Chief Medical Officer for Scotland’s Annual Report summary 2017-2018: annex
The Chief Medical Officer's A Summary of the Health of the Nation provides data on some of the key issues related to Scotland’s health.
Priority 4: A Scotland Where We Reduce The Use of and Harm From Alcohol, Tobacco and Other Drugs
We need to reduce the harm caused by smoking, drinking and drugs in Scotland. The number of people using these substances and the harm caused to them and those around them can be minimised.
Substance use is an important contributor to Scotland's persisting health inequalities. Smoking, drinking and drug use continue to cause high levels of harm to individuals, families and communities across Scotland, with these harms experienced most by those living in disadvantaged circumstances. This section presents some key indicators that illustrate the impact of substance use on health.
Smoking
In 2017, approximately one in five (18%) adults smoked in Scotland, a fall from 28% in 2003. This coincides with an increase in the percentage of adults reporting that they had never smoked regularly or at all, from 50% in 2003 to 56% in 2017. Data from the Scottish Adolescent Lifestyle and Substance Use Survey (SALSUS) also shows a steady decline in the percentage of 13 and 15 year olds reporting as regular smokers.[9]
Despite these positive trends, smoking remains a leading cause of preventable disease and premature death. In 2017, 9,332 deaths among those aged 35 years and over in Scotland were estimated to be attributable to smoking[10]. There are also stark inequalities in deaths caused by smoking, with rates in the most deprived areas in Scotland being four times higher than in the least deprived areas. Despite the decline in smoking-attributable deaths occurring across all Scottish Index of Multiple Deprivation (SIMD) groups, relative inequalities have widened over time.
Alcohol
Between 2001 and 2013, the rates of death due to alcohol-specific causes (i.e. wholly attributable to alcohol) fell in Scotland, with the greatest absolute decline among those living in the most deprived areas. However, in recent years, this downward trend has not continued and the decline in inequalities in alcohol-specific death rates has now plateaued[11] (Figure 7).
Figure 7: Age standardised death rates from alcohol-specific causes by deciles of SIMD score for Scotland 2001-2017
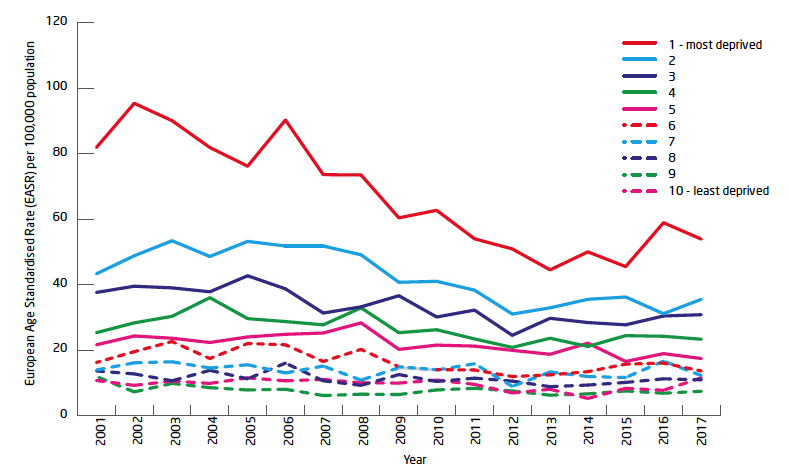
Source: National Records of Scotland[11]
- In 2017, 1,120 people died in Scotland from alcohol-specific causes, an average of 22 people per week. The rate of deaths caused by alcohol was more than seven times higher in the 10% most deprived areas than in the 10% least deprived areas.
- In recent years, the general trend in alcohol-specific death rates has been upward for both men and women; this has been driven by increases in rates in the older age groups, particularly those aged 55 years and older.
- Rates of alcohol-specific death and alcohol-related hospital stays are around 2.5 times higher in men than in women.[12 ]
- Rates of alcohol-related hospital stays in general acute hospitals in Scotland were over four times higher in 2017/18 than in 1981/82. Since 2007/08, the general trend in alcohol-related hospital stays has been downward, but this has flattened over the last 5 years, remaining high at over 668 per 100,000 population in general acute hospitals in 2017/18.
- In 2017/18, alcohol-related hospital stay rates in general acute hospitals were more than eight times higher for those living in the most deprived areas of Scotland than those in the least deprived areas. Inequality by area deprivation is even more marked for alcohol-related admissions to psychiatric hospitals: stay rates were more than 12 times higher in the most deprived decile.
- The Scottish Public Health Observatory (ScotPHO) has estimated that alcohol consumption accounts for about 8% of the overall burden of disease in Scotland.
- Alcohol sales provide the best measure of population alcohol consumption levels in Scotland. In 2017, 10.2 litres of pure alcohol were sold per adult in Scotland. This is equivalent to 19.6 units per adult per week, which is 40% more than the low risk drinking guidelines of 14 units a week set by the UK Chief Medical Officers.[13] Per adult sales in Scotland were 14% higher than in England and Wales. This was largely due to more alcohol being sold at lower prices in the off-trade (supermarkets and other off-licences) in Scotland.
Drug Use
Figure 8: Numbers of drug-related deaths (DRDs) by type of drug implicated in Scotland for 2000-2017
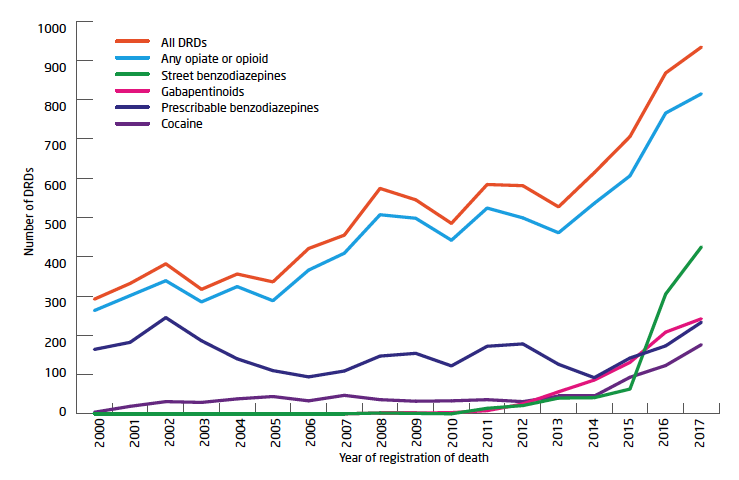
Source: Information Request from National Records of Scotland with ISD definitions for benzodiazepine categories
Footnotes:
- 'Street benzodiazepines' are benzodiazepines (or metabolites thereof) which are a) not licensed for prescription in the UK or b) thought to have originated from an illicit source due to very low overall levels of prescribing in the UK.
- 'Prescribable benzodiazepines' are benzodiazepines (or metabolites thereof) which are licensed for prescription in the UK, but which may not have been prescribed to the individual who died.
- Gabapentinoids are the drugs gabapentin and pregabalin.
- Multiple drug types may be implicated in , or have potentially contributed to, each death.
- In 2017, there were 934 drug-related deaths (DRDs) in Scotland. This was the highest number ever recorded and a more than threefold increase since 2000.
- Scotland's crude DRD rate is more than twice as high as those of other UK countries and high compared to other European countries. This is in part due to the historically high numbers of individuals with problem drug use in Scotland (estimated at 57,300).[14]
- Drug use disorders are the sixth leading cause of both early death and disability in Scotland and the leading cause of preventable death in 15-34 year olds.[14]
- There is a marked deprivation effect with just over half of those who died having lived in the 20% most deprived neighbourhoods in Scotland.
- Figure 8 shows the number of DRDs in Scotland from 2000 to 2017 by selected drug types implicated in those deaths.
- Opioids were consistently implicated in deaths (86% to 91%) across the time series. From 2014, the implication of three other drug types 'street' benzodiazepines, gabapentinoids and cocaine) began to increase.
'Street' benzodiazepines such as etizolam and alprazolam (Xanax) have been increasingly implicated in DRDs since emerging on UK drug markets in the early 2010s as New Psychoactive Substances (so-called 'Legal Highs'). Though the supply and sale of many of these drugs was banned by the Psychoactive Substances Act 2016, they remain widely available via illicit drug markets. At high doses and when taken alongside opioids, benzodiazepines are a risk factor for DRD due to their respiratory depressant effects. Uncertainties regarding product type, purity and effect profile mean that the risks associated with consumption of unlicensed 'street' benzodiazepines may be higher than for prescribable benzodiazepines.
Gabapentinoids are prescription-only medications licensed for the treatment of neuropathic pain, epilepsy and (for pregabalin only) generalized anxiety disorder. There is growing evidence that, as a consequence of self-reported euphoric effects at high doses (particularly if taken with opioids), gabapentinoids are being used increasingly by people with a drug problem. However, potential side effects such as the reversal of methadone tolerance and respiratory depression mean these drugs are a risk factor for DRD. As a consequence of increasing evidence of diversion, misuse and harm, gabapentinoids became Class C controlled substances under the Misuse of Drugs Act (1971) on 1 April 2019.
There is evidence that cocaine use in the UK has increased in recent years due to a reduction in price and an increase in purity. Concurrently, cocaine-related harms (hospital admissions and deaths) have increased. The Needle Exchange Surveillance Initiative (NESI) reports an increase in injecting cocaine use among people who inject drugs (mainly opioid users) , particularly in Glasgow. This has also led to an increased prevalence of HIV among the population of people who inject drugs in the city (with more than 100 new cases of HIV identified between 2015 and 2017). The health vulnerabilities of Scotland's ageing population of opioid users (a group often with multiple and complex comorbidities) alongside the risk of cardiac arrhythmia (and sudden death) from simultaneous cocaine and opioid use may help explain the increase in cocaine-implicated deaths.
Contact
Email: stephen.fenning@gov.scot
There is a problem
Thanks for your feedback