Distress Brief Intervention pilot programme: evaluation
This report presents a realist evaluation of the Distress Brief Intervention (DBI) programme. DBI has been successful in offering support to those in distress, and has contributed to peoples’ ability to manage and reduce their distress in the short term, and for some in the longer term.
6 Delivery of DBI
In this section, we present data on the delivery of DBI at Level 1 and Level 2, variations in the delivery of DBI across pilot sites, the staffing and cost implications of delivering DBI Level 2 interventions, how individuals who received DBI accessed further and future support, and the importance of the role and activities undertaken by DBI Central.
6.1 Delivery of DBI Level 1
6.1.1 Variations in implementation and delivery of DBI Level 1
Overall, DBI Level 1 was implemented with incremental roll-out across frontline service as intended. Across the pilot sites, the frontline services were engaged to differing degrees, reflecting local contexts and relationships. There was considerable variation in the delivery of DBI Level 1, much of which was related to the wide range of services involved and their role in delivering frontline care. DBI was successfully adapted to different contexts.
Some DBI staff, at different levels and in different pilot areas, became so involved that they acted as champions for the intervention. In doing so they promoted DBI and overcame implementation challenges both within and between organisations. These champions oversaw the feedback loops between Level 1 and Level 2 to ensure that awareness of appropriate DBI referrals was increased. Champions also acted as role models within services, embodying the DBI principles of compassion in their work and allowing the benefits of DBI to be seen by others. Feedback on the continued success of implementing the 24-hour contact requirement at Level 2 increased trust in the programme and confidence among Level 1 practitioners that they were offering a compassionate and effective response to individuals in distress. This supported the implementation of DBI and reduced concern among Level 1 practitioners regarding their accountability for the wellbeing and safety of people who presented in distress.
Where Level 1 practitioners doubted the added value of DBI, this acted as a key barrier to implementation. A few Level 1 practitioners working in frontline services perceived DBI as a threat to services that were already operating and which they considered to be of greater use and expressed concern that DBI would replace these. Level 1 practitioners in frontline services who considered addressing mental health issues to be outwith their role were also more reluctant to adopt the programme.
In frontline services where DBI was perceived as an additional task, this appeared to pose a barrier to its use. For example, for police officers, making a DBI referral meant that the person also had to be entered into the Vulnerable Persons Database. Before the introduction of DBI, this person would not automatically have been entered into the Vulnerable Persons Database, meaning that DBI had created additional processes for some frontline services.
"She'd been having ongoing issues with her husband etc. and other members of the family and she appeared quite distressed. Now I wasn't concerned by her situation but she was distressed so I offered her a DBI but then I also had to submit a VPD [Vulnerable Persons Database entry]. Now I had no concern for her or her wellbeing in the environment she was in but I could see that she probably wanted to speak to somebody that was out of the family situation. So it's kind of I was doing a VPD just because it's supposed to be done." Level 1 practitioner, Police Scotland
6.1.2 Provision of a compassionate, constructive and effective response at DBI Level 1
Both those working in frontline services and individuals who received support from DBI described the DBI Level 1 response as compassionate and effective.
Overall Level 1 practitioners reported feeling empowered by DBI to offer a more compassionate and constructive response. They recognised that they had always aimed to be compassionate, but had felt constrained by an inability to offer distressed individuals they encountered any tangible support. The ability to offer a practical and timely solution was perceived as being of benefit to many of the individuals presenting to frontline services, but also offered Level 1 practitioners comfort and reduced some of the frustration previously felt with the lack of options.
"It still allows us to put something in place with that and it gives you a bit a nicer feeling that I'm not just abandoning that person to, you know, just some immediate treatment." Level 1 practitioner, Scottish Ambulance Service
When asked to rate their agreement with statements on the impact of the DBI pilot on frontline services overall, the majority of Level 1 practitioners survey respondents (86%) agreed that DBI provided a more efficient way for their services to respond to people in distress (with 57% strongly agreeing) (Appendix 4). However, frontline Level 1 staff did recognise the limitations of the DBI service and some interviewees doubted DBI's effectiveness in reducing the number of calls to attend people who frequently used their service and who were often perceived to present with more severe and enduring mental health conditions.
Individuals who accessed support from DBI also reported experiencing a compassionate response at Level 1, with some variation in perceived compassion by Level 1 referrer.
6.1.3 Referral to Level 2
Individuals who were deemed suitable for a DBI Level 2 intervention were referred by Level 1 practitioners using a specifically developed referral form. Overall, Level 1 practitioners considered DBI referral forms to be relatively straightforward to complete, adding few additional processes to existing work. However, the paper or telephone referral process to Level 2 created an additional step that did not always fit well with frontline services' existing procedures. For some, notably the Scottish Ambulance Service, this created a barrier to making referrals. A specific referral challenge was the submission of incomplete referral forms. This appeared to be a particular issue if the referring individual had not undergone DBI Level 1 training (in theory only people who were trained in DBI Level 1 could refer to a Level 2 service, but our data suggests this was not always the case in practice). DBI Level 2 practitioners reported that referrals from Police Scotland were often the most detailed and complete.
It is important for future roll-out that new areas implementing DBI ensure they can capitalise on existing local systems and networks to allow a faster and/or more effective referral process. This may have a resource implication for planning stages to identify which systems are in place and any additional software or personnel time required to streamline the referral process.
Where multiple services were involved, issues occasionally arose regarding whose responsibility it was to make the referral to DBI Level 2. This was resolved by allowing the service with the most straightforward referral process to make the referral. On other occasions, Level 1 practitioners reported that the same individual may be referred by more than one service. This did not appear to cause a significant issue for the Level 2 service.
"If the police and ambulance go out and attend to an incident, and decide that, no they don't need to bring them to ED [Emergency Department]. But if there are some things that this person could do with some help with, they will themselves make a referral. We have had situations where, the police have made a referral, actually, where the patients come to ED … and we've made a referral." Level 1 practitioner, Mental Health Crisis Team
Where local changes to systems and networks were possible, these enabled the referral process to work well. In one area, local protocols were developed that involved use of a local 'hub' used by all local emergency services, which enabled the Scottish Ambulance Service to call immediately and securely pass on an individual DBI Level 2 referral. This allowed a more efficient referral process from Level 1 to Level 2 for the Scottish Ambulance Service in this area. Other pilot areas did not develop similar local protocols and in these areas the Scottish Ambulance Service Level 1 practitioners found the referral process to be more challenging.
Individuals who accessed DBI generally found the referral process straightforward, although their initial awareness of the support they would be offered in Level 2 varied between frontline services. Individuals referred from GPs usually clearly understood the purpose of the DBI Level 2 referral and, frequently, the immediacy of the Level 2 contact was met with surprise and welcomed. Individuals referred to DBI Level 2 from emergency services were often less clear about the reasons for their referral - and the role that a DBI service could have was less well understood. These individuals appeared to have less understanding of DBI and the referral process. This appeared to impact on individuals' ongoing engagement with DBI. In some cases, this challenge was addressed by frontline staff leaving personalised written information with an individual describing which services had been involved in the crisis situation and why the referral to DBI had been made. This appeared to result in improved engagement with the service and distress reduction during the DBI Level 2 intervention.
"The GP explained it very clearly and said that somebody would call me about it within the next 24 hours, and they did call I think within…I think they called that afternoon actually so it was just about…maybe about four hours later they called and then arranged the first appointment. I can't remember the timescale, but it was very quick." Individual
In the early stages of the project, feedback from DBI Level 2 services that some referrals were inappropriate may have dented the confidence of some Level 1 practitioners. Although they felt that their training had provided them with the basic skills and competencies to make referrals, they were less certain that their referrals were always appropriate in practice. Over the implementation period, the rate of inappropriate referrals seems to have fallen. Level 1 practitioners reported receiving constructive feedback and support from Level 2 practitioners that helped them identify individuals who were unsuitable for DBI. Some Level 1 practitioners suggested that they became more selective about referrals over time, as they valued the service and wished it to be as effective as possible to allow it to continue. The most notable increase in referrals was from GPs. DBI Level 2 practitioners stated that this may be due to DBI providing an additional pathway to prevent patients' problems from developing into a crisis level that required emergency service intervention.
"One of the biggest inputs we now have are from GPs, those are the ones that we went out and developed and spoke to practices and brought them on, and if anything the quality of the referrals from the GP is higher." Level 2 practitioner
6.2 Delivery of DBI Level 2
6.2.1 Variations in implementation and delivery of DBI Level 2
The core elements of DBI Level 2, namely contact within 24 hours, a supportive first contact, the offer of up to 14 consecutive days of person-centred support and completion of a D-MaP, were implemented as intended across pilot sites and third-sector partners.
While the core elements were adhered to, Level 2 staff felt that the flexibility allowed in implementing DBI was a strength. This also allowed Level 2 practitioners to go above and beyond the basic process to optimise the service offered, where possible.
"It's a real strength that the openness allows for the character of the person who is doing a particular delivery to be part of that and therefore for it to be a more authentic intervention. That's a really good thing because so many manualised approaches which are deemed to be low intensity now are manualised within an inch of their lives and they are not…they don't allow for the authentic inclusion of the person who is doing the delivery." Level 2 practitioner
Adaptations have largely been led by a focus on delivering a person-centred approach. Some Level 2 practitioners noted, however, that adaptations based on feedback from one area may not be appropriate to other areas where existing processes worked well. This might suggest that a menu of options should be made available, allowing areas to pick and choose which adaptations might be suitable to their context.
"Some of the stuff that other teams have suggested aren't going to work for us, for example. Again, different areas, different geographical places we're covering and things like that – just different people in general, i.e. talking about service users and things – they're just not going to work for us. So I think implementing a change across the board isn't going to work for everybody." Level 2 practitioner
The key variations in the implementation of DBI Level 2 were identified as initial contact with individuals following referral, length and intensity of support and the settings in which Level 2 was delivered. These are discussed in more detail below.
6.3 Contact with individuals following referral
6.3.1 Contact within 24 hours
One of the core elements that was consistently executed in accordance with the DBI implementation plan was the commitment for Level 2 practitioners to attempt to contact the referred individual within 24 hours. As shown in Section 4.4, this was achieved for all referrals, and successful contact was made within 24 hours in 65% of referrals. Largely achieving this has surprised some frontline services and individuals and contributed to building their trust in DBI as a service.
"The fact that they do exactly what they say they do on the tin. Because I think, you do, you can stick in a referral at ten o'clock at night, and the next morning they're phoning up saying, oh we've got more information about that person, and we're just about to go and see them, and you think, blooming hell. It's excellent, it's really excellent." Level 1 practitioner, Police Scotland
"Because when you are feeling that low, that you are considering, obviously, taking your own life, and you get told, oh well, we can see you in 12 weeks' time, it feels like you're not really valued. It feels like you're sort of just being given a number and being told, oh we'll see you when we can. But it felt really personal, and the fact that it felt like they were actually wanting to help get you out of that stage." Individual
Level 2 providers had protocols in place for making the first contact with individuals within 24 hours. However, the success of these could be affected by the availability of the individual, particularly if drugs or alcohol issues affected their recall of being referred to DBI, or if they were in hospital overnight. Some Level 2 providers mentioned the benefit of adapting to processes that worked better for individuals, such as not making contact before 10am, as individuals had often been in hospital through much of the night:
"We now don't phone anybody before ten o'clock, only because a lot of people could have been in hospital until one o'clock the previous night or the previous morning and then phoning them at nine o'clock is a wee bit early…" Level 2 practitioner
The majority of individuals who completed the first session DBI Level 2 individual impact survey (See Section 3.2.1) (79%) were contacted by the Level 2 provider within 24 hours of referral. Nearly all respondents to the second session survey (See Section 3.2.1) (97%) thought that contact within 24 hours from the Level 2 intervention provider was just about right. Level 2 practitioners felt that delays in follow-up after the initial contact had an adverse effect on the person in distress. However, this was not borne out by the individual-level survey data. Whether contact was made within 24 hours appeared to make no difference to the reduction in distress levels over the time of the Level 2 intervention, with similar outcomes for those who were contacted within 24 hours and those who were not (Appendix 3, Table A6.1).[8]
Individuals recognised that a prompt follow-up to the first contact could make a positive difference to engagement:
"That was so hard, that was literally, like, cause I was there first thing on Friday morning so the whole of Friday night, Saturday and Sunday I was just an absolute mess and it's like when I'm feeling like that I get irrational thoughts as well, so I was thinking oh, you know, maybe he's not even referred me and it's like maybe they won't even phone me, am I even going to get help? Yeah, it was a hard weekend, I'm not even going to try and deny that. Come Monday I got the phone call but I was a wee bit disheartened cause it was like they couldn't see me until the following week, the end of the week." Individual
6.3.2 Supportive first contact
The first contact between a DBI Level 2 provider and an individual who had been referred tended to consist of clarifying the reason for the referral and purpose of DBI. This was an important step in managing individuals' expectations, especially regarding the short-term nature of the intervention. Individuals' perceptions of what should be covered at the first contact varied. Some hoped for an opportunity to talk in a counselling-type approach. Others felt that the first was more of an explanation of the service and more detailed talking sessions should follow when a degree of trust in the DBI Level 2 practitioner had been developed. Where the first contact focused on administrative detail, some individuals felt disappointed:
"I kind of felt as if it was going to be like a bit of counselling to kind of help me talk about what I had done and what I had been through and what kind of led me to doing what I had done but it wasn't like that. It was more…the chap that spoke to me was more interested in me filling out forms about…for himself, basically." Individual
As DBI implementation progressed, some Level 2 services appointed administrative support to take the details on initial contact from the Level 1 referrer. This appeared to increase the potential of making contact within 24 hours. However, having administrative support as the first contact limited the potential for the provision of emotional support from a trained DBI Level 2 practitioner. To overcome this issue, one service trained its administrative practitioners as Level 2 practitioners, so that they can offer a level of support from the first contact.
"Those two guys who do the admin, they are now Level 2 trained. So, what it allows them to do is when they take…they bring a referral in and they make the packs up and they will make everything all kind of streamlined. They can then do that initial call. Start populating the D-MaP and then allow the colleagues who will be delivering the interventions to pick that up and they can then take that care on." Level 2 practitioner
6.3.3 Uptake of support following first contact
There was wide variation by Level 2 provider in how and when the first contact was followed up. This was often client-led but could also be affected by Level 2 practitioners' availability. Assessment of risk was considered in determining the location and the number of Level 2 practitioners involved in the first face-to-face encounter.
Individuals who accessed support from DBI were generally willing to engage in any service that offered support without being placed on a waiting list. However, those interviewed were largely individuals who had engaged beyond the first contact.
Some individuals felt that they had recovered enough by first DBI Level 2 contact to not need the service and felt that their decision not to engage may free appointments for those more in need. Fourteen percent of all referrals to DBI received one supportive phone call and opted not to receive further support (Figure 4.4). Police officers interviewed expressed some concern that this may happen more often when alcohol or drug use has been involved, with the individual in distress feeling more able to cope when they become sober again. Level 2 practitioners noted that some individuals who had exhibited high levels of alcohol or drug abuse were less likely to recall that they had been referred and therefore needed further explanation of the nature and purpose of the DBI intervention. There was a perception that this group of individuals were more likely to feel that DBI was not what they were looking for and thus disengage. Over time, pilot sites introduced elements of the Distress Management Action Plan on first contact to ensure that individuals had some form of support even if they chose not to engage with DBI Level 2 practitioners beyond that contact.
Some Level 2 practitioners perceived particularly vulnerable people as being hard to engage, suggesting that referring them could lead to further disappointment, which could be harmful:
"People whose depression is really quite severe, you know, they're not able to lift themselves enough to be proactive in doing things. Addictions is another difficult one as well, if they're there as well, you know, that's always the priority; or other ones would probably be when the housing situation's really bad cause that really should be taken care of first so they're not in a position to, you know, if they're homeless and they're living in the homeless unit which is quite chaotic, they're probably not really in the position where the techniques that you're giving them are going to really help at the moment till they get a roof over their head and they feel safe." Level 2 practitioner
Level 2 practitioners mentioned that some individuals who had not engaged on their first referral, did so after further referrals, suggesting it was important to continue with offers of support until the individual was ready to engage.
6.3.4 Variation in length and intensity of Level 2 support
Variation in the length and intensity of support provided by the pilot sites is reported in Section 4.5.1. There was also variation across pilot sites in the number of support sessions delivered and the total time for an intervention: Aberdeen City delivered the fewest average support sessions (although they had the highest proportion of support that went over 14 days, see section 4.5.1) and Scottish Borders delivered the highest average number of support sessions. Some of this variation may be accounted for in the different ways in which sites recorded the number of sessions but these findings reflect the person-centred approach of DBI support. The total time required for each person receiving a DBI Level 2 intervention comprised of contact time with each individual plus associated administrative time. A quarter of cases (26%) took no more than four hours in total, while 62% took between four and seven hours in total, and 12% more than seven hours in total.
Level 2 practitioners suggested the length and intensity of DBI sessions were person-led, taking individuals' circumstances and needs into account. However, data from those who took part in the evaluation surveys indicate that differences in completion time or total time for the intervention were not associated with characteristics of the individual or the nature and level of distress (Appendix 3, Table A5.3). This suggests that differences in length of support were due almost entirely to the different practices, and perhaps different interpretations of person-centred approach, of the Level 2 providers.
While individuals who accessed DBI generally described the offer of 14 days of support as about right, a substantial minority (30%) of individuals who responded to the surveys felt it was not enough. Individuals who felt they had become less distressed[9] during the course of the intervention were more likely to say that two weeks was about right. However, neither higher numbers of hours of support beyond 4 hours nor intervention periods beyond 14-days of support resulted in significant additional improvements on levels of distress (Appendix 3, Tables A6.5 and A6.6).[10]
Some Level 2 Practitioners mentioned a tapering off period, where support was more intensive in the first week, then reduced in the second week. This allowed the individual to adjust to the end of the service.
"We just work our way through it for the 14 days and try and get as much of the work done within the first seven days with them and get it into place as much as we possibly can because you don't really want to just be flipping the rug out from somebody's feet after 14 days, so the second week try and tell them that so that maybe the support isn't as intense on the second week so you're kind of weaning them back off getting all the support so it's not as if 'oh 14 days, I've seen you every day and I've had a phone call every day for 14 days and now it's all just disappeared." Level 2 practitioner
However, comments from some individuals who had accessed DBI suggested that they felt they had fewer sessions than expected or these were more spread out due to organisational issues within Level 2 services. One individual felt that the ending of the sessions was a little abrupt:
"And then I rang up and they said we'll have another meeting which I couldn't attend cause I had double-booked, and then I went to another meeting with the DBI and then he said 'right that's you, you've given me this information, go there, there or there' and you're out the door." Individual
6.4 Provision of a compassionate, constructive and effective response at DBI Level 2
Level 2 practitioners generally perceived DBI as an effective way for services to respond to people in distress and as beneficial to those who engaged (See Appendix 3, A6.13). DBI was seen as an empowering service that reduced the risk of dependency arising from long term contact with a service and provided rapid and intensive support to the individual recovering from immediate distress. There was recognition that DBI may have had less impact on individuals who repeatedly access services, often with severe and enduring mental health conditions. However, DBI still played a role in supporting these individuals to some extent.
"Even the smallest of change can be a huge thing for something, like, just somebody even having the confidence to decide whether they want to have a cup of tea or a cup of coffee, that is huge to get somebody to actually have the confidence that they can make their own decision and their own choice, and that's what I like about the DBI, it's putting the empowerment back onto the person to make the choices, to get them to take control of their own self-management of their mental health and their own wellbeing and signposting them or getting them access into other services that can complete and fulfil the rest of it for them." Level 2 practitioner
"We do get quite often a lot of referrals from police for people who already fall into that category of revolving door, you know, because they'll mention in the police…in the referral that, you know, this person phones regularly because of this issue or because of this issue. And I think that, you know, I have to narrow…I was very optimistic for DBI preventing that behaviour developing, but I was very pessimistic about it changing any of that behaviour. But some of the cases we've had come through I have to admit it does seem very positive, the outcome. So, yeah, I do think there is evidence it's working." Level 2 practitioner
The Level 2 intervention was acceptable to most of the individuals who engaged in the programme and generally met their immediate needs, offering an opportunity to talk without being judged. Overall, individuals who accessed support from DBI Level 2 reported experiencing high levels of compassion from their Level 2 practitioner and very positive impacts of the DBI Level 2 intervention on their ability to self-manage their distress. Findings discussed fully in Section 7.2.2 suggest that the more compassionate the response at Level 2, the better the outcomes for individuals.
"To be honest with you I'm quite easy talking to people so I was kinda glad. I wanted it to go down that route, I mean, I wanted… when I was in prior to that I wanted to go see someone as opposed to getting put on sleeping pills. So yeah I was quite happy to do it. Yeah, I was glad, I was glad that I was going to get to speak to someone." Individual
Misconceptions regarding what the Level 2 service could offer led to a negative response from some individuals. These misconceptions included expectations on the part of some individuals interviewed that they would be receiving a counselling or therapeutic service, which led to disappointment at the short term and more practical focus of DBI. Some individuals overestimated the level of support they would receive, expecting it to help them address their issues in full, rather than providing signposting to other services.
"I think I expected something a bit more like counselling. And what happened to me was a very extreme PTSD [post-traumatic stress disorder] reaction to a situation. And it was really…which is very scary for me 'cause I hadn't actually experienced anything on that scale before. It was very extreme. And I was really scared about it. And I think I would have liked a bit more information about PTSD and a bit more reassurance that what I was feeling was normal. And I didn't really get that to be honest." Individual
"To be quite honest, to me it just felt like a palm off. They said 'right, this is all you're entitled to, you don't have to come back to us again but if you want to contact there, there, there or there you're more than welcome to, but your sessions with us are finished' and I felt quite low at that point, because I thought you were going to sort everything out for me, like, talk to you and, like, distress. But it wasn't, it was just to see what was on my mind and go to these other organisations." Individual
Most individuals accepted the Distress Management Action Plan as a useful approach to work through triggers and coping mechanisms. Some DBI Level 2 practitioners felt that the Distress Management Action Plan was an overly manualised approach, and its use needed to be centred on an individual's emotional state. Some DBI Level 2 practitioners felt that some individuals were not ready to begin this process until they had been able to talk about their distress and build trust in the relationship.
"I think a third of service users are not completing them. I think they feel it's a paperwork overload. They feel there's too much paperwork. We've had a lot of feedback of that, that they are feeling that it's a paperwork overload." Level 2 practitioner
6.5 Staffing and cost implications of Level 2 delivery
The staffing required to deliver DBI is presented here because it is important to acknowledge the number and composition of staff required to meet the demand for DBI services and to know how this has changed over the rollout of the DBI programme.
| Financial Year 2019-2020 | South Lanarkshire | North Lanarkshire | Aberdeen | Inverness | Scottish Borders |
|---|---|---|---|---|---|
| Lead/Co-ordinator | |||||
| Statutory sector lead | 1.0 AfC Band 8A | Joint with S.Lan | no | no | 0.6 AfC1 Band 8B |
| Third sector lead | no | no | yes | yes | no |
| Practitioners (FTE*) | |||||
| DBI Manager/ Co-ordinator | 1.00 | 0.13 | 1.00 | 1.00 | 0.85 |
| DBI Senior Practitioner | 0.00 | 1.00 | 0.00 | 0.00 | 1.00 |
| DBI Practitioner | 6.40 | 5.40 | 5.50 | 3.60 | 2.65 |
| DBI Sessional Practitioner | 0.50 | 0.00 | 0.12 | 0.00 | 0.00 |
| Administrative Support | 0.50 | 1.15 | 0.50 | 0.71 | 0.85 |
| Other staffing | 0.00 | 0.00 | 0.00 | 0.20 | 1.00 |
| Total Number of staff** | 12 | 11 | 9 | 8 | 8 |
| Total staff by FTE* | 8.40 | 7.68 | 7.12 | 5.51 | 6.35 |
1 AfC: Agenda for Change: circular informing NHS Scotland employers of changes to staff pay covered by the Agenda for Change agreement from 1 April 2020.
*FTE, full-time equivalent (35.0 hours per week)
**not including sessional practitioners or lead co-ordinator
DBI was implemented in four pilot areas (Aberdeen, Inverness, Lanarkshire and Scottish Borders) and included a managing organisation, DBI Central. Aberdeen and Inverness were led by third sector partners, and Lanarkshire and Scottish Borders by statutory partners (North & South Lanarkshire Health & Social Care Partnership and NHS Lanarkshire, and Scottish Borders Health & Social Care Partnership respectively). There were differences in the way the DBI programme was implemented in the respective council areas of North and South Lanarkshire. These two areas are similar in size to the other pilot areas, each serving big populations of approximately 300,000 people. We present North and South Lanarkshire separately here, to highlight the differences in implementation and costing implications between the two parts of Lanarkshire.
As shown in Table 6.1 a range of staff were required to provide DBI within each site. Each pilot site employed a manager who oversaw local operations and was the point of contact with DBI Central to report back outcomes and other data. Initially, the development and set-up of this role required limited investment at 10% to 50% of full-time equivalent (FTE). Pilot sites employed DBI senior practitioners, DBI practitioners and DBI sessional practitioners. The latter were employed on an as-needed basis. The difference between practitioners and sessional practitioners is that the former were solely employed in DBI on an annual contract but the latter were paid by the hour and possibly were involved in non-DBI activities too. Senior practitioners supported the manager at each site, managed practitioners, worked as practitioners and oversaw the operation of DBI referrals. In South Lanarkshire, the DBI Manager and senior practitioner posts were subsumed into part of an existing team manager post and were funded from elsewhere. These are therefore not shown in Table 6.1.
Clinical leads were employed in Lanarkshire and the Borders to coordinate all aspects of the DBI programme, ensure linkage across all pathways, systems and other local programmes and coordinate Level 1 and Level 2 training. In the case of Lanarkshire, the clinical lead had to coordinate three different organisations which offered DBI Level 2 services across North and South Lanarkshire.
The total number of staff varies across sites; this reflects the size of the population that each site serves and also the stage of implementation. The change in the staffing requirements for DBI Central since its inception in 2016 is presented in Appendix 5 (Table 4.3). Incremental growth of DBI and the changing staff numbers can also impact on other resource requirements such as space, with Scottish Borders DBI locating to new premises in December 2019. There was similar spending across the sites in infrastructure which included premises rental costs, travel and subsistence costs, promotional materials, IT support and other necessary equipment to perform all DBI related tasks and spending in utilities and other bills. Rental costs were kept at a minimum by sharing facilities with other services (Appendix 5, Table 4.4,).
Some Level 2 practitioners found the administrative load of delivering DBI Level 2 burdensome.
"In DBI, you know, you've got huge amounts of admin in terms of processing referrals, writing GP letters, collecting data, actually providing your interventions and then the result of that sometimes is you have to follow safeguarding protocol, you have to do incident reporting, you have to do safeguarding protocols, so just the volume and the quantity and the range of work is a lot to ask of people." Level 2 practitioner
Each pilot site had administrative staff to support the delivery of the DBI service. This ensured that DBI practitioners spent their time providing services to individuals in need rather than spending time on administrative tasks. These admin roles provide value, with their contribution increasing over time towards roughly equivalent of one full-time role.
At times, some services reported being very busy and approaching the capacity of what they could deliver. Some individuals felt that this placed the quality of the service they delivered at risk.
"We've had quite a few times when we've nudged capacity and if that were to persist for any period of time I would say that probably the quality of the service would be quite quickly affected because of things like meetings and supervision and things having to go out of the window in order to physically meet sort of like the 24-hour contact thing and the needs of the service users." Level 2 service lead
6.6 Post DBI: accessing further and future support
6.6.1 Signposting and supported connection to statutory and non-statutory services
An option for Level 2 practitioners at the end of a DBI was to support the individual into another service. Individuals could be either signposted towards more support or actively introduced to other services, including mental health support, through a supported connection to the service. Signposting implies that the person was provided with the details of the particular service and then the person is responsible to make contact with that service. Supported connection implies that the DBI Level 2 service assisted the person with actually making contact with the service, e.g., called the service on behalf of the person to initiate contact. Examples of signposting or supported connection to non-statutory services included apps or other online supports, Breathing Space (a confidential phone line for anyone in Scotland over the age of 16 who is feeling low, anxious or depressed), counselling services and national or local helplines. Examples of signposting or supported connection to statutory services included GP services, NHS 24, social work, and welfare support teams.
A large proportion of individuals who accessed DBI were signposted to, or actively supported to access other services. The majority (85%) of people across all of the pilot sites who had a successful contact at Level 2 were signposted to non-statutory services and 42% of these were provided with a supported connection to the service by Level 2 staff. Just under a third (29%) were signposted to statutory services and 57% were provided with a supported connection to the service by Level 2 staff. This data highlights the importance of having services within the locality to support people beyond DBI Level 2 (Appendix 3, Tables A6.7, A6.8, A6.9, A6.10).
Future provision of DBI should consider the availability of these types of services within the community and the risks of increased demand for services and the impact on waiting lists.
The vast range of services to which individuals were signposted indicates that interventions were tailored to the individual. Signposting to non-statutory services was much more common than to statutory ones (Appendix 3, Tables A5.7 and A5.8).
There was considerable variation between Level 2 providers in the use of signposting to statutory services, ranging from 61% of cases from LAMH, South Lanarkshire and 55% from Lifelink, North Lanarkshire, to 8% from Penumbra, Aberdeen. Conversely, signposting to non-statutory services was lowest from LAMH (65%) and Lifelink (67%), and above 90% from Penumbra (94%), SAMH, Scottish Borders (96%) and the Richmond Fellowship, South Lanarkshire (92%). Differences in signposting practices partially reflect differences in presenting problems in the different areas. However, this does not appear to account for all variations in signposting. The Richmond Fellowship, for example, signposted a smaller proportion of cases to statutory services (23%) than the other Lanarkshire providers, despite a similar profile of users.
Men were more likely to be signposted to statutory services than women (36% compared with 26%). This possibly related to the type of problem they presented with: men were more likely than women to present with self-harm or thoughts of self-harm and suicidal behaviour or thoughts of such, while women were more likely to present with stress or anxiety. Individuals whose main presenting problem was self-harm or thoughts of self-harm (40%), suicidal behaviour or thoughts of suicidal behaviour (41%) or an intentional overdose / self-poison (48%) were more likely to be signposted to statutory services than those whose main presenting problem was depression / low mood (20%) or stress/anxiety (25%) (Appendix 3, Tables A6.7 and A6.8).
There were also differences between Level 2 providers regarding the degree of actual introduction and support individuals received in making initial contact with the service to which they were signposted. Overall, 37% of individuals receiving a Level 2 intervention were actively introduced to non-statutory services. However, this varied from 10% of those receiving an intervention from LAMH to 82% from SAMH. One in six (17%) were actively introduced to statutory services, with this also being high from SAMH (28%), as well as from Lifelink (27%) and LAMH (26%) where signposting to such services was much higher. At Penumbra and Support in Mind, Highlands, active introduction to statutory services was much less common (both 5%) (Appendix 3, Tables A6.9 and A6.10).
The three-month follow-up survey asked about the uptake of services, but because of the small sample size (n= 102), findings should be treated with caution. Of those who answered the question regarding referral to another service (n=58), 52% stated they were referred to another service. Slightly more people stated they were signposted to a service (55% for statutory and 59% non-statutory) or actively introduced to a service (63% for statutory and 65% non-statutory), although several people did not recognise this signposting as a referral (Appendix 3, Table A6.11). Of those who did report being referred, 83% said they took up the service.
6.6.2 Re-presentation to frontline services in distress
The follow-up survey found that in the three months since their last contact with DBI, 47% of respondents reported that they had been in contact with the police, ambulance, their GP, A&E or another emergency service because they were in distress (Appendix 3, Table A6.12). With a lack of a comparator group, it is not possible to say whether this indicates a reduction in such contacts, although other indications from the follow-up survey suggest that those going through DBI have been using what they learned during the intervention to help them manage their distress.
6.7 DBI Programme pathways
Delivery of DBI depends on people appropriately responding to individuals in distress, and on services being available and able to respond in turn. This pathway is standardised - however, there are choices about the organisation of resources and modes of delivery (which in turn affect resource use). Figure 6.1 shows the typical pathway that individuals in distress accessing DBI may end up taking.
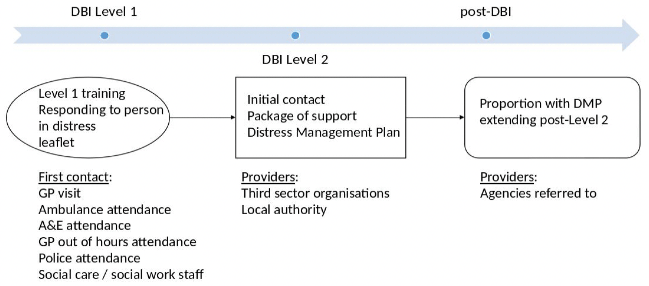
Data from the evaluation, specifically about locality, reason for referral, Level 1 referral agency, number of hours and days attending the Level 2 service and post DBI signposting or initiation to other services, were used to construct three scenarios that represent typical pathways through the DBI programme.
6.7.1 Using the scenarios
Three scenarios are presented below. The purpose of these scenarios is to highlight observations about successful configurations, and of challenges, in organisation and use of resources. Unit costs (Curtis et al. 2020) have been added to the scenarios for information with the focus being on Level 2, which is the core component of DBI from the individual user perspective. Where applied, unit costs are presented in parenthesis and use data presented in Appendix 5, Table 4.2. It is also assumed that without DBI, the frontline service would have responded to the individual e.g. Police Scotland would have attended a call out or an individual would have attended a GP appointment, so no additional cost is incurred as a result of providing a compassionate response at DBI Level 1 response and referring onto a DBI Level 2 provider.
The constructed scenarios set out below follow the individual user pathway, drawing on data from the evaluation data set for context. Key decision points on resource use are indicated at the end of each scenario. The decision points also draw on findings from the wider evaluation to illustrate where choices need to be made in the further development and rollout of DBI, including physical space, staff training and onward support. Although they are presented under specific scenarios, they should be considered in any setting where DBI is being delivered. Presenting these scenarios transparently can aid realistic and feasible decisions about delivering DBI to be applied by decision makers in their local context.
6.7.2 Scenario 1
In Lanarkshire, 54% of Level 2 referrals came from A&E and out of these 32% of referrals were for reasons of (thoughts of) self-harm and 43% with suicidal thoughts or behaviour. For those individuals who received Level 2 support from LAMH, 77% of participants had at least seven hours of support and 42% received support of 15-21 days at Level 2.
In this scenario, an individual presents at A&E in Lanarkshire with thoughts of self-harm. The A&E clinical contact (Level 1 practitioner) provides a compassionate response and suggests a referral to a Level 2 DBI service. The individual views this positively and confirms they would like to be referred and the Level 1 A&E practitioner completes the referral paperwork.
The next day the individual receives a call from the Level 2 provider, LAMH. The sessional practitioner provides more detail about the programme and sets up a further appointment (£3.43) for the individual with the Level 2 trained specialist. The individual goes on to receive 10 hours of support (£152.40) over the next 18 days in which they have high levels of engagement. The practitioner who provides this service is supported by admin support which is available at the Level 2 provider (£6.50).
At the end of the 18 days, the Level 2 provider recommends several non-statutory services within the local community that the individual could follow up with themselves; the Level 2 provider also contacts a statutory service (£3.81) on behalf of the individual to set up an appointment for further support post-DBI Level 2.
The DBI related cost of this scenario is £166.14.
Key decision points illustrated in this scenario are:
- Who makes the first Level 2 contact. In this scenario we make the assumption it is the session practitioners who makes the first contact but the use of administrative staff to make the first contact with the individual increases the probability of making contact within 24 hours and can free up Level 2 practitioners to be providing DBI but may risk the individual wanting more emotional support that is not provided.
- Is there sufficient, safe space that is accessible to the individuals receiving the Level 2 DBI or does additional space need to be identified and how is this managed depending on levels of demand.
6.7.3 Scenario 2
In this scenario, an individual in distress comes into contact with DBI in Aberdeen through Police Scotland. We have chosen this scenario since Aberdeen was the area with the most Police Scotland related referrals to DBI at 14%. In Aberdeen, 72% of cases required between 4-7 hours of support at Level 2.
As soon as Police Scotland are called to an incident in Aberdeen, the officers who are trained in DBI recognise that the individual is experiencing an episode of distress. They provide a compassionate response and ask the individual if they would like to be referred to a Level 2 DBI service. The individual views this in a positive way and confirms they would like to be referred. The police officer completes the referral paperwork.
The next day the individual receives a call from the Level 2 provider Penumbra who provides more detail about the programme and sets up a further appointment for the individual with the Level 2 trained specialist (£3.43). The individual goes on to receive six hours of support (£91.44) over the 14 day follow up period. The individual completes a Distress Management Action Plan with the Level 2 provider and they identify that further support is needed at the end of the DBI Level 2 process. The Level 2 provider signposts (£2.44) the individual to local community non-statutory services such as online support services.
The DBI related cost of this scenario is £94.87.
Key decision points illustrated in this scenario are:
- The mode of training for the Level 1 frontline staff. Delivery of Level 1 training via an online platform has the potential to reduce cost compared to face-to-face if additional facilities and trainers are required. However, there were concerns this may lower the overall effectiveness of the training. Police Scotland in particular stressed the importance of face-to-face training for all staff in Level 1.
- Feedback on the role and use of the D-MaP was generally positive from individuals highlighting the importance of communication from Level 2 practitioners on the need and purpose of the D-Map.
- Post DBI support is crucial, and most individuals (73%) are at least signposted to non-statutory services. Consideration is needed on the availability of statutory and non-statutory services within the community and the risks of increased demand for services and the impact on waiting lists.
6.7.4 Scenario 3
A GP in the Borders has a standard appointment with an individual. In the appointment, the individual reports feelings of stress and anxiety and appears in distress. Data have shown that 77% of all referrals for stress and anxiety took place at the GP level. In this case, the GP provides a compassionate response and offers to the individual a referral to a Level 2 DBI service.
The individual is contacted within 24 hours by the Level 2 provider (£3.43) and receive 6 hours of support over the 14-day period (£91.44). The individual's situation was particularly challenging requiring a senior practitioner to also be involved providing two hours of supervision to the practitioners regarding this case (£36.92). Following discussion between the Level 2 practitioner and the individual, the Level 2 practitioner contacts both statutory and non-statutory services (£7.62) to set up appointments for the individual to receive further support at the end of the Level 2 DBI.
The DBI related cost of this scenario comes at £139.40.
Key decision points illustrated in this scenario are:
- Within the Level 2 services decisions are needed on staffing composition to ensure a range of skills and experience to meet the needs of a wide range of service users.
- An assessment is needed for each individual to determine if there is a need for paired staff members, such as when dealing with a particularly challenging case, or if different materials are required for each Level 2 user.
6.8 DBI Central – role and activities
DBI Central supported pilot sites' delivery of DBI and ongoing DBI development, coordinating activities, administration and service developments. Overall DBI services perceived the role of DBI Central in coordinating services and enabling open communication and information sharing as an essential component of the DBI programme.
"It's definitely needed, a central point, definitely. Sometimes you're like is it kind of tokenistic central leads and the areas just get on with this and report directly but I think it's very much needed to keep the focus going, information being shared appropriately and I think that has also stopped people just kind of being quite rogue, you know, just going off and doing their own thing which is never done in a bad sense, I don't think… I think because they listen to us and that informs how then they lead all of us, I think it just feels really…it's working extremely well having a central team." Level 2 Service Coordinator
DBI staff reported that the constructive leadership of the DBI programme manager was particularly central to the overall success of the DBI programme.
"…the DBI central team. As much as I don't actually know everybody or anything, but when he [DBI Programme Manager] comes out and does his… We meet up every now and again and he pops into the office to see how we're getting on and he actually…I've never worked with anybody, and I don't know why, that actually listens and takes on board what we're saying and then goes and changes it." Level 2 Practitioner
6.8.1 The Gathering
A specific DBI Central activity was the organisation of twice-yearly national events known as Gatherings. The Gatherings brought together key stakeholders, Level 1 and Level 2 services and provided a forum for sharing practice experiences, consolidating local and national networks and allowing all those involved in DBI to share ownership in the programme as a whole. The Gathering also provided a forum for the evaluation team to share interim evaluation findings and to gather further information to inform the evaluation process. The Gathering was not developed as a core part of the DBI intervention; however, stakeholders considered it to play a vital role in achieving cross-sectoral delivery of the overall DBI programme.
"…it was actually partnership in action, and you could actually feel the difference you were making just by actually putting those boundaries away and working together and I think the openness and the honesty, people have been very candid. I'm not coping with this. I don't understand what you're saying. I don't really agree with that. How does that work? You know, and we were very open about the fact we've made a complete pig's ear of recruitment, somebody's going to have to help us." Level 2 service lead
The Gatherings enabled cross-sectoral delivery of DBI. The success of these events was perceived as stemming from the 'open door' offered by DBI Central and their continuous efforts to listen to stakeholders, acknowledge where implementation was less effective, and address issues in conjunction with those delivering the service.
"You have the support from the central team and part of that really is through the DBI Central manager and his attitude to all of this and his attitude to problem solving and getting people to work together, it's real compassion actually across the piece.'" Stakeholder
6.8.2 Local implementation groups
Each pilot site created a local implementation group comprising key local stakeholders. While engagement across local stakeholders had occurred before, DBI services reported their impression that these local implementation groups engaged more agencies than many had previously experienced.
"The only other thing that's really surprised me is the will on the part of organisations which are really stretched. When we have our implementation groups I'm always really sort of tickled about the fact the manager of the out of hours social work team will come and, you know, they're out of hours. They don't work 9.00 to 5.00 or that the police will find time to come and meaningfully attend. Those things have really surprised me." Level 2 service lead
Contact
Email: socialresearch@gov.scot
There is a problem
Thanks for your feedback