Coronavirus (COVID-19): modelling the epidemic (issue no.113)
Latest findings in modelling the COVID-19 epidemic in Scotland, both in terms of the spread of the disease through the population (epidemiological modelling) and of the demands it will place on the system, for example in terms of health care requirement.
Coronavirus (Covid-19): modelling the epidemic in Scotland (Issue No. 113)
Background
This is a report on the Scottish Government modelling of the spread and level of Covid-19 in Scotland. This updates the previous publication on modelling of Covid-19 in Scotland published on 10th November 2022. The estimates in this document provide an overview of the situation regarding the virus and help the Scottish Government, the health service and the wider public sector plan ahead.
Key Points
- The reproduction rate R in Scotland is currently estimated as being between 0.8 and 1.0 as at 8th November. Both the lower limit and the upper limit have decreased since the last publication.
- The daily growth rate for Scotland is currently estimated as between ‑3% and 0% as at 8th November. Both the lower limit and the upper limit have decreased since the last publication.
- The number of new daily infections for Scotland is estimated as being between 115 and 271 per 100,000 people as at 8th November.
- The most recent wave of the Scottish Contact Survey (10th – 16th November) indicate an average of 5.8 contacts. This has decreased by 6% compared to the previous wave of the survey (27th October – 2nd November) where average contacts were 6.2. Prior to the Covid-19 pandemic, the average daily contacts for adults in the UK were reported to be 10.8.
- Mean contacts have decreased by 19% in the work setting compared to the previous wave of the survey. Mean contacts in all other settings have remained at a similar level compared to the previous wave .
- Mean contacts have increased in 30-49 age group, by 14%, while mean contacts have decreased in the 18-29 and 70+ age groups .
- The largest decrease in interactions between age groups compared to the previous wave of the survey was between those ages 18-29 with themselves.
- Pubs and restaurants saw the largest decrease in percentage of participants visiting compared to the previous wave of the survey, decreasing from 58% to 54%. The percentage of participants visiting a work location had the largest increase, rising from 31% to 35%.
- The percentage of people wearing a face covering where they have at least one contact outside of the home has decreased from 20% to 17% since the last wave of the survey .
- The percentage of people who had taken at least one lateral flow test in the previous 7 days decreased from 21% to 18% since the last wave of the survey .
- The SPI-M-O consensus view is that by 20th December, daily hospitalisations from Covid-19 in Scotland are estimated to be between 1 and 41, and hospital occupancy is estimated to be between 217 and 792.
- Nationwide, during the period 3rd – 16th November, wastewater Covid-19 levels were in the range of 21 to 32 million gene copies per person per day (Mgc/p/d). This continues the downward trend observed in the previous two-week period (22nd October – 4th November) when the levels were in the range of 34 to 62 Mgc/p/d.
Overview of Scottish Government Modelling
Modelling outputs are provided here on the current epidemic in Scotland as a whole, based on a range of methods. Because it takes a little over three weeks on average for a person who catches SARS-CoV-2 (the causative agent of Covid-19) to show symptoms, become sick and either die or recover, there is a time lag in what our model can tell us about any changes in the epidemic.
The Scottish Government presents its modelling outputs to the Epidemiology Modelling Review Group (EMRG). These outputs are included (shown in green) in Figure 1 and Figure 2. Outputs from other modellers are shown in either cyan (for models based only on cases data) or purple (for models based on other data). The consensus range is the rightmost (in red).
The R value, growth rates and daily incidence are also estimated by several independent modelling groups based in universities and the UKHSA. Estimates are considered, discussed and combined at the EMRG, which sits within UKHSA. These are based on data up to 21st November.
The consensus view of the EMRG across these methods was that the value of R in Scotland is between 0.8 and 1.0 as of 8th November 2022 (Figure 1). The lower limit and the upper limit have both decreased since the last publication. R is an indicator that lags by two to three weeks.
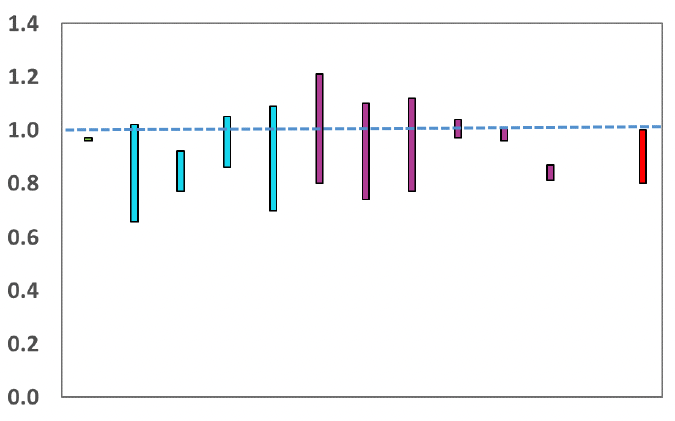
Source: EMRG
The consensus from EMRG is that the growth rate in Scotland is between -3% and 0% per day as at 8th November. The lower limit and the upper limit have both decreased since the last publication.
The various groups which report to EMRG use different sources of data in their models to produce estimates of incidence (Figure 2). The consensus view across these methods was that the incidence of new daily infections in Scotland as of 8th November was between 115 and 271 people. This equates to between 6,300 and 14,900 people becoming infected each day.
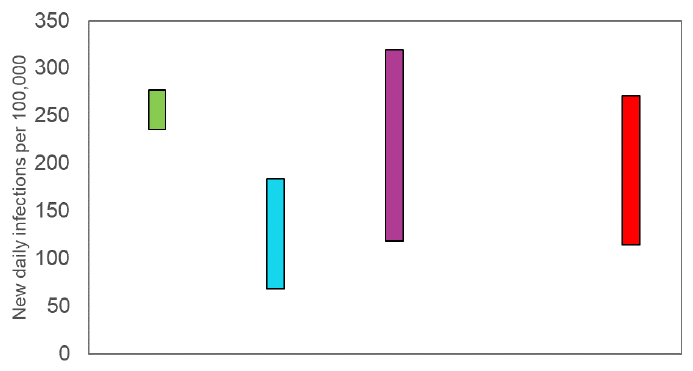
Source: EMRG
What we know about how people's contact patterns have changed
Scottish Contact Survey contact matrices are now published as open data. The dataset contains mean contacts between age groups for all waves of the survey since its inception in August 2020 and will be updated fortnightly to add data for the latest survey wave.
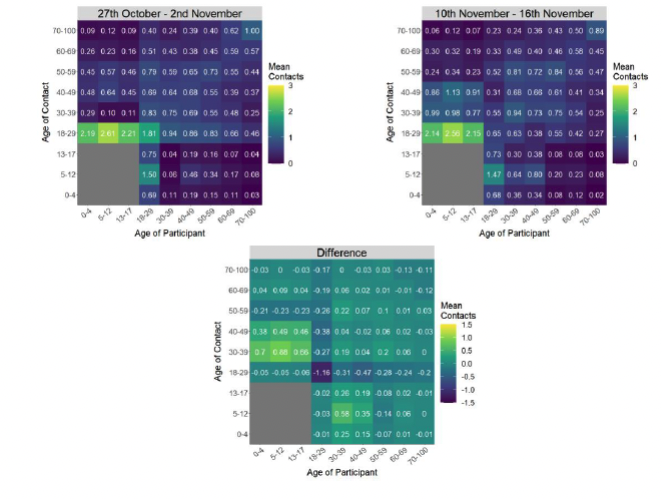
The most recent wave of the Scottish Contact Survey (10th – 16th November) indicates an average of 5.8 contacts. This has decreased by 6% compared to the previous wave of the survey (27th October - 2nd November) where average contacts were 6.2, as seen in Figure 3.
Prior to the Covid-19 pandemic, the average daily contacts for adults in the UK were reported to be 10.8 from the UK-wide POLYMOD study[1].
Mean contacts have decreased by 19% in the work setting compared to the previous wave of the survey. Mean contacts in all other settings have remained at a similar level compared to the previous wave..
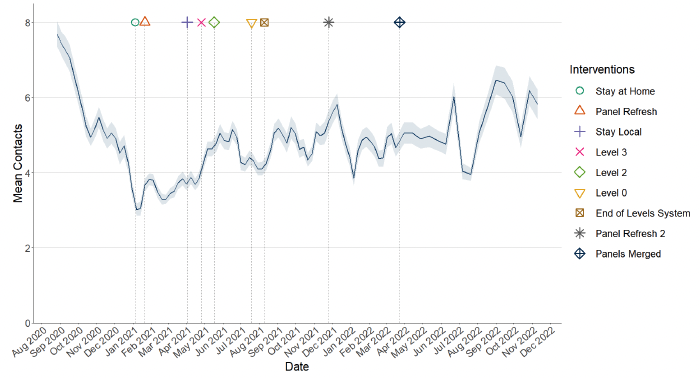
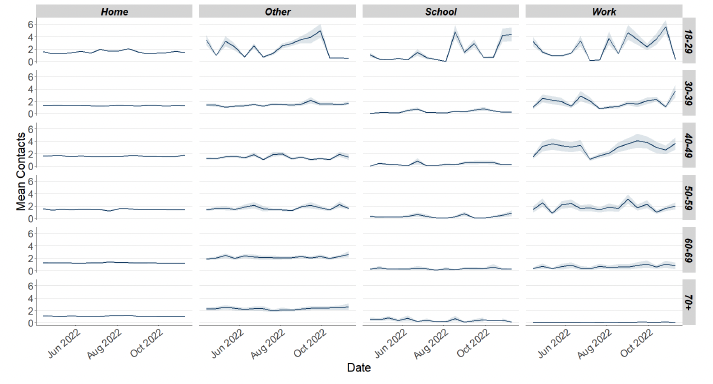
Figure 4 shows how contacts change across age group and setting. Mean contacts have increased in 30-49 age group, by at least 14%, whilst mean contacts have decreased in the 18-29 and 70+ age groups .
The heatmaps in Figure 5 show the mean overall contacts between age groups for the surveys relating to 27th October - 2nd November and 10th - 16th November and the difference between these periods. The largest decrease in interactions between age groups compared to the previous wave of the survey was between those ages 18-29 with themselves.
Pubs and restaurants saw the largest decrease in percentage of participants visiting compared to the previous wave of the survey, decreasing from 58% to 54%. The percentage of participants visiting a work location had the largest increase, rising from 31% to 35%. See Figure 6.
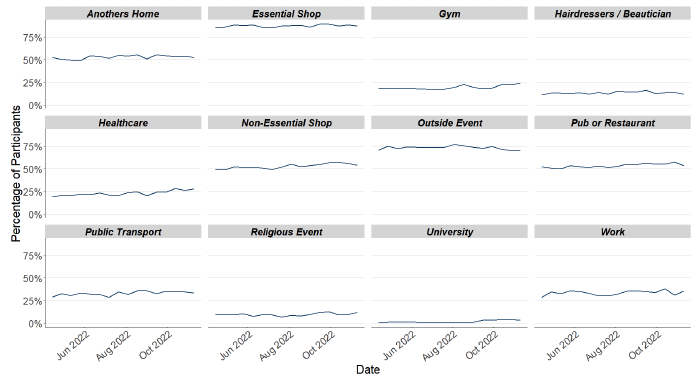
Figure 7 shows the percentage of people wearing a face covering where they have at least one contact outside of the home. This has decreased from 20% to 17% since the last wave of the survey .
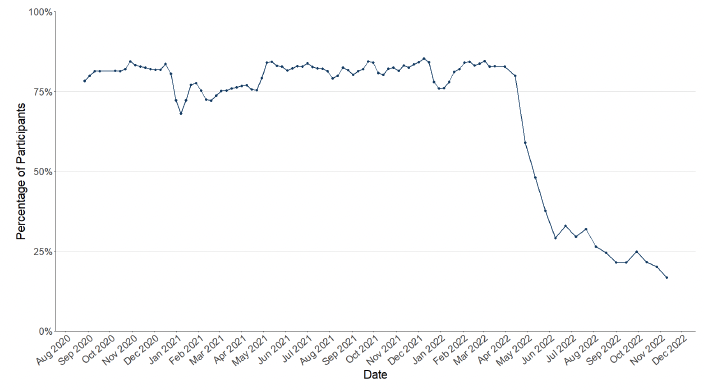
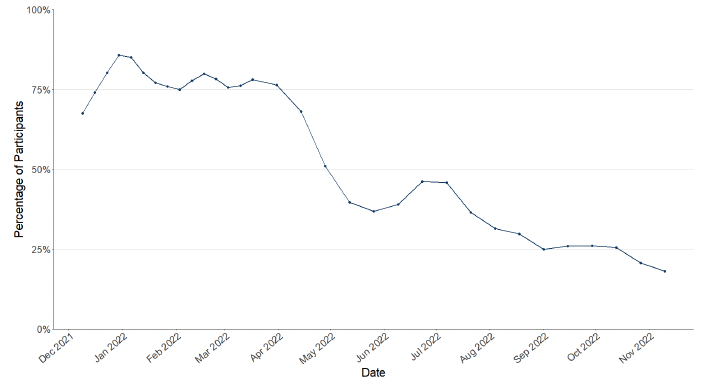
Figure 8 shows the percentage of people who have taken at least one lateral flow test in the previous 7 days. This has decreased from 21% to 18% since the last wave of the survey .
What the modelling tells us about projections of hospitalisations and hospital occupancy in the medium term
SPI-M-O produces projections of the epidemic (Figure 9 and Figure 10), combining estimates from several independent models. These projections are not forecasts or predictions. They represent a scenario in which the trajectory of the epidemic continues to follow the trends that were seen in recent data and do not include the effects of any future policy or behavioural changes. The delay between infection, developing symptoms and the need for hospital care means they cannot fully reflect the impact of behaviour changes in the two to three weeks prior to 7th November. The projections include the potential impact of vaccinations over the next few weeks. Modelling groups have used their expert judgement and evidence from UKHSA, Scottish Universities & Public Health Scotland, and other published efficacy studies when making assumptions about vaccine effectiveness.
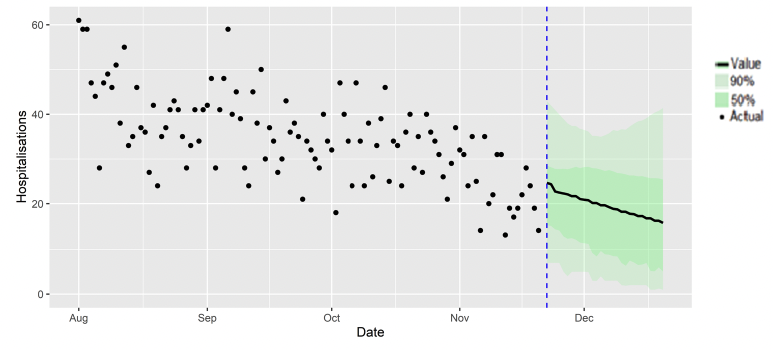
Figure 10 shows the SPI-M-O consensus on hospital occupancy. Hospital occupancy is determined by the combination of admissions and length of stay, the latter of which is difficult to model with confidence.
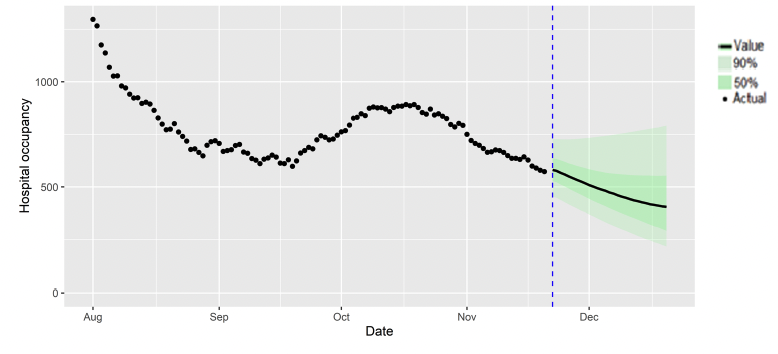
The SPI-M-O consensus view is that by 20th December, daily hospitalisations from Covid-19 in Scotland are estimated to be between 1 and 41, and hospital occupancy is estimated to be between 217 and 792.
What can analysis of wastewater samples tell us about local outbreaks of Covid-19 infection?
Levels of Covid-19 RNA in wastewater collected at a number of sites around Scotland are adjusted for population and local changes in intake flow rate (or ammonia levels where flow is not available). See the Technical Annex in Issue 34 of Scottish Government Research Findings for the methodology. These reports are based on the most recent data available. Future updates to data may lead to small retrospective changes.
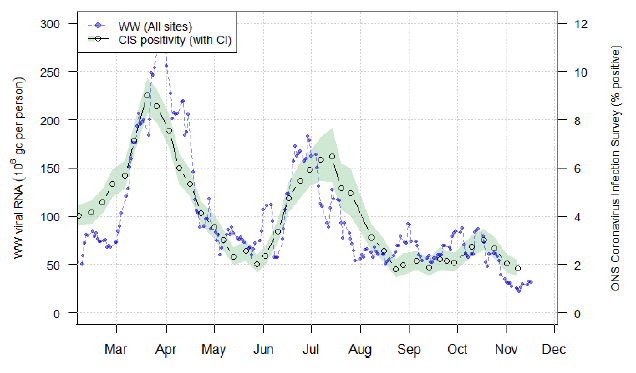
Nationwide, during the period 3rd – 16th November, wastewater Covid-19 levels were in the range of 21 to 32 million gene copies per person per day (Mgc/p/d). Levels in the previous two-week period (21st October – 2nd November) went down from 61 to 30 Mgc/p/d. The latest data consolidate this decrease. This is in line with most recent changes seen in the ONS Coronavirus Infection Survey as of 8th November.
In Figure 11, we show national wastewater Covid-19 levels up to 16th November 2022 with the ONS Coronavirus Infection Survey (CIS) estimates of Covid-19 prevalence superimposed.
Looking to the future
What may happen in the future around SARS-CoV-2 is uncertain and therefore there are a number of possible Covid-19 futures that may occur in the future. For example, the current Omicron wave may dissipate leaving low levels of Covid-19, or a new variant may emerge potentially having vaccine escape or increased severity, or people's behaviours may change. One approach to this uncertainty is to model alternative versions of the future through the development of different Covid-19 scenarios.
Given what we know about Covid-19 these possible futures range from a world where immunity reduces Covid-19 hospitalisations and ICU to low levels, through to variant world where a variant with immune escape enters Scotland and Covid-19 hospitalisations and ICU could increase. In between these two extremes there could be possible futures where people's behaviour becomes polarised between those who continue with Covid-19 precautions e.g. hand washing etc. and those who do not.
The scenarios we provide in the next section look at what could happen for planning purposes, not to forecast what will happen. The assumptions are based on our most up to date knowledge, but do not include the effect of future changes in treatment of Covid-19 e.g. widespread use of antivirals or changes in behaviour in response to high levels of infections e.g. in variant world. Therefore, in the most extreme scenarios the peak may be lower than suggested if behaviour or restrictions changed.
There is no linear progression between the worlds and all are plausible. Each world inherently contains a different threat level requiring a different approach to management.
Immune World
In this possible future vaccines and natural immunity are effective at keeping Covid-19 at low levels. New variants may emerge in Scotland but for the foreseeable future infections are based around Omicron.
Infections may decrease from current levels over the coming weeks and months to very low levels. Likewise hospital and ICU occupancy may follow this trend relieving the pressure on healthcare services. Issues with new variants are not considered in this world and therefore levels of infections remain low (see Figure 12).
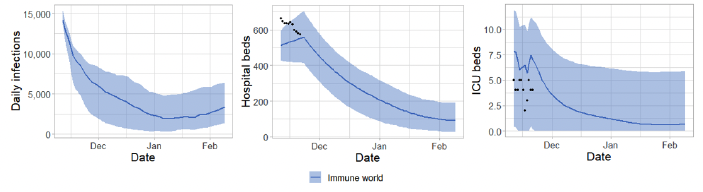
In Immune world Covid-19 in Scotland reduces below epidemic levels, becoming endemic. Cases of Covid-19 therefore spring up only as rare outbreaks which are controlled through public health measures. People's lives return to something close to normality e.g. physical distancing is not needed but people still choose to self-isolate and hygiene is good. As vaccines are effective, take-up of first/second/third doses are good and boosters become part of an annual cycle like flu. The numbers of people who need medical treatment or hospitalisation for Covid-19 remain low.
The focus moves away from Covid-19 response and into recovery. This includes addressing learning losses, treating Long Covid and working through the hospital backlog. Wellbeing measures improve with reduced anxiety and increased happiness. Those from the highest risk groups feel they can reintegrate without government interventions. The economy continues to recover from the effects of Covid-19. Travellers do not face significant issues with trips overseas.
Polarised world
In this world, vaccines and natural immunity are effective at reducing infections. The approach followed relies on individual risk assessment and behaviours. However, society becomes polarised as some continue to take up vaccines and follow guidance while others are more reluctant. Covid-19 becomes a disease associated with those who do not or cannot get full vaccine benefit and do not or cannot adopt a risk based approach.
Impacts on hospital/ICU occupancy are uncertain but levels may be higher than what may happen in Immune world (see Figure 13).
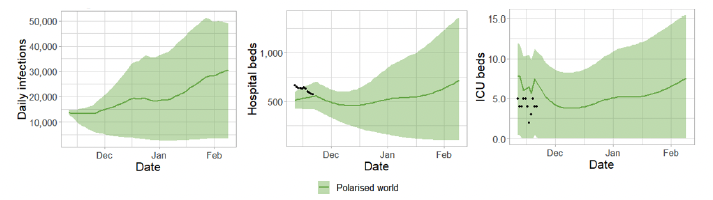
Cases of Covid-19 spring up and are hard to control in those who are not vaccinated or vulnerable. People's lives return to a "new normal" but, due to polarised groups in society with some following and some not following guidance, infections remain.
Vaccines are effective so older and more vulnerable people come forward for future doses in high numbers.
The focus remains on Covid-19 and the shift onto recovery is slower. Existing learning losses are harder to rectify and continue to accrue due to infections within education settings. The hospital backlog is difficult to address as hospitals are still dealing with Covid-19 cases. The population becomes polarised in to those whose wellbeing improves e.g. lower risk people and those whose wellbeing deteriorates e.g. higher risk or poorer people whose levels of anxiety increase as Covid-19 circulates. They continue to experience greater illness, greater poverty or disruption to their income. The economy continues to be impacted from the effects of Covid-19.
Variant world – vaccine escape with same severity as Delta
In this possible future a variant with vaccine escape emerges in Scotland presenting a challenge even for fully vaccinated people. This new variant leads to increased transmission, but not to increased severity compared to previous variants. In this scenario other NPIs may need to be put in place for a short time. This world is similar to what has happened in Scotland with the emergence of Omicron.
Omicron may be reduced to low levels within Scotland as a new variant takes over. This causes a new wave of Covid-19 infections as well as increases in hospital and ICU occupancy. People's lives are disrupted due to the increasingly high levels of infections leading to time off work ill or isolating.
To show the potential impact assume a new variant appears in Scotland over the festive period. The timing is uncertain and a potential new variant may appear sooner than this or significantly later but has currently been lined up over the festive period to show illustratively what could happen. The new variant may cause Omicron infections to decrease significantly or disappear entirely (and is not shown). The new variant is modelled with similar transmissibility and vaccine escape as Omicron with severity characteristics similar to Delta. It could lead to high levels of infections leading to hospital occupancy rising above capacity restrictions. With sustained high levels of infection we could again see increased staff absences in a number of sectors that were affected by this in the recent Omicron wave. See Figure 14.
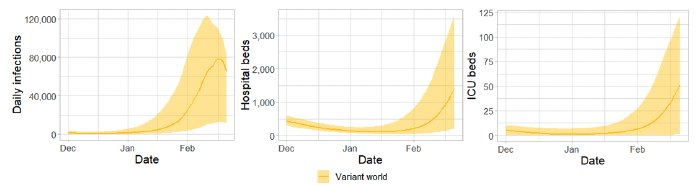
The focus remains on Covid-19 and it is hard to shift on to recovery. Continued infections within education settings and staff shortages may impact schools. The Covid-19 strain on hospitals is high due to the very high numbers of infections and workforce pressures grow making it difficult to address the hospital backlog. Wellbeing measures deteriorate with people reporting low happiness and general 'tiredness with it all'. The economy continues to be impacted from the effects of Covid-19 with many people off work. Travellers may not want to come to the UK as the new variant sweeps through.
Variant world – vaccine escape with increased severity compared to Delta
As with the other example of Variant world, a new variant appears in Scotland in the Scotland over the festive period. The timing is uncertain and a potential new variant may appear sooner than this or significantly later but has currently been lined up over the festive period to show illustratively what could happen.
The new variant may cause Omicron infections to decrease significantly or disappear entirely (and this is not shown on the graph). It is modelled with similar transmissibility and vaccine escape as Omicron with severity characteristics 50% higher than Delta, purely for illustrative purposes.
It could lead to high levels of infections leading to hospital occupancy rising significantly. With sustained high levels of infection we could again see increased staff absences in a number of sectors that were affected by this in the recent Omicron wave. See Figure 15.
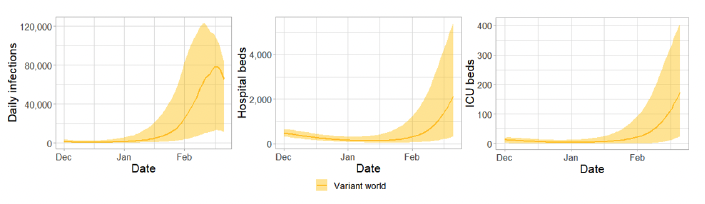
The focus remains on Covid-19 and it is hard to shift on to recovery. Continued infections within education settings and staff shortages may impact schools. The Covid-19 strain on hospitals is high due to the very high numbers of infections and workforce pressures grow making it difficult to address the hospital backlog. Wellbeing measures deteriorate with people reporting low happiness and general 'tiredness with it all'. The economy continues to be impacted from the effects of Covid-19 with many people off work. Travellers may not want to come to the UK as the new variant sweeps through.
What next?
Archiving of models is currently being undertaken via the Data Science Scotland GitHub organisation. Details of the Scottish Contact Survey contact matrices are available. See the Technical Annex of issue 96 for details of other archived models.
Contact
There is a problem
Thanks for your feedback