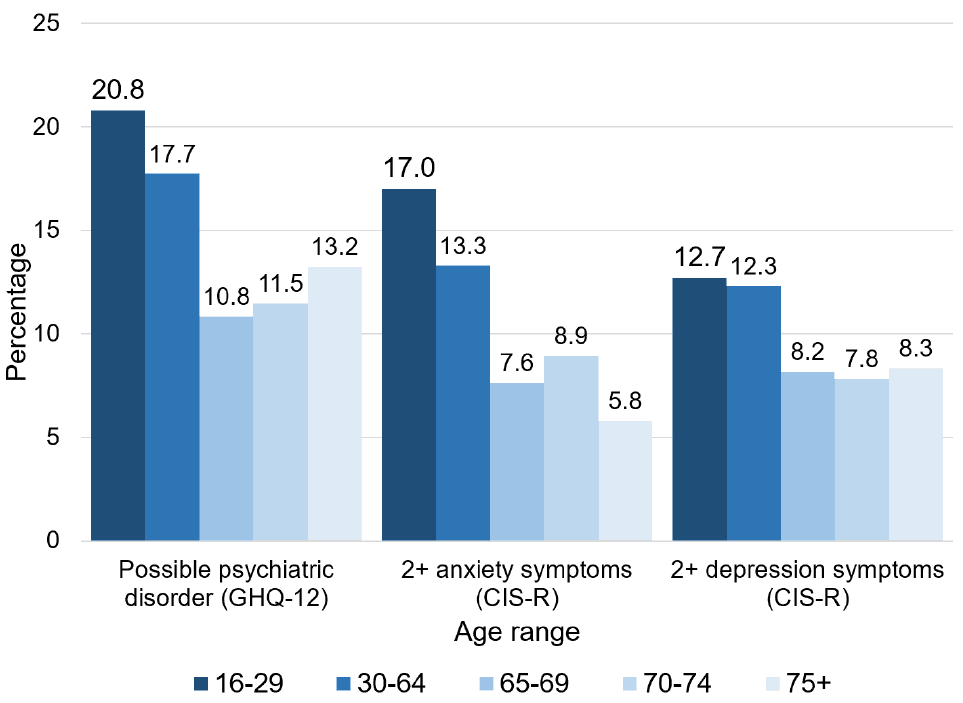
- The SHeS 2016-2019 analyses data found that older adults were less likely than younger adults to meet the threshold for a possible psychiatric disorder (i.e., 4+ psychiatric symptoms; Figure 3). For anxiety, older adults aged 65-69 and 75+ were less likely to indicate two or more symptoms than younger adults. However, older adults aged 70-74 were less likely to report two or more anxiety symptoms than those aged 16-29, but were similar to those aged 30-64. For depression, older and younger adults were similarly likely to report two or more symptoms.
- The same pattern of results for possible psychiatric disorder and anxiety were reported for analyses of the SHeS telephone survey conducted between August and September 2020[34]. However, no significant differences were reported in the rates of depression across the different age ranges.
- Similarly, in each of the first four waves of the Scottish COVID Mental Health Tracker study[35] a smaller proportion of older adults (defined as 60+ in the study) indicated a potential psychiatric disorder or moderate to severe anxiety or depression symptoms compared with younger adults.
- In the CovidLife survey of Generation Scotland participants,[36] those in their 60s, 70s and 80+ appeared less likely to report (mild to severe) depression than those in younger age groups.
- In Spring 2020, a survey conducted by researchers at Glasgow Caledonian University[37] found that older adults aged 65+ were the age group least likely to indicate anxiety, depression and post-traumatic stress disorder.
- Supporting information from an analysis of UK Household Longitudinal Study data[38] indicated that older adults reported better mental health on average than younger participants at six points between 2017 and 2020.
- A 2017 survey by researchers at the University of Dundee[39] found that older adults reported lower depression scores on average than adults aged 50-64, although no differences were found with regard to anxiety.
- Through a survey with a sample representative of the Scottish population, researchers at the University of Aberdeen found that older participants were less likely to indicate anxiety or depression from their survey responses than younger participants[40].
With regard to possible psychiatric disorder, anxiety and depression, the findings from comparisons of older adults in narrower age groupings (e.g., in their 60s, 70s, 80s) are inconsistent:
- The SHeS 2016-2019 analyses found that similar proportions of the three older adult age groups (65 to 69, 70 to 74, 75+) indicated a possible psychiatric disorder, or two or more anxiety or depression symptoms (Figure 3). Similarly, the SHeS telephone survey conducted in 2020[42] found that similar proportions of older adults aged 65-74 and 75+ met the threshold for a potential psychiatric disorder (13% and 15%, respectively).
- The longitudinal study of the Lothian Birth Cohort 1921[43] found that participants reported higher levels of depression, but lower levels of anxiety at 90 than they did at 79.
- The CovidLife survey[44] indicated that a larger proportion of older adults aged 80+ reported experiencing depression than those in their 70s. In contrast, fewer participants reported experiencing anxiety as age increased.
- Scottish Government survey-based research conducted during the pandemic[45] found that a higher proportion (20%) of older adults aged 70+ reported high levels of anxiety compared with those aged 55 to 69 (20% and 17%, respectively).
Suicide and self-harm
Statistics published by the National Records of Scotland indicate that 12% (98) of probable suicides in Scotland in 2020 were completed by older adults (65+)[46]. As older adults comprised 19% of Scotland’s population in 2020, this statistic suggests that they are less likely to be recorded as dying from suicide than younger age groups.
Survey-based findings indicate that older adults are less likely to report suicide attempts, incidences of self-harm and suicidal thoughts compared with younger adults. Specifically:
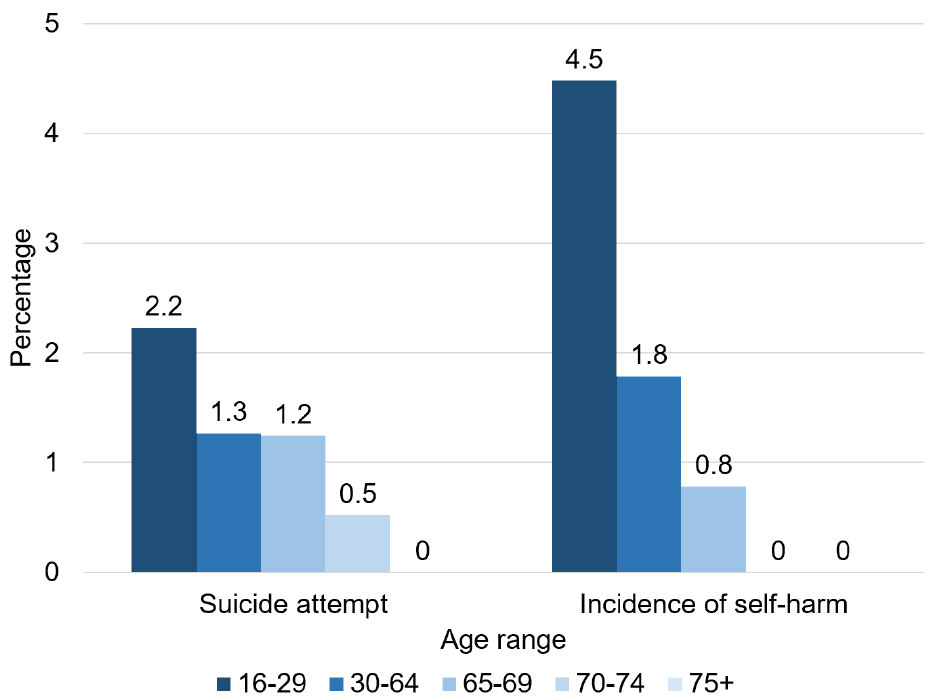
- The analyses of SHeS 2016-2019 data indicated that fewer than 5% of respondents in all age ranges reported a suicide attempt or incidence of self-harm in the year preceding the completion of the survey (Figure 4). No older adults aged 75+ reported a suicide attempt, and no older adults aged 70+ reported an incidence of self-harm. For the age ranges in which at least one person had indicated a suicide attempt (all except 75+), there was a similar prevalence of suicide attempts across all age ranges. However, for the age ranges in which at least one person indicated an incidence of self-harm (16-29, 30-64, 65-69), younger adults aged 16-29 were more likely to report such an incidence than adults aged 65-69.
- Across the first four waves of The Scottish COVID Mental Health Tracker study[47],a smaller proportion (between 2.3% and 3.6%) of older adults (defined as 60+ in the study) reported having suicidal thoughts compared with younger adults.
Before and during the COVID-19 pandemic
The COVID-19 pandemic impacted Scotland’s population in a wide variety of ways[48]. Impacts on the population’s mental health could be for a variety of reasons, such as people experiencing social isolation due to various restrictions, as well as concern about catching the virus. This section appraises the evidence relating to the impact of the COVID-19 pandemic on older adults’ mental health.
Comparing before and during the pandemic
Overall, evidence tends to indicate that older adults report poorer mental health during the pandemic than before. This evidence comes from research that asked older adults before and during the pandemic to report their mental health, and then compared these scores (i.e., longitudinal research), or asked older adults during the pandemic to report their mental health at the time and how they remember it being before the pandemic.
Two longitudinal studies – The Lothian Birth Cohort 1936 study[49] and the UK Household Longitudinal Survey[50] – have compared older adults’ mental health before and during the pandemic. Findings from the UK Household Longitudinal Survey showed that older adults’ mental health (assessed by GHQ-12) was worse during the pandemic compared with before. Similarly, the Lothian Birth Cohort 1936 study found that a smaller proportion of the sample reported ‘excellent’ or ‘very good’ emotional and mental health during the pandemic than before. In contrast, however, the Lothian Birth Cohort 1936 study also assessed changes in mental wellbeing (assessed by WEMWBS) and loneliness, and found no statistically significant differences before and during the pandemic.
In contrast to the findings from the longitudinal Lothian Birth Cohort 1936 study, findings from other studies conducted during the pandemic indicated a negative impact of the pandemic on older adults’ loneliness. Specifically, two surveys – conducted separately by researchers at the University of Stirling[51] and Age Scotland[52] – reported that just over half (54% and 53%, respectively) of their mainly older adult samples reported feeling more lonely during the pandemic compared with before. Similarly, in the COVID Life survey[53], higher proportions of older adults (in their 60s, 70s and 80+) reported feeling lonely during the pandemic than before, with those aged 80+ appearing to indicate the largest proportional increase. In Wave 1 of the Scottish COVID-19 Mental Health Tracker study[54], older adults (60+) also reported an increase in their average level of loneliness during the pandemic (with this increase being larger than for younger adults). These survey findings align with a consultation undertaken by Health and Social Care Alliance[55] (with 29 older adults, and people who work with and support them), in which older adults’ feelings of loneliness were said to have worsened during the pandemic.
Two of the studies conducted during the pandemic – those by the University of Stirling and Age Scotland – also presented findings about the impact of the pandemic on older adults’ experience of anxiety and depression. However, no clear conclusions can be drawn from these findings. While the study by the University of Stirling reported that the majority (61%) of their sample experienced anxiety and depression similarly before and during the pandemic, Age Scotland found that just over half (51%) of their sample indicated that the lockdown in early 2021 made them feel more anxious about the future.
An important consideration regarding the research in this section is that asking people to remember how they felt at some point in the past is likely to be less accurate or more subjective than asking them to indicate how they feel at the time. The overall conclusions should therefore be considered critically but still has the potential for future exploration.
Experiences during the pandemic
Evidence concerning older adults’ mental health during the pandemic (i.e., not making comparisons with before the pandemic) presents a mixed pattern of findings.
In line with an easing of restrictions, researchers at the University of Aberdeen[56] found that the proportions of older adults reporting loneliness and/or depression decreased from June to August 2020. Similarly, findings from the UK Household Longitudinal Survey[57] suggest that older adults’ average level of mental health improved from April to July 2020. In contrast, over a wider period of time, older adults’ (60+) average mental wellbeing was not found to differ over the first four waves – from May/June 2020 to February/March 2021 – of the Scottish COVID-19 Mental Health Tracker study[58].
It is important to note the previous findings are based on samples of older adults, and might conceal individual older adults’ experiences. For example, a participant in the Health and Social Care Alliance’s[59] consultation stated how the various lockdown cycles had had different impacts on their mental health.
Demographic differences
While older adults are often broadly grouped together (e.g., 65+), it is crucial to keep in mind that older adults are not a homogenous group and represent a diversity of experience equal to individuals of other ages. For example, the SHeS 2016-2019 analyses found that, within the broad 65+ grouping, older adults aged 75+ reported poorer mental wellbeing than those aged 65-69 and 70-74. As well as age, older adults’ mental health is likely influenced by a wider range of characteristics (e.g., physical health conditions, ethnic background), which are likely to interconnect and influence each other. This section focuses on different characteristics in turn, and presents evidence on how they influence older adults’ mental health.
Older men and women
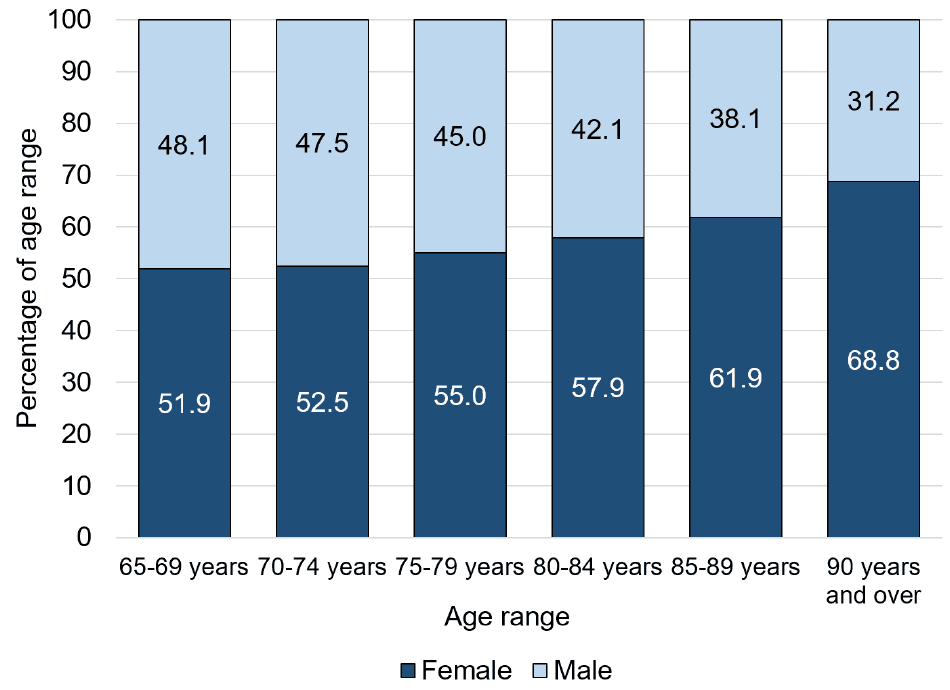
The proportion of older adults who identify as female compared with male increases with age. While female and male older adults each comprise roughly half of those aged between 65 and 69 years, roughly two-thirds of those aged 90 years and over are female (Figure 5)[60].
Data from three nationally representative surveys provide evidence for differences between older men and women relating to mental wellbeing, anxiety and depression symptoms, having a possible psychiatric disorder and suicidal thoughts. Findings from the SHeS 2016-2019 analyses (graphs A to D, Appendix 1), the SHeS survey conducted between August and September 2020[61], and the first four waves of the Scottish COVID-19 Mental Health Tracker study[62], demonstrate that:
- Regarding mental wellbeing and depression symptoms, older men and women appear to be similar. Findings from the three surveys were consistent, with no differences between older men and women being found.
- Regarding anxiety, findings are inconsistent, but suggest older men might be more at risk. While the two SHeS analyses found no differences regarding anxiety, at waves 3 and 4 of the Mental Health Tracker study, older women were found to be less likely to report anxiety.
- Regarding possible psychiatric disorder, findings are inconsistent, but suggest older women might be more at risk: The SHeS 2016-2019 analyses indicated that a higher proportion of older women than men aged 65-69 indicated a possible psychiatric disorder, but there were no differences for the other age ranges. Similarly, older women (60+) were found to be more likely to indicate a possible psychiatric disorder at waves 3 and 4 of the Mental Health Tracker study. In contrast, no differences between older men and women were identified through the analyses of the SHeS survey conducted between August and September 2020.
- Findings are limited regarding suicidal thoughts, but suggest that older men might be more at risk. In line with roughly two-thirds of people aged 65+ who died by probable suicide being male[63], the Mental Health Tracker study reported that older men (60+) were more likely to report suicidal thoughts than an older women. Neither of the SHeS analyses assessed suicidal thoughts.
Findings concerning loneliness are mixed and it is unclear whether older women and men differ in terms of the likelihood of experiencing loneliness. However, differences in the level of loneliness (e.g., mild, moderate) are slightly better supported by evidence and suggest that older women experience a higher level than older men. The specific evidence for these findings is presented below:
- The Scottish COVID-19 Mental Health Tracker study[64] did not find any differences between older men and women (60+) in terms of loneliness (at any of the four waves). In contrast, the following studies suggested differences in experiences of loneliness between older men and women:
- An NHS survey of older adults in the Highlands conducted before the pandemic found that a higher proportion of older men (70%) than older women (63%) reported feeling lonely, although more older women than men reported feeling ‘intense’ loneliness (9% and 7%, respectively)[65].
- In Age Scotland’s Big Survey, conducted during the pandemic, 29% of older women reported never feeling lonely, compared with 41% of older men[66]. This survey also found that more older women (58%) than men (42%) felt that the pandemic and associated restrictions had made them feel lonelier, which was in line with similar insights provided by older women participating in a consultation conducted by the Scottish Women’s Convention.
- Similarly, older women were found to report higher loneliness on average in a survey conducted by researchers from The University of Stirling during the pandemic[67].
A common insight in feedback from stakeholders for this review was that older women’s mental health is not seen as a sufficiently serious issue[68]. Indeed, the limited evidence identified for inclusion in this section highlights the lack of focus on older women’s (as well as older men’s) mental health. While it is difficult to draw strong conclusions about differences between older men and women based on this evidence, tentative findings suggest that older women might be more at risk of some mental health outcomes (i.e., possible psychiatric disorder, loneliness), and less at risk of others (i.e., anxiety, suicidal thoughts and death by suicide). However, these findings should be viewed critically due to the limited evidence.
LGBTI+ People
A large evidence gap in this report concerns the mental health of older adults who identify as LGBTI+ as no evidence could be identified concerning these older adults throughout the pandemic. Related to this gap, due to insufficient sample sizes , no SHeS 2016-2019 analyses could be conducted on the basis of sexual orientation.
Insights provided through our consultations with stakeholders in the Mental Health Equalities and Human Rights Forum (EHRF)[69] highlight several specific experiences that older LGBTI adults are likely to have had throughout their life that might negatively impact on their previous and current mental health. Examples include lack of acceptance, marginalisation, and prejudice (e.g., from family and society), discrimination (e.g., in employment, health and social care, being historically banned from military service), criminalisation, pathologisation (e.g., sexual orientations and trans status being considered as a mental illness), living through the AIDS epidemic, and participation in unwanted therapies (e.g., psychiatric[70], conversion practices or so called ‘conversion therapy’) and subsequently minority stress.
Related to these examples, the stakeholders also stressed how isolation in older LGBTI adults was being a key issue. Reasons given for this included people possibly choosing to conceal their identities when forming new social connections, losing friends and family through coming out, feeling “ignored” by younger LGBTI people, and LGBTI spaces in which they could be open about their true identity closing during the pandemic. Bereavement also likely has specific complexities for older LGBTI adults, particularly for those who are not out and lose a primary partner, as they might experience less recognition from others of their loss, and a reduced connection with their LGBTI identity. Last, the COVID-19 pandemic might have raised a particular challenge for older LGBTI adults by triggering past traumas associated with the AIDS epidemic.
Ethnic and religious background
Another large evidence gap in this report concerns how older adults’ mental health varies across different ethnic and religious backgrounds. As with evidence for LGBTI older adults, SHeS 2016-2019 analyses could not be conducted on the due to insufficient sample sizes, and no evidence could be identified that investigated older adults’ mental health in relation to these characteristics.
Physical health conditions and sensory impairments
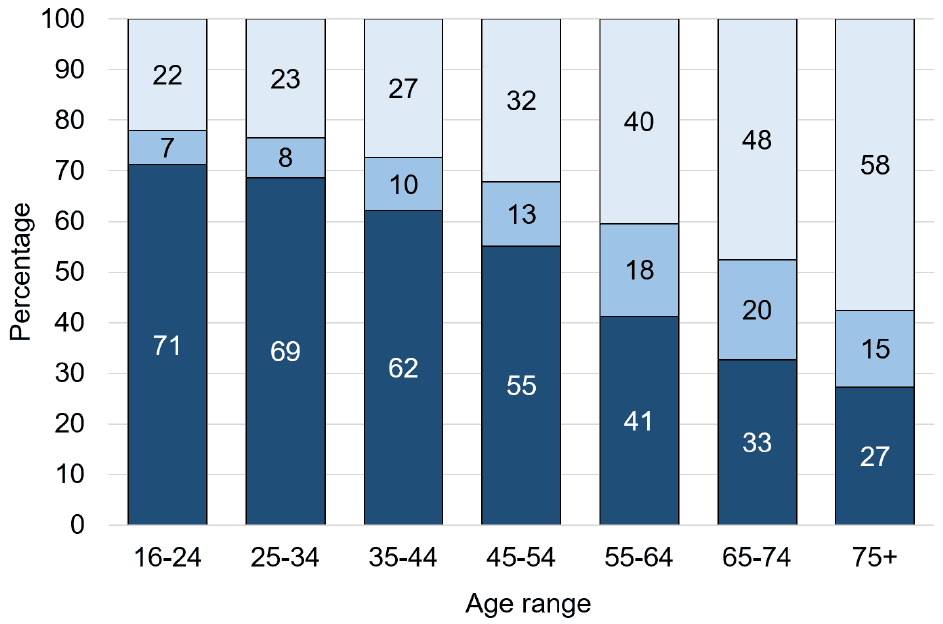
Physical health deteriorates over the lifespan, both in terms of self-assessed general health (Figure 6), and the prevalence of limiting and non-limiting long-term health conditions (Figure 7)[71]. Regarding COVID-19, older adults are also at greater risk of mortality from the virus[72], and, accordingly, perceived catching the virus to be more serious for themselves than for younger adults[73]. As such, the impact of physical health issues on mental health likely becomes increasingly important as age increases.
Overall, older adults with a physical health condition, or who have poor general health, tend to have poorer mental health outcomes than those without such health issues. The evidence is consistent for some mental health outcomes (mental wellbeing, having a possible psychiatric disorder and loneliness), but less clear for other outcomes (anxiety and depression symptoms). Specifically:
- Regarding mental wellbeing:
- Regarding having a possible psychiatric disorder:
- Regarding anxiety symptoms:
- Regarding depression symptoms:
- Regarding loneliness:
- In addition to physical health issues, sensory impairments also appear to be associated with poorer mental health outcomes for older adults. Specifically:
Isolation
Evidence concerning different types of isolation was identified. Specifically, whether or not older adults have regular contact with others, live with other people, or live in rural or urban areas. Overall, evidence was mixed across these types of isolation, although more consistent findings included older adults living alone reporting poorer mental wellbeing and a higher likelihood of experiencing loneliness than those living with others).
Older adults are suggested to be at particular risk of experiencing social isolation and not having regular contact with others. Before the pandemic, such isolation was suggested to be prevalent for several reasons including: experiences of mental health stigma and discrimination in earlier adulthood increasing social isolation over time[83]; bereavement for family and friends, resulting in smaller social networks[84]; and a lack of access and/or ability to use digital communications[85].
Older adults’ risk of isolation likely increased during the COVID-19 pandemic, with 68% of Age Scotland’s Big Survey 2021[86] sample reporting difficulty accessing friends and family – 24% did not see anyone else during a typical week and only 21% saw someone every day. Added to which, many older adults were advised to or chose to minimise in-person contact during the pandemic. Roughly 9% of Scotland’s older adult population (91,463) was asked to shield in June 2020, and an estimated 45-50% of adults aged 60+ choose to shield despite not being asked to do so[87]. Furthermore, restrictions on visitations to care homes might have isolated some older adults living in residential care from family and friends[88], even if they were not on a shielding list or did not choose to shield. The increased reliance on digital communications also likely impacted older adults’ contact with others.
In a survey conducted before the pandemic, the Mental Health Foundation found that 80% of older adults reported that spending time with family and friends in-person improves their mental health, in comparison with 50% who indicated that it improves with time alone[89]. This finding is in line with results from the COVID-19 Shielding Programme (Scotland) Impact and Experience Survey, which found that 64% of older adults who were asked to shield reported a negative impact of shielding on their mental health. Relatedly, a survey of older adults conducted during the pandemic by researchers at the University of Stirling found that less social contact was associated with feelings of loneliness[90]. An insight from a 76-year old participant in this survey reflects this finding, as they expressed feeling the loss of their spouse “more acutely as [they had] no overnight stays from grandchildren or visits from family and friends”. However, the COVID-19 Shielding Programme (Scotland) Impact and Experience Survey found that older adults aged 75-79 and 80+ were less likely to report a negative impact of shielding on their mental health (56% and 60%, respectively) than those aged 65-69 and 70-74 (70% and 63%, respectively). Such a finding might indicate that ‘older’ older adults were more socially isolated before the pandemic, and so the restrictions might not have had as large an impact.
The evidence was more mixed in relation to older adults’ mental health outcomes depending on whether or not they live alone. Specifically:
- Older adults who live alone indicated poorer mental wellbeing and a higher likelihood of experiencing loneliness:
- Evidence concerning mental ill health, anxiety and depression was more mixed:
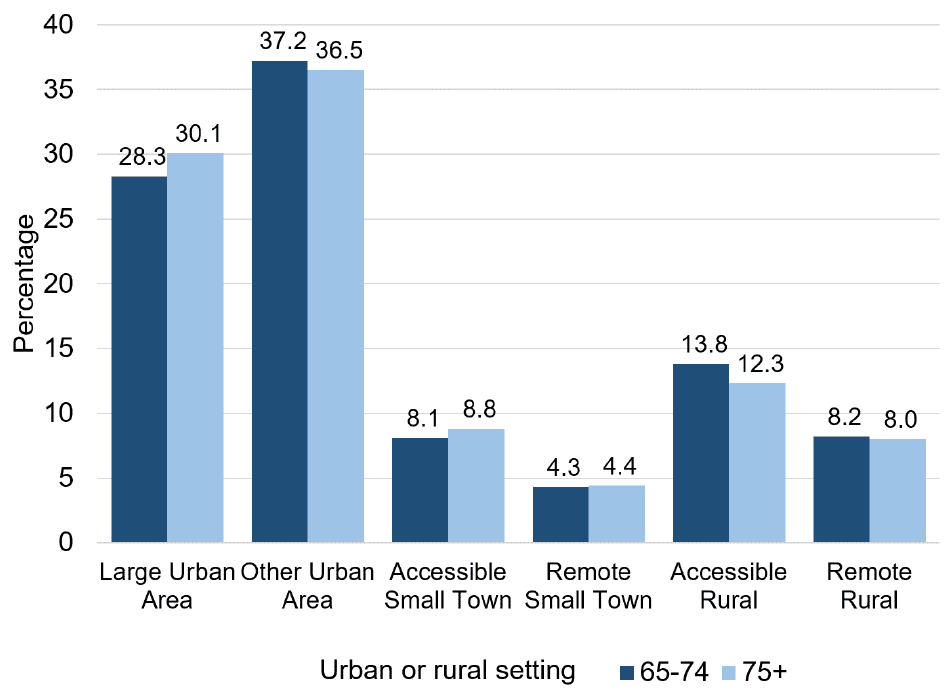
Concerning living in rural or urban settings, roughly two thirds of older adults report living in urban areas, with this being similar for those aged 65 to 74, and 75+ (Figure 8)[96]. Over 10% of older adults live in remote locations. Additionally, 39% of households in remote rural areas are older adults (living alone or with another older adults) compared with 33% of accessible rural areas[97].
The evidence was also mixed in relation to older adults’ mental health outcomes depending on whether they lived in rural or urban settings:
- The SHeS 2016-2019 analyses found that:
- Before the pandemic, a survey of older adults in the Highlands[98] found that:
Caring responsibilities
Combined data from several representative surveys indicates that roughly 17% of older adults aged 65-74 provide unpaid care, compared with 12% of those aged 75+[99]. However, little evidence was identified that compared the mental health of those with and without such responsibilities. The SHeS 2016-2019 analyses were able to investigate this, but those with and without such caring responsibilities were found to be similar in terms of mental wellbeing, having a possible psychiatric disorder, and experiencing anxiety or depression symptoms (graphs A to D, Appendix 6).
Regarding loneliness, a survey of older adults in the Highlands conducted before the pandemic[100] found that a larger proportion (79%) of older adults providing 20+ hours of care reported feeling lonely, compared with those providing fewer hours of care (between 58% and 65%). This finding is in line with the insight that loneliness results from older adults’ caring responsibilities, which was found through a consultation with older adults[101], and open-response questions on a survey conducted by researchers at the University of Stirling[102]. Consultations also suggested that a lack of respite from caring responsibilities during the pandemic impacted older adults’ mental health, and that caring responsibilities were seen as more likely to fall to women rather than men[103].
Finances and deprivation
Little evidence was identified that investigated how older adults’ mental health varies in relation to finances and deprivation. In terms of mental wellbeing, the SHeS 2016-2019 analyses found that older adults with lower (compared with higher) incomes, and who experienced higher (compared with lower) deprivation reported poorer mental wellbeing (Graphs A, Appendices 7 and 8). However, no differences between older adults on the basis of income or deprivation were found regarding the likelihood of indicating a possible psychiatric disorder, except more deprived older adults aged 65-69 being more likely to indicate a possible disorder. Regarding loneliness, similar levels of loneliness were reported by adults living across the SIMD quintiles in an NHS survey of older adults in the Highlands conducted before the pandemic[104].
Contact
Email: socialresearch@gov.scot
There is a problem
Thanks for your feedback