Citizens' Jury on QCovid: Report on the jury's conclusions and key findings
Ipsos Scotland was commissioned to conduct a Citizens' Jury exploring views on QCovid®. QCovid® is a risk model developed to identify people at the highest risk of death or a poor outcome should they catch Covid-19. This report documents the Citizens' Jury process and findings.
Appendix: Ethics panel
The ethics panel included:
- Doreen Grove, Scottish Government
- Lara Macdonald, Centre for Data Ethics and Innovation
- Dr Mavis Machirori, Ada Lovelace Institute (from January 2022)
- Reema Patel, Ada Lovelace Institute (until January 2022)
- Professor Shannon Vallor, University of Edinburgh.
Secretariat
- Úna Bartley, Scottish Government
- Gary Todd, Scottish Government
- Tom Speight, Scottish Government
- Albert King, Scottish Government
- Ryan Anderson, Scottish Government
Recruitment and sampling
| Quota | Group | % in population | Number selected (and confirmed) for the Jury |
|---|---|---|---|
| Age | 16-24 | 11% | 4 |
| Age | 25-34 | 18% | 6 |
| Age | 35-54 | 32% | 9 |
| Age | 55+ | 38% | 11 |
| Gender | Female | 52% | 16 |
| Gender | Male | 48% | 14 |
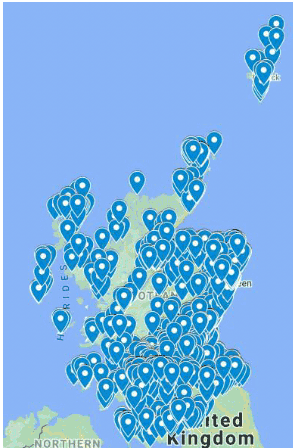
| Scottish region | Central | 12% | 3 |
| Scottish region | Glasgow | 13% | 3 |
| Scottish region | Highlands and Islands | 8% | 3 |
| Scottish region | Lothians | 15% | 5 |
| Scottish region | Mid Scotland and Fife | 12% | 4 |
| Scottish region | North East Scotland | 14% | 5 |
| Scottish region | South | 13% | 3 |
| Scottish region | West | 13% | 4 |
| Ethnicity | African, Caribbean, Black or Black Scottish/British | 1% | 1 |
| Ethnicity | Asian, Asian Scottish or Asian British | 3% | 2 |
| Ethnicity | White Scottish/Other British/White Other | 96% | 26 |
| Ethnicity | Other ethnic group or mixed/multiple ethnic groups | 0% | 1 |
| Disability | No long-term physical or mental health condition | 70% | 21 |
| Disability | Long-term physical or mental health condition which is limiting | 24% | 7 |
| Disability | Long-term physical or mental health condition which is not limiting | 6% | 2 |
| SIMD | 1 – most deprived | 21% | 7 |
| SIMD | 2 | 21% | 6 |
| SIMD | 3 | 20% | 6 |
| SIMD | 4 | 20% | 6 |
| SIMD | 5 – least deprived | 19% | 5 |
| Attitude towards data access[11] | Very comfortable | N/A | 11 |
| Attitude towards data access | Somewhat comfortable | N/A | 9 |
| Attitude towards data access | Somewhat uncomfortable | N/A | 2 |
| Attitude towards data access | Very uncomfortable | N/A | 2 |
| Attitude towards data access | Don't know | N/A | 6 |
Onboarding materials: welcome pack
Welcome
Thank you for agreeing to become part of the QCovid® Citizens' Jury.
The purpose of the Jury is to consider the use of a tool called QCovid®, which uses health data to identify factors that put people at a higher risk of being seriously unwell or dying because of Coronavirus. These factors – like age and medical condition – were used to build what's called a risk prediction model, which estimates an overall risk level. More information on QCovid® is provided below.
There are different ways in which risk prediction models, like QCovid®, can be used in Scotland. The role of this Jury will be to consider the benefits and risks of tools such as QCovid®, and to discuss the ethical issues around using people's health data.
Before taking part, it is important that you understand why the research is being carried out and what it will involve. If you have any questions, please do not hesitate to get in touch (contact details are at the end of this document).
What is a Citizens' Jury?
A Citizens' Jury brings together a randomly selected group of people who broadly represent the entire community. The people who attend will listen to evidence from a range of experts, learn about key issues, discuss them with one another, and then deliberate and draw conclusions together.
Due to the uncertainty of the ongoing COVID-19 pandemic, we have decided to run the Citizens' Jury virtually using the online platform Zoom, rather than face-to-face. We did not want to take any unnecessary risks and felt that it was better to seize the moment rather than wait until we can safely meet face-to-face. You will be able to view all supporting materials, such as recordings of presentations, slide packs, and summary documents – all from the comfort of your home.
The Jury will meet over six sessions to learn, deliberate and discuss QCovid® before drawing conclusions about the use of this type of tool. The Jury will answer this important question - 'What are the risks and benefits of using public health data to predict people's risk of dying from Covid?' – with a focus on the ethical issues surrounding the use of tools like QCovid®. By ethical issues we mean the benefits, risks and wider social harms that should be considered with a risk model such as QCovid®.
At the end of the process, Ipsos MORI will produce a report outlining the Jury's conclusions. The report from the Jury will be presented to the Scottish Government in April 2022 and the Scottish Government will consider the Jury's conclusions. This is a fantastic opportunity to help the Scottish Government decide how it might use tools such as QCovid® in its response to the pandemic.
What is QCovid®?
QCovid® was commissioned in 2020 by the Chief Medical Officer for England on behalf of the UK government. The first QCovid® tool was developed using the QResearch database hosted at Oxford. This database has anonymised data from GP and hospital records, COVID-19 test results and death registries. Factors such as age and medical conditions, which were found to increase risk relating to coronavirus, were used to build a risk prediction model. The model, QCovid®, estimates someone's combined risk of catching coronavirus and being admitted to hospital and their combined risk of catching coronavirus and dying.
The tool has now been updated to include factors such as vaccination status and background infection rate. There is a need to identify those at highest risk of severe outcomes if infected with COVID-19, even if individuals are vaccinated.
The model was tested to find out whether it accurately predicted severe outcomes due to COVID-19 during the first wave of the pandemic in England. More recently, it has been tested on vaccinated individuals between December 2020 and June 2021.
The research, published in the British Medical Journal (BMJ), showed that the model performed well in predicting severe outcomes due to COVID-19 (death and hospitalisation) in both models. You can view the research on the BMJ's website.
The research team is led by Professor Julia Hippisley-Cox at the University of Oxford
The QCovid® team includes researchers from:
- University of Nottingham
- London School of Hygiene & Tropical Medicine
- University of Leicester
- Swansea University
- Queen's University Belfast
- University of Edinburgh
- Department of Health and Social Care
- NHS England and Improvement
- Queen Mary University of London
- University of Liverpool
- University College London
- NHSx
- NHS Digital
For more information about QCovid®.
Who is carrying out the Jury?
Ipsos MORI is an independent research agency carrying out this work on behalf of the Scottish Government.
What is involved in taking part?
You are one of 25 people selected to take part in the QCovid® Citizens' Jury which will be answering the important question:
What are the risks and benefits of using public health data to predict people's risk of dying from Covid?
The Jury will run across six online sessions in February and March and you need to be able to attend all six sessions.
The sessions will run as follows:
- Session 1: Saturday 12th February: 10am-1pm
- Session 2: Thursday 17th February: 6-9pm
- Session 3: Tuesday 22nd February: 6-9pm
- Session 4: Thursday 24th February: 6-9pm
- Session 5: Tuesday 1st March: 6-9pm
- Session 6: Saturday 5th March: 10am-1pm
We will give you £300 to thank you for your time. This will be split into two payments of £150 after the third session and £150 after the final session. You can choose to receive this either as cash (BACS transfer) or in the form of an e-voucher (Amazon). Please just let us know which option you would prefer when we contact you in advance of the first session. Receiving a bank transfer for this amount may impact on any benefit payments or tax positions, so it is worth checking this before choosing a payment method. Receiving an e-voucher will not impact on any benefit payments or tax positions.
You don't need any prior knowledge to take part in the Jury; all we require from you is a willingness to listen to the information presented and share your opinions with us and your fellow participants.
What information will be used?
The findings from the Jury will be anonymised, and we will not reveal personal details without obtaining your explicit consent.
Please note that there may be observers in attendance throughout the Jury. These may be people from academia (for example university researchers) or from Scottish Government (such as representatives from the Highest Risk Division). We will inform you of the presence of any observers and the reasons for their attendance in each session. This is a normal part of Citizens' Juries and helps to foster a sense of openness and transparency in the process for those with an interest in understanding how it is being conducted. They will not contribute to or shape the discussion in any way but will simply listen in on some conversations and plenary sessions. There are strict controls on the number of observers for each session as well as guidelines that observers must agree to before attending.
If you have any queries about this aspect of the Jury, please get in touch (contact details below).
How will we record what you say?
We would like to audio-record our discussion but will only do so with your agreement. Recording the discussion enables us to accurately capture what has been said and helps our researchers with note taking.
How will the information be used?
A report will be published on the Scottish Government's website. It will also be used internally by the Scottish Government to help determine how QCovid® or similar risk prediction models are used in Scotland. The report is likely to use quotes, but we will not name or identify anyone when we use quotes. If you do not want us to quote anything you say, please just let us know.
Do I have to take part?
No. It is your choice whether or not you participate. You can also choose not to answer individual questions and/or leave the discussion completely. You can change your mind at any point, and you do not have to give a reason. If you would like to withdraw your consent to participate, please contact us.
Can I talk about my participation with others?
We encourage you to talk to family and friends during your time as a juror. It is also okay to talk about the fact that you are part of a Citizens' Jury on social media, but we ask you not to share the content of the discussions, as it will be out of context for the general public, and to respect the anonymity of everyone else taking part.
Privacy Notice
We have a legal duty to inform you about why we are collecting information from you for the research. We provide this information in our Privacy Notice which should be read alongside this information sheet. The Privacy Notice outlines what information we will collect and why, and your rights. If you would like another copy of the Privacy Notice, please contact us (see below).
Importantly, you need to know that:
- We will never use your personal data for anything other than this project
- Only Sortition (the organisation who invited and selected you to take part in the Jury) and the Ipsos MORI project team will have access to your personal data
- Only members of the research team will hear the recording and all recordings will be destroyed at the end of the project.
- Your personal data will be securely deleted three months after completion of the project
- You will not be identifiable in any of our reporting.
Where can I get more information?
For more information about the research, or if you have any questions, please contact: [redacted]
For more information about Ipsos MORI.
If you have questions or concerns about your role and rights as a juror, would like to obtain information or offer input, or would like to register a complaint about this study, please contact us.
Next steps
If you are happy to continue to take part in the QCovid® Citizens' Jury, please complete the consent form slip and return it to the researcher by email.
Presentations and speakers
Session One:
- Úna Bartley, Scottish Government – 'Introduction to QCovid® model and the different tools'.
- Professor Sarah Cunningham-Burley, the University of Edinburgh – 'Introduction to public health data ethics and previous public engagement on this topic'.
Session two:
- Professor Aziz Sheikh, Director of the Usher Institute at the University of Edinburgh – 'Introduction to the clinical tool'.
- Professor Alison McCallum, Usher Institute at the University of Edinburgh (and former Director of Public Health and Health Policy at NHS Lothian) – 'introduction to the public-facing tool'.
Session three:
- Professor Aziz Sheikh, Director of the Usher Institute at the University of Edinburgh – 'Introduction to the population tool'.
- Professor Jeremy Brown, University College London and member of the Joint Committee on Vaccination and Immunisation – 'Applying the population tool (vaccination prioritisation example)'.
- Dr Helen Stagg, Usher Institute at the University of Edinburgh – 'Considerations for using the population tool in an anonymised or non-anonymised way'.
Session four:
- Professor Alison McCallum, Usher Institute at the University of Edinburgh (and former Director of Public Health and Health Policy at NHS Lothian) – 'data security and privacy in relation to public health data'.
Session five:
- Professor Sarah Chan, University of Edinburgh – 'data and risk prediction: personal or public health? Thinking about the ethical issues'.
Session five materials
Case studies
As part of the fifth workshop, the jury was put into small breakout groups and asked to continue exploring the risks, benefits and ethical issues by putting themselves in the shoes of someone else. Each group was given a different avatar (a fictional person and scenario) which represented a low, medium or high risk case. Copies of each avatar presented to the jury are shown below:
Case Study 1: Assume that Taj would be categorised as at low risk

Taj is 19. He is a student living in Aberdeen. He is from Glasgow. When he first started at University, he lived at home with his parents in Glasgow and studied remotely due to Covid. This year, he has been able to move into student accommodation. He currently lives with seven other people.
Taj is a non-smoker and lives an active lifestyle. He is on the University's swimming and badminton teams and regularly travels at the weekends for competitions.
He has no underlying health conditions and would be considered at low risk from Covid-19.
When he's not training or studying, Taj likes to go out and spend time with his friends. He doesn't use social media much as he is nervous about sharing his personal information.
The pandemic has made it very difficult for him to have a 'normal' University experience and he has only just been able to start enjoying the sociable side of things, so he hopes that things stay as they are.
Case Study 2: Assume that Jenny would be categorised as at medium risk

Jenny is 43. She lives in a block of flats with her partner and two children. She works full-time as a taxi driver. Her partner is unable to work, so she supports the family.
Because of her job, Jenny comes into contact with a lot of people. On several occasions during the pandemic, she was 'pinged' by the track and trace app to say that she was a close contact of someone who had tested positive and was asked to self-isolate and test. She is self-employed as a taxi driver and is not entitled to sick pay from her employer, so not being able to work when she was 'pinged' caused her stress and financial worry. Other financial support available to her during the pandemic was limited.
Jenny has other health conditions which sometimes affect her daily life, although she has never been on the highest risk list. But she has had issues with her employer in the past when her condition has prevented her from working. Because of her condition, she has been very careful to avoid catching the virus. But as the sole earner, she also needs the money to support her family. She heard on the news recently that the vaccine is becoming less effective against existing variants
Case Study 3: Assume that Benjamin would be categorised as at high risk
Benjamin is 68. He is retired and lives with his wife in the village of Strathblane in Stirlingshire. His wife is registered disabled, so he tends to be responsible for day-to-day tasks such as grocery shopping and collecting prescriptions.
Benjamin is very active in his community and is a member of the local community council.
During the lockdowns, Ben was involved in a number of voluntary initiatives, such as befriending elderly residents living alone and running errands for those who were shielding or isolating. The community response to the pandemic has inspired him to form a community group to continue the befriending service.
In the earlier stages of the pandemic, neither Benjamin nor his wife was identified as being at high risk and so they were not asked to shield. He does not like going to the GP and does not trust the doctors there. However, he has recently been diagnosed with a serious health condition. The diagnosis has affected his life insurance policy, which has worried Benjamin and his wife. He is also becoming increasingly worried by news of an emerging variant of coronavirus which appears to be resistant to the current vaccine.
Case Study 4: Assume that Mabel would be categorised as at high risk

Mabel is 82. She lives in a care home on the island of Islay, where Covid cases have been low.
Before the lockdown came in early 2020, Mabel was able to go out and visit friends, to go on outings with her family when they visited, and to attend appointments. In the early stages of the pandemic, Mabel was identified as being at high risk from Covid and was asked to shield during pandemic. She was very worried about catching the virus, so she followed the advice and did everything she could to keep herself and others safe. Mabel has been grateful to her GP for keeping her informed.
Mabel feels lucky that she has a community supporting her, as the care home and residents who live in the area have been kind and looked after each other during the pandemic.
Her family lives on the mainland and they were unable to visit her for a long time. Although the care home did their best to support her, this has had a negative impact on Mabel's wellbeing and she has been feeling very lonely. Cases of Covid in Islay continue to be low, so she hopes that her family will not be prevented from visiting again.
Risk-benefit exercise (Google Jamboard)
As part of the fifth workshop, participants were asked to assess the balance of risk and benefit of each of the tools based on their discussions so far. This was facilitated via Google Jamboard,[12] a collaborative digital whiteboard. Each facilitator shared their screen so that all participants could see the same whiteboard, which depicted a risk/benefit quadrant chart. Taking each tool in turn, participants were asked to place a digital post-it on the chart according to their assessment of the risk-benefit of the tool. Each group's post-its were assigned a different colour, so that members could see in real-time where other participants were placing themselves. Once plotted on the diagram, participants explained and discussed their reasoning. Screenshots of the completed quadrant charts are shown in the main report.
Session six materials
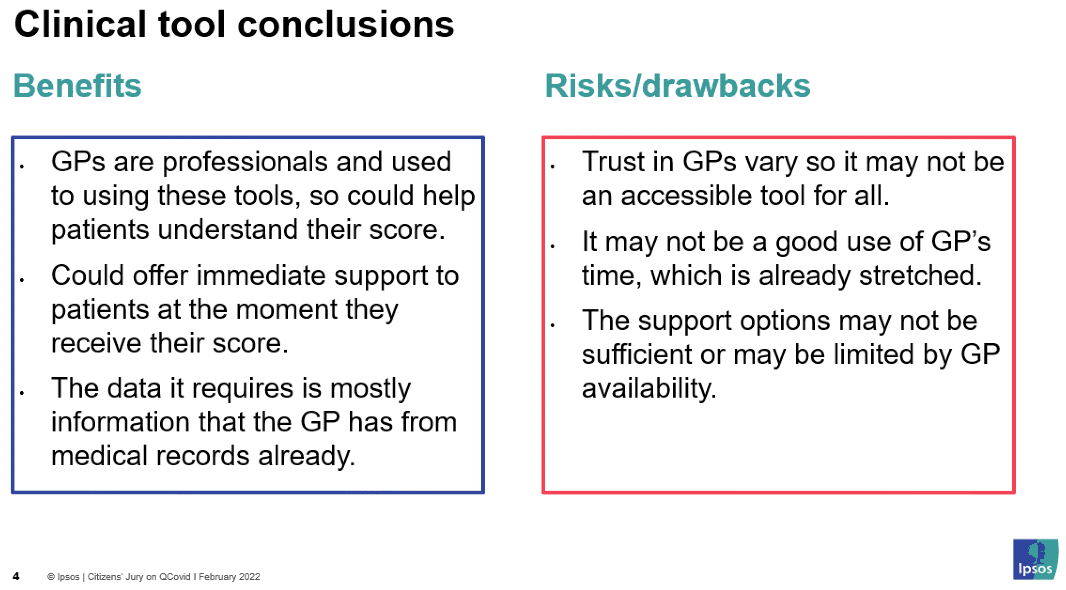
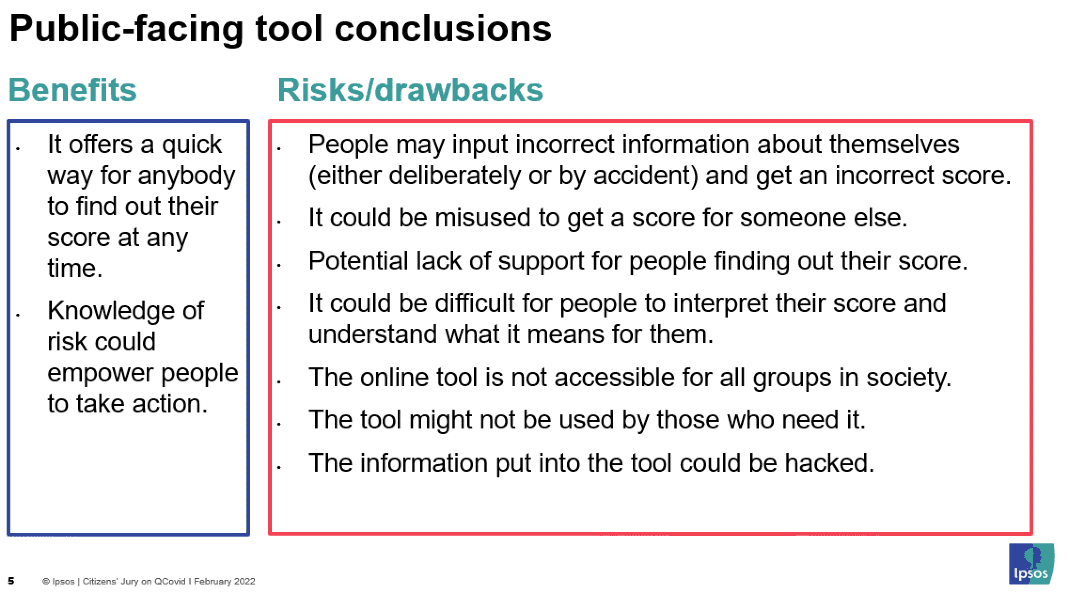
Benefits and risks summaries
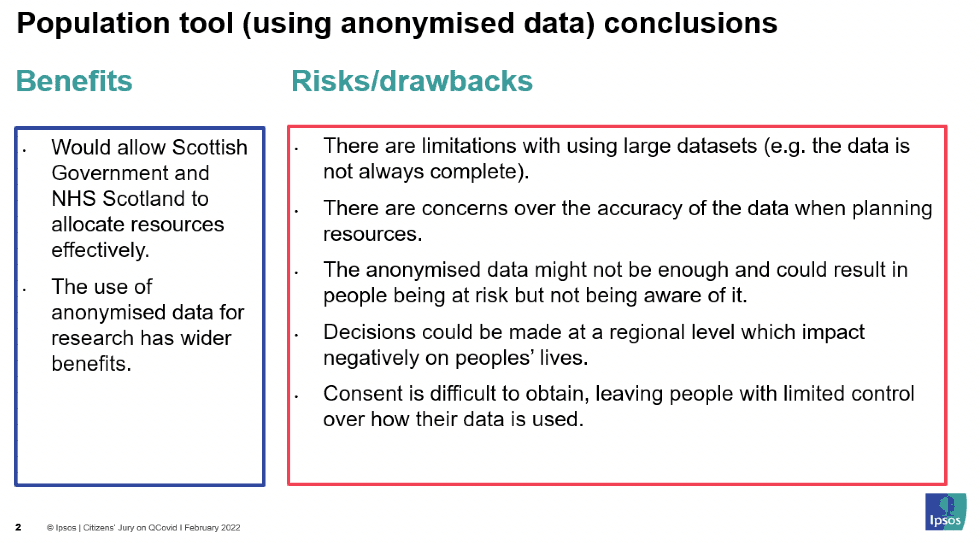
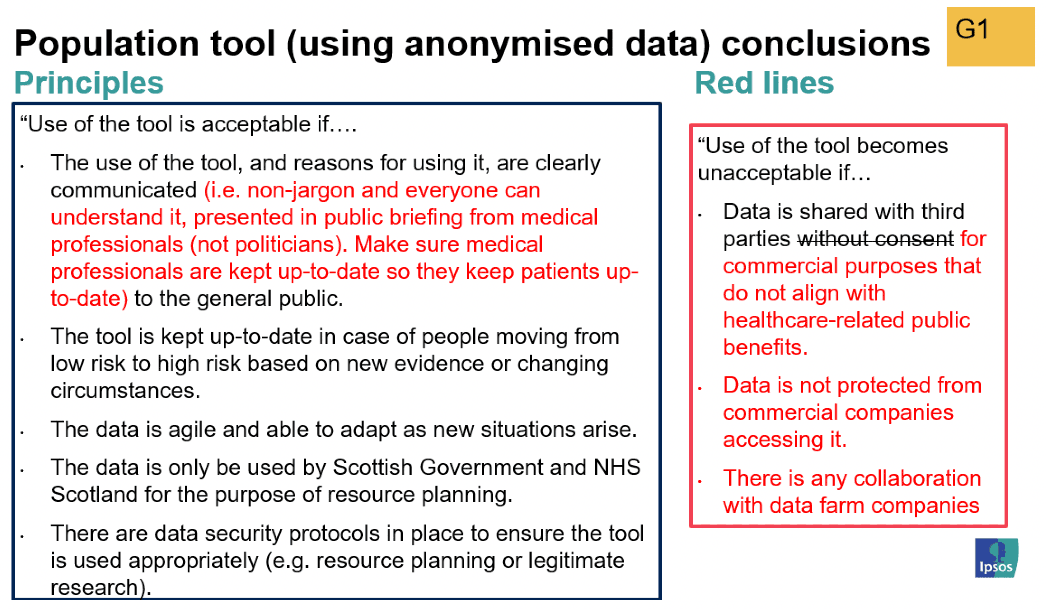
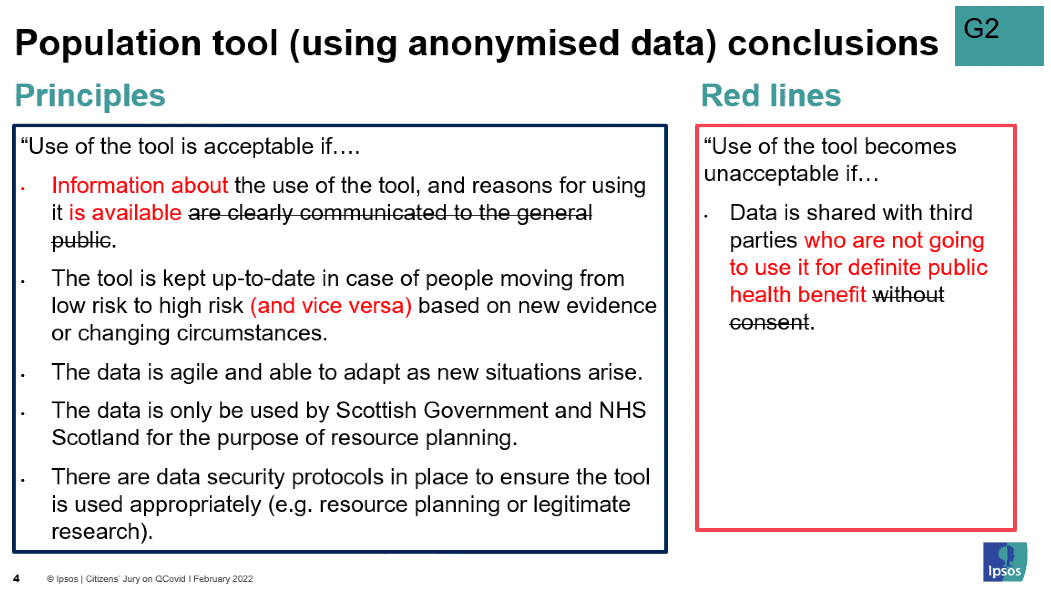
Population tool (anonymised) – group edits
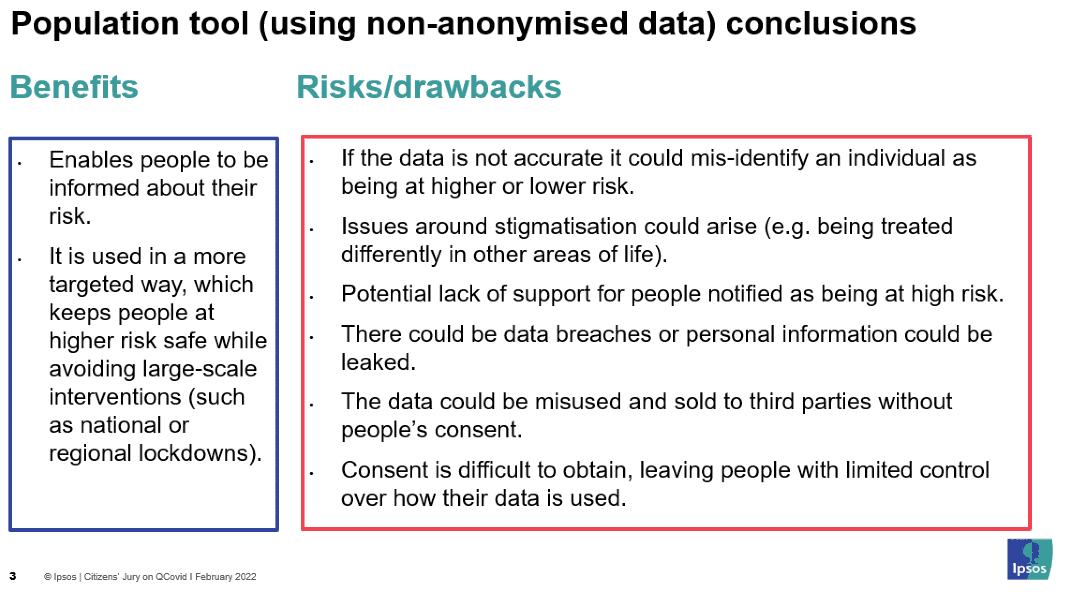
Population tool (non-anonymised) – group edits
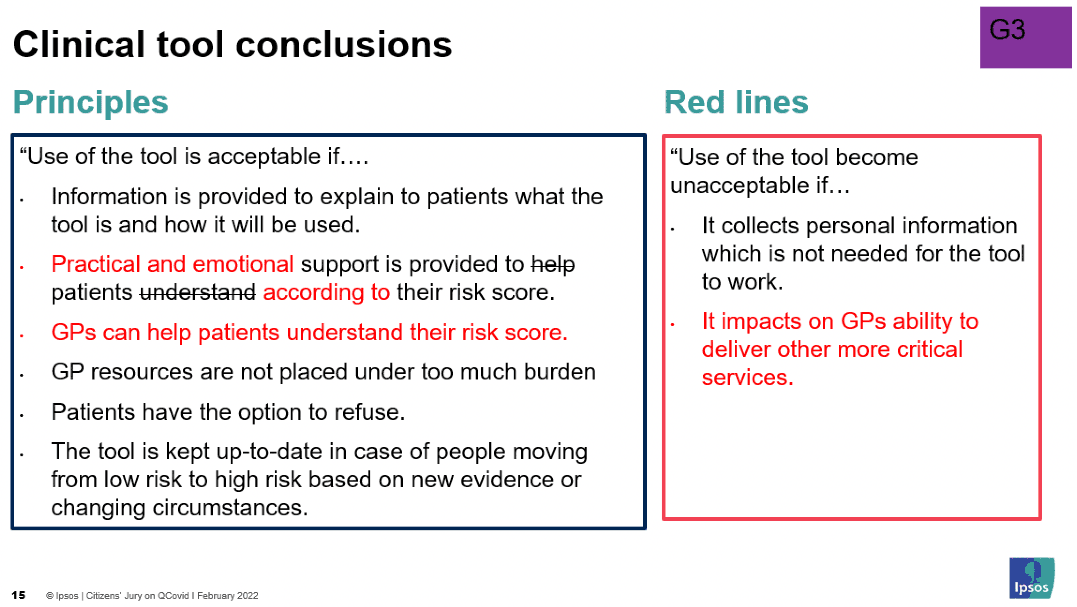
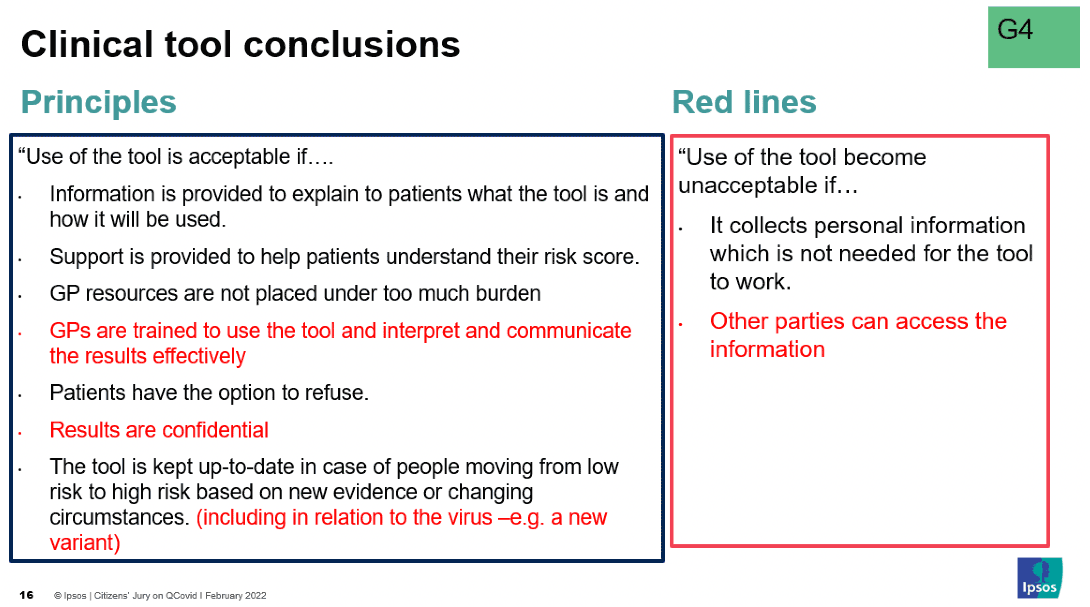
Clinical tool – group edits
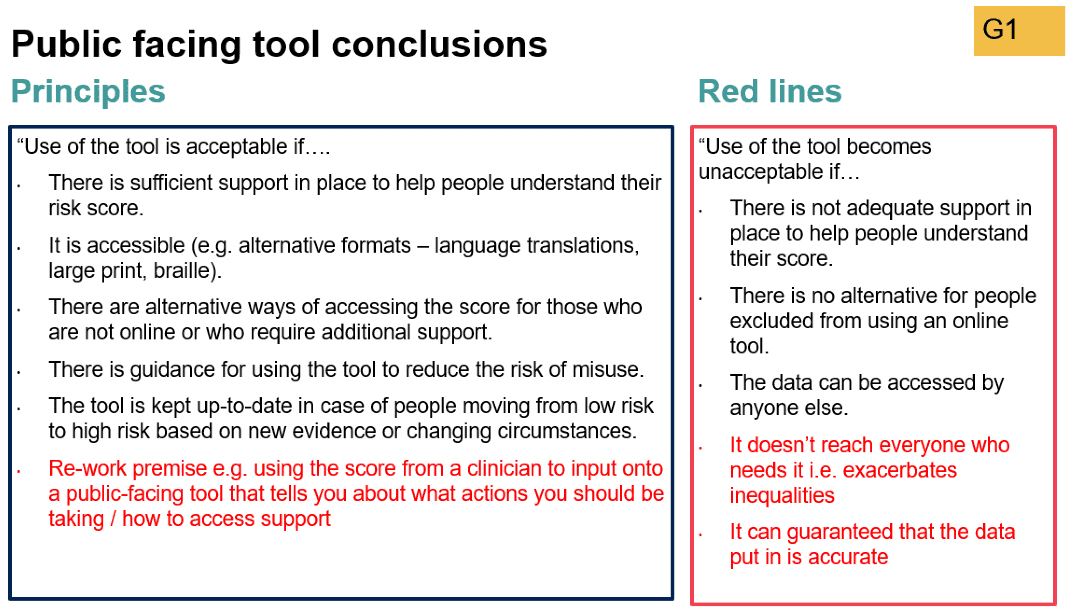
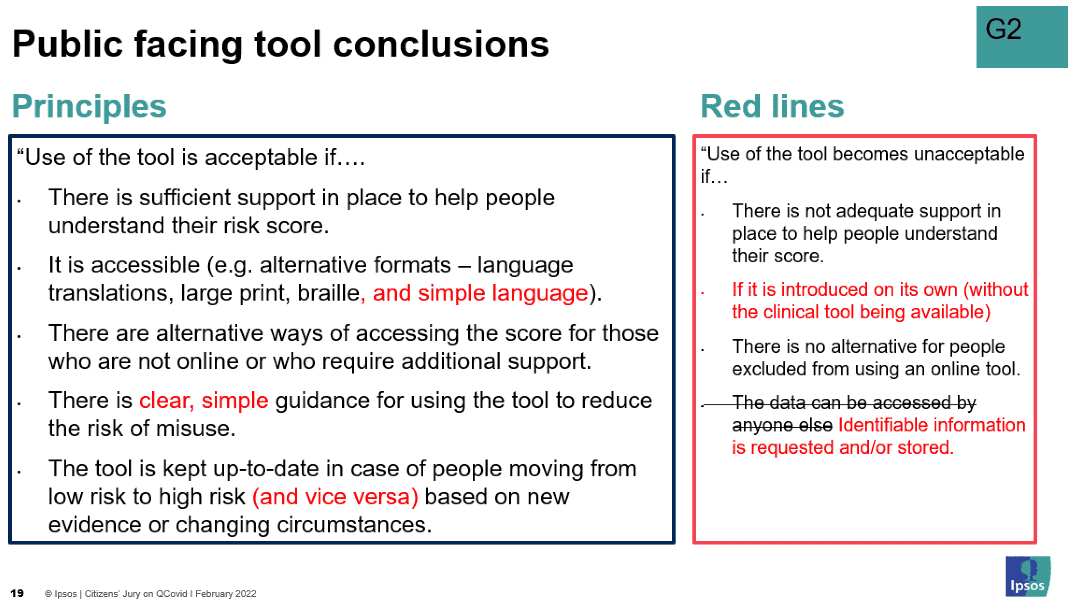
Public-facing tool – group edits
Summary of jury's principles and red lines for each tool
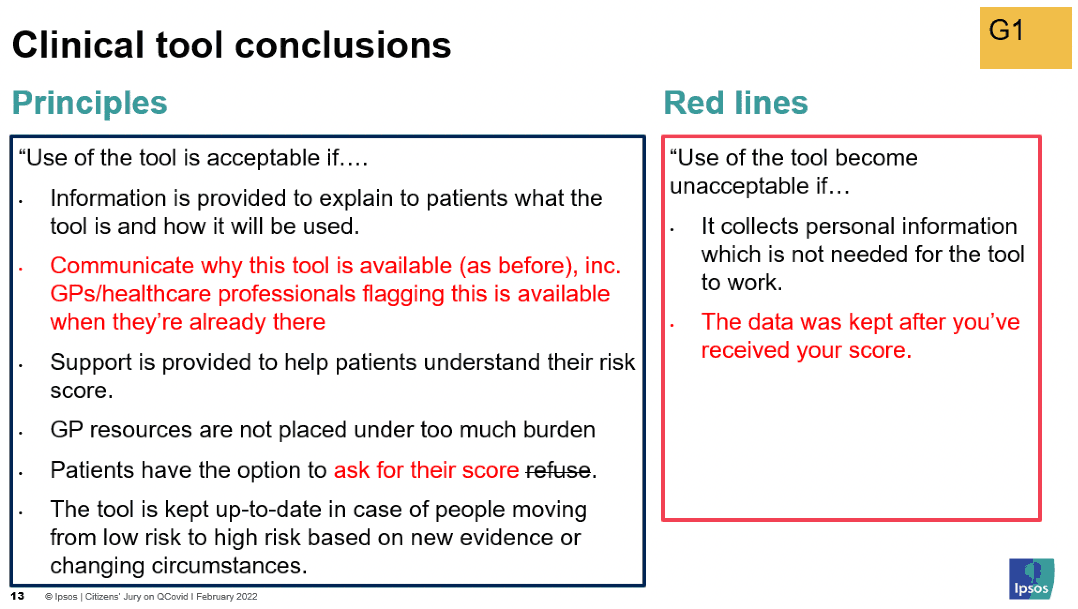
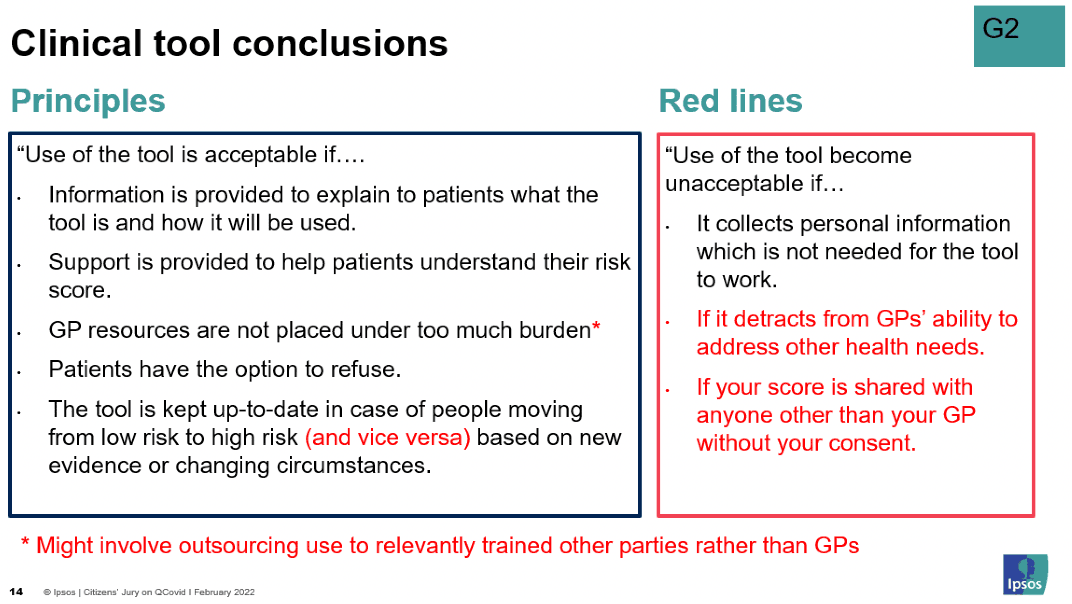
Clinical tool
Use of the tool is acceptable if:
- Information is provided to explain to patients what the tool is and how it will be used.
- It is communicated why this tool is available, including via GPs (or other healthcare professionals) to flag that it is available when with a patient.
- Practical and emotional support is provided to help patients according to their risk score.
- GPs (or other healthcare professionals) can help patients understand their risk score.
- GP resources are not placed under too much burden (which may involve outsourcing to relevantly trained health professionals rather than GPs).
- GPs (or other healthcare professionals) are trained to use the tool and interpret and communicate the results effectively.
- Patients have the option to ask for their score (and to refuse the option to discover their score).
- Results are confidential.
- The tool is kept up to date in case of people moving from low risk to high risk (and vice versa) based on new evidence or changing circumstances (including in relation to the virus e.g. a new variant).
Use of the tool becomes unacceptable if:
- It collects personal information which is not needed for the tool to work.
- The data is kept after you've received your score.
- If it detracts from GPs' ability to address other, more critical, health needs.
- If your score is shared with other parties (i.e. anyone other than your GP) without your consent.
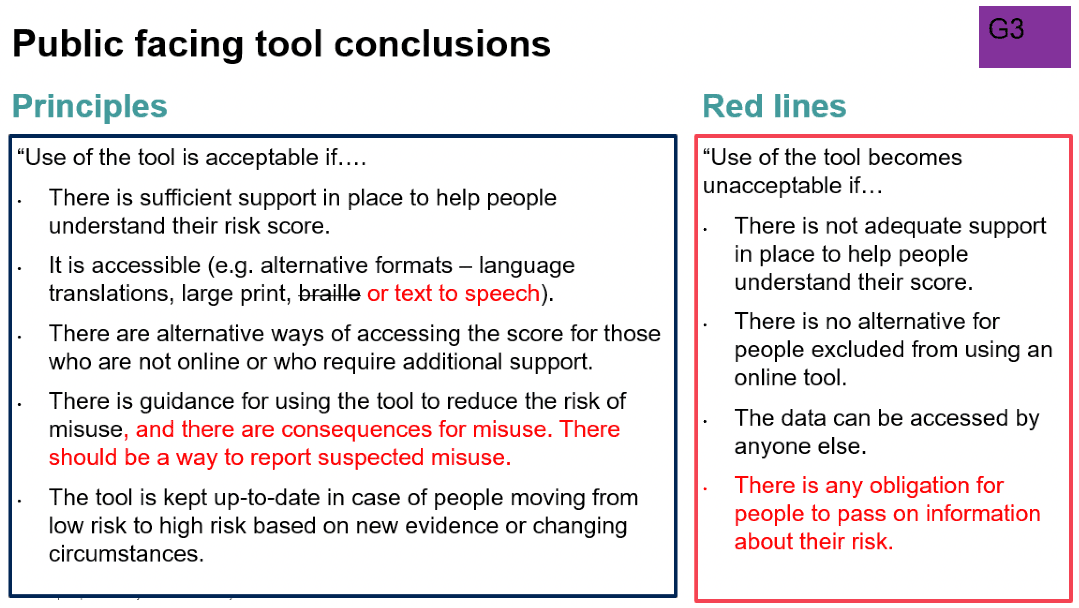
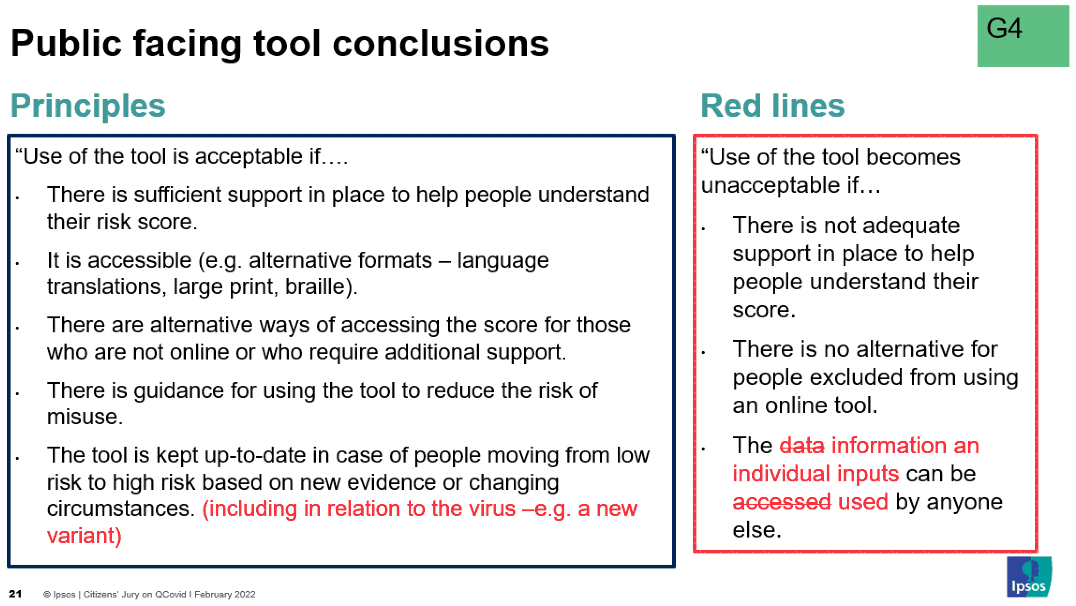
Public-facing tool
Use of the tool is acceptable if:
- There is sufficient support in place to help people understand their risk score.
- It is accessible (e.g. alternative formats – language translations, large print, braille or text to speech, and simple language).
- There are alternative ways of accessing the score for those who are not online or who require additional support.
- There is clear, simple guidance for using the tool to reduce the risk of misuse, and there are consequences for misuse along with a way to report suspected misuse.
- The tool is kept up to date in case of people moving low risk to high risk (and vice versa) based on new evidence or changing circumstances (including in relation to the virus e.g. a new variant).
Use of the tool becomes unacceptable if:
- There is not adequate support in place to help people understand their score.
- It is introduced on its own (without the clinical tool being available).
- There is no alternative for people excluded from using an online tool.
- The information an individual inputs can be accessed and/or used by anyone else.
- Identifiable information is requested and/or stored.
- It doesn't reach everyone who needs it i.e. exacerbates inequalities.
- There is any obligation for people to pass on information about their risk score.
- It can be guaranteed that the data put in is accurate.
- Note that the group who deliberated this final "red line" recognised this would not be plausible without a medical professional present, at which point it becomes the clinical tool. They therefore suggested changing the intended use of the public-facing tool to maintain intentions of empowerment but reduce the risk e.g. using the score from a clinician, provided using the clinical tool, to input onto a public-facing tool that provides information about actions that should be taken and how to access support.
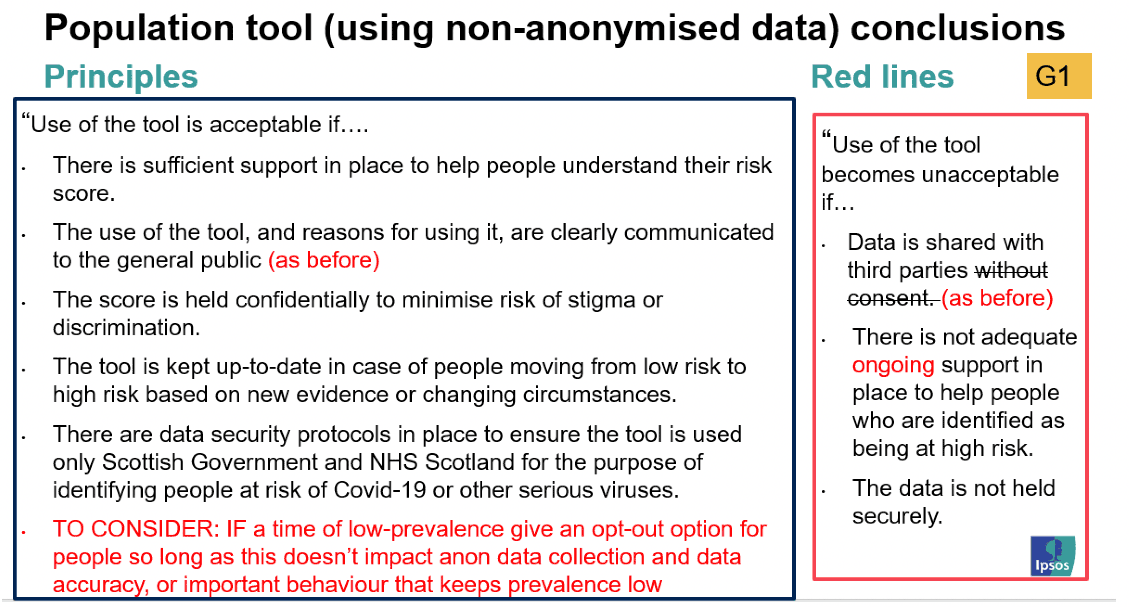
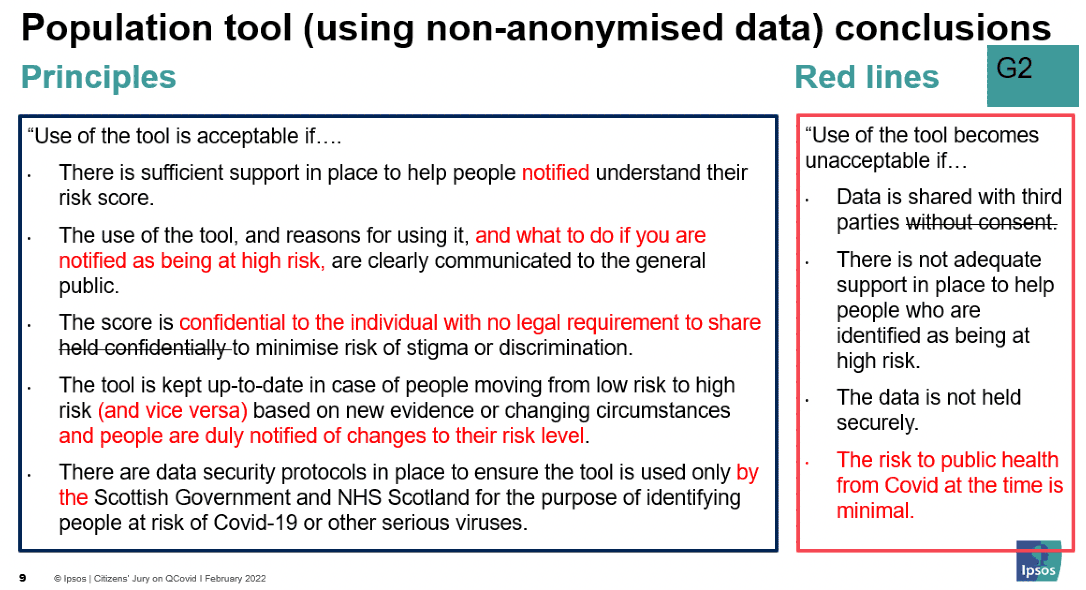
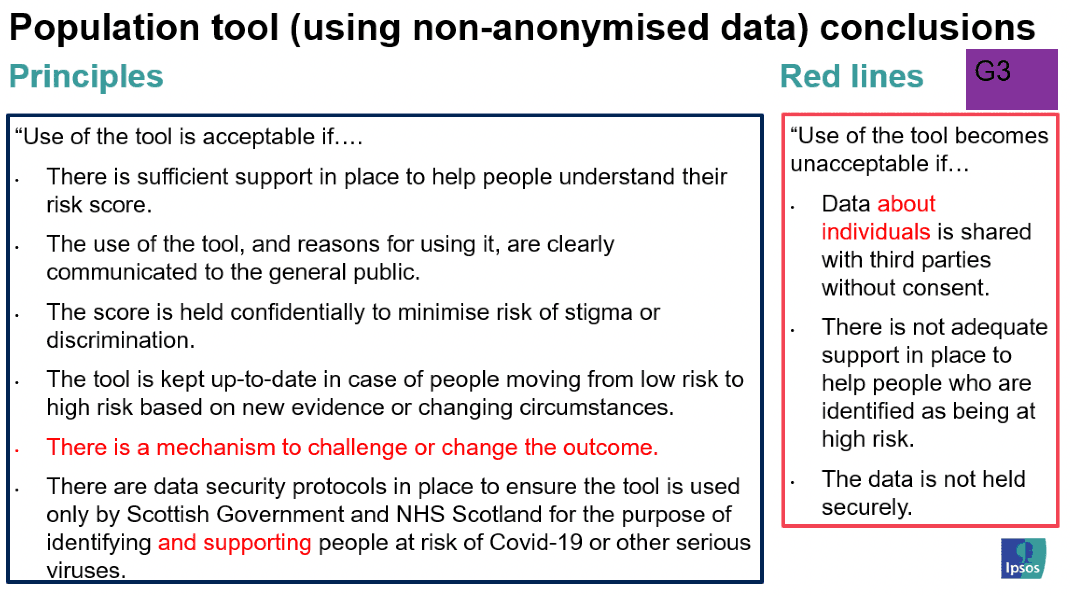
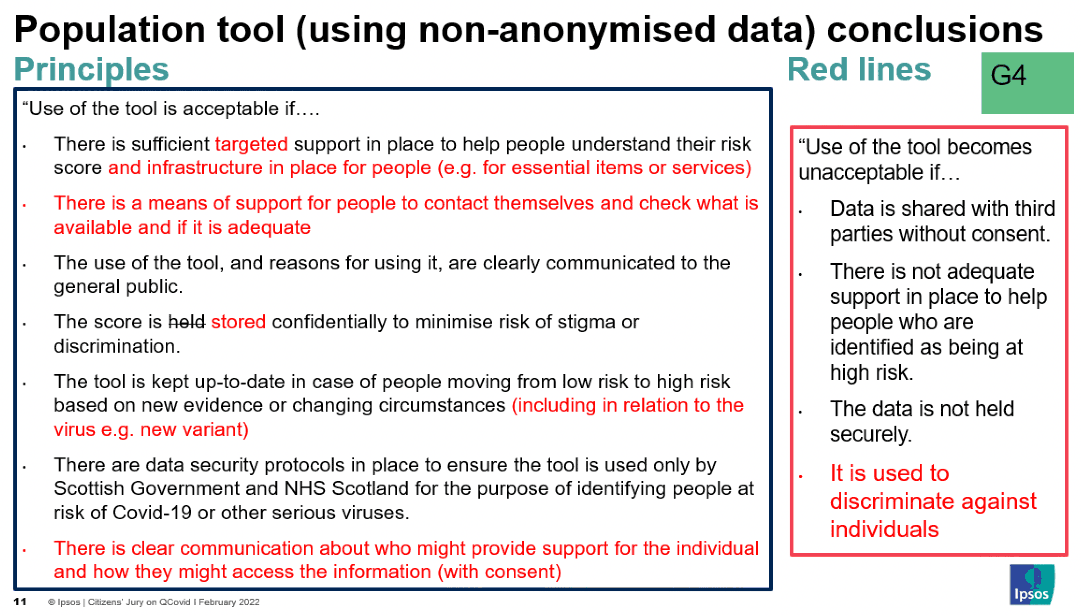
Population tool (using non-anonymised data)
Use of the tool is acceptable if:
- There is sufficient targeted support in place to help people notified understand their risk score and infrastructure in place for people (e.g. for essential items or services).
- There is a way for people to access further support if needed.
- Information about the use of the tool, and reasons for using it, and what to do if you are notified as being at high risk, is available and clearly communicated to the general public i.e. without jargon.
- The score is stored confidentially to the individual, with no legal requirement to share, to minimise risk of stigma or discrimination.
- The tool is kept up to date in case of people moving from low risk to high risk (and vice versa) based on new evidence or changing circumstances (including in relation to the virus e.g. new variant), and people are duly notified of changes to their risk level.
- There is a mechanism to challenge or change the outcome.
- There are data security protocols in place to ensure the tool is used only by the Scottish Government and NHS Scotland. In the case of QCovid®, this would be for the purpose of identifying and supporting people at risk of Covid-19 or other serious viruses.
- There is clear communication about who might provide support for the individual and how they might access the information (with consent).
- Note that, while this was included as a principle, one group deliberated (without reaching consensus) the potential for including an opt-out option for people, as choice is important in terms of rights and building trust, so long as this doesn't impact anonymous data collection and data accuracy or important behaviours that keeps prevalence low.
Use of the tool becomes unacceptable if:
- Data about individuals is shared with third parties for purposes that do not align with healthcare-related public benefits relating to the pandemic.
- There is not adequate ongoing support in place to help people who are identified as being at high risk.
- The data is not held securely.
- The risk to public health from Covid-19, or another virus, at the time is minimal.
- It is used to discriminate against individuals (e.g. in the workplace or in accessing services such as insurance).
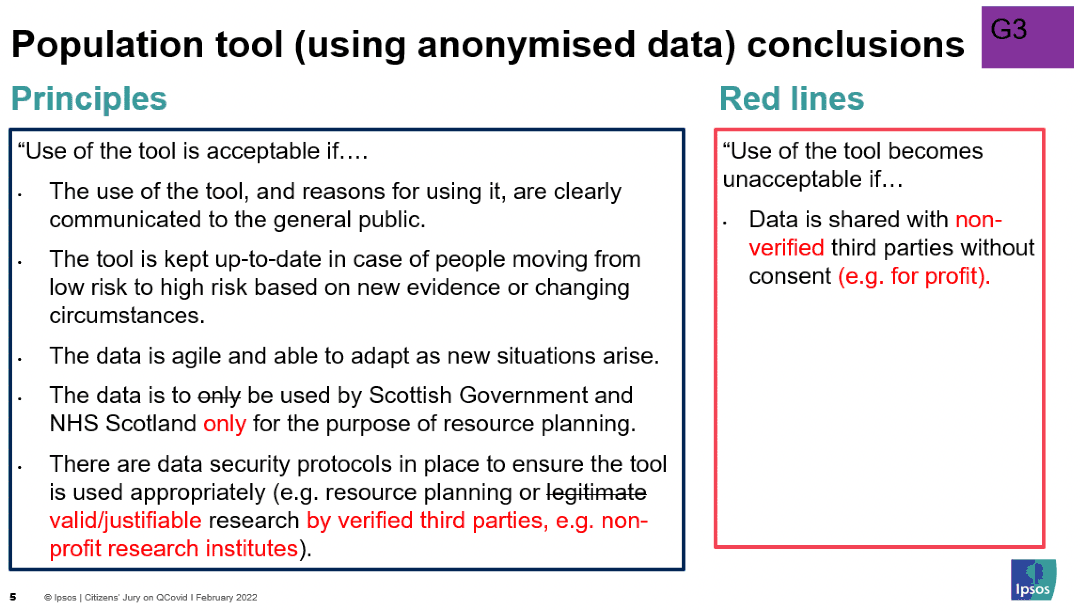
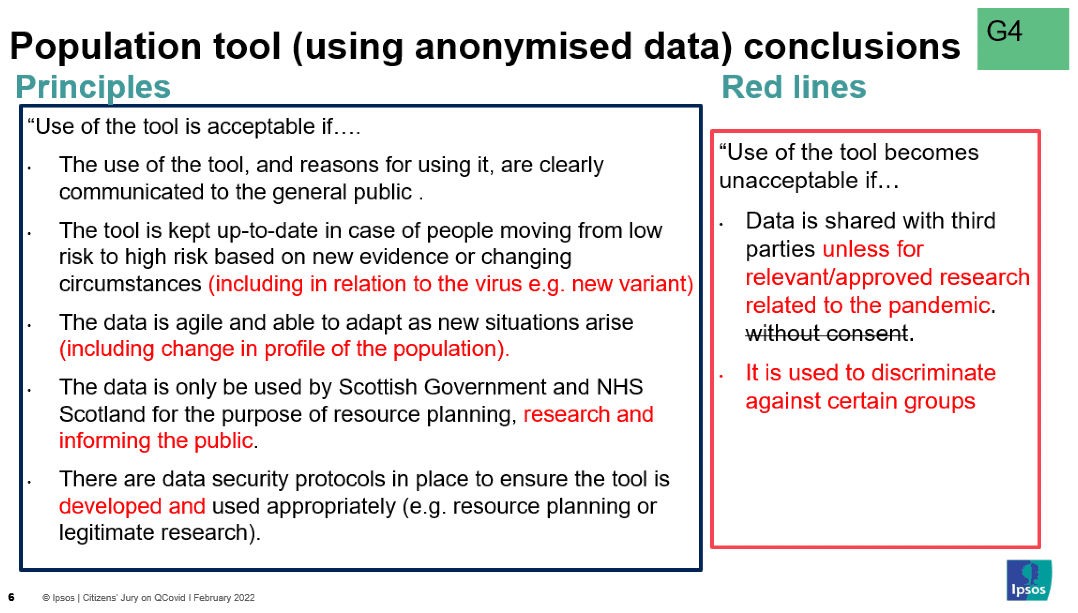
Population tool (using anonymised data)
Use of the tool is acceptable if:
- Information about the use of the tool, and reasons for using it, is available and clearly communicated to the general public i.e. without jargon.
- Note that some felt the information should be available where others felt it should be presented i.e. during a public briefing by a medical professional. Some also felt medical professionals should be kept up to date in order to keep their patients up to date.
- The tool is kept up to date in case of people moving from low risk to high risk (and vice versa) based on new evidence or changing circumstances (including in relation to the virus e.g. new variant).
- The data is agile and able to adapt as new situations arise (including change in profile of the population).
- The data is to be used by Scottish Government and NHS Scotland only for the purpose of resource planning, research and informing the public.
- There are data security protocols in place to ensure the tool is developed and used appropriately (e.g. resource planning or valid/justifiable research by verified third parties e.g. non-profit research institutes).
Use of the tool becomes unacceptable if:
- Data is shared with third parties for purposes that do not align with healthcare-related public benefits relating to the pandemic.
- Data is not protected from commercial companies accessing it.
- There is any collaboration with data farm companies.
- It is used to discriminate against certain groups (e.g. being denied access to certain services based on age or ethnicity).
Contact
Email: shielding@gov.scot
There is a problem
Thanks for your feedback