Scottish allied health professions public health strategic framework implementation plan: 2022 to 2027
In 2019, the first UK wide Allied Health Professions (AHPs) Public Health Strategic Framework 2019-2024 was published by all four nations, intended to help AHPs and partners to further develop their role in public health. Thereafter, each nation agreed to develop their own implementation plan.
Introduction
The first UK wide Allied Health Professions (AHPs) Public Health Strategic Framework 2019-2024 was published in 2019.[1] The strategic framework sets out a united, collective approach to Public Health for AHPs across all four nations with input from professional bodies and other collaborating partners.
This Strategic Framework committed the Scottish Government to work with key stakeholders to develop and publish an implementation plan to provide more detail on delivery, monitoring and reporting in a Scottish context.
This initial implementation plan signals a key milestone in building on the role of AHPs in public health in Scotland, along with the goals and actions that we aim to take to realise this vision. It is intended to help AHPs and their partners including NHS Boards to progress, support and enable themselves to improve public health in the population, reduce health inequalities and encourage self-management and self-care through early intervention and prevention. This document is a first for Scotland in that it brings together the public health impact of the AHP practice in partnership with professional organisations, NHS Boards and Public Health Scotland.
The plan has been written from the perspective of the collaborating partners, and references to "we" have been made to reflect the collective and unique roles of all partners to realise our vision.
This plan has been prepared by the Scottish Government with input from a range of stakeholders including members of a fixed-life stakeholder reference group. The group was established to advise on and support implementation of the UK wide Strategic Framework by considering significant priorities, key deliverables and lead partners for inclusion in the plan. The process behind the implementation plan's creation are described in the 'Our Approach' section and the membership of the Stakeholder Reference Group who oversaw its development is presented in Appendix 1.
Areas for action by Scottish Government, NHS Boards, AHP leaders and AHPs are presented with the expectation that local implementation plans will be made in support of this. Implementation will mark a positive step in the quest to maximise the AHP impact to population health and a National Oversight Group in reviewing progress will be key to enable this.
Allied Health Professionals
AHPs encompass a broad group of 14 health professions, who make up the third largest workforce in the NHS Scotland. These 14 professions include: Art Therapists, Diagnostic Radiographers, Dietitians, Dramatherapists, Music Therapists, Occupational Therapists, Orthoptists, Paramedics, Physiotherapists, Podiatrists, Prosthetists and Orthotists, Speech and Language Therapists and Therapeutic Radiographers.
AHPs support people of all ages to live healthy, active and independent lives. The breadth of AHP skills and their reach across the life course, third sector, communities and in health and care settings makes them ideally placed to be leaders within public health improvement. Their expertise is used to support prevention, self-management and promote wellbeing.
Defining Public Health
The Faculty of Public Health has defined public health as the science and art of preventing disease, prolonging life and promoting health through the organised efforts of society.[2] It seeks to support and empower people to improve their health and focuses on the wider determinants of health, prevention and early intervention to help achieve this aim.
Within the UK AHP Strategic Framework, co-designed with members including the Scottish Government, is a model that has been designed to be relevant to the roles of AHPs. This model spans four broad areas: wider determinants, health improvement, population healthcare and health protection.
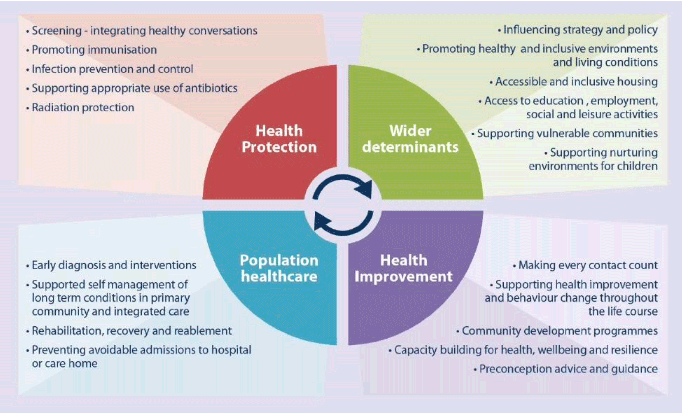
Source: UK AHP Public Health Strategic Framework 2019-2024 PDF (ahpf.org.uk)
The following are examples of how AHPs already contribute to public health; this will vary by profession and is not intended to be exhaustive:
- Health Improvement - describes the work to improve the health and mental wellbeing of individuals, communities or populations through enabling and encouraging healthy lifestyle choices and developing resilience.
- Population healthcare – aims to maximise value, equity and good outcomes by focusing on the needs of the population and delivering person centred services across the entire health and care system.
- Health Protection – aims to protect the population's health from communicable diseases and other threats, while reducing health inequalities
- Wider determinants – working across different communities, especially those that are in areas of higher deprivation and therefore likely to have multiple risk factors for higher health inequality. Also ensuring access to positive influences on health such as leisure and community resources.
- Older people - prevention and early intervention is at the forefront of support services for older people. Making day-to-day living easier and supporting older people to have full and meaningful lives by planning for the ageing process and preventing, delaying or managing crises.
- Reducing harm from alcohol, tobacco and drugs - this includes health promotion, prevention, early intervention, treatment, and recovery focused approaches.
- Antimicrobial resistance and Infection prevention and control for Allied Health practices implements an infection prevention and control strategy to minimise the spread of infectious agents.
- Children and young people – prevention and early intervention is at the heart of children's services. AHPs works with children and young people, their parents, carers, families, stakeholders and communities to improve their well-being and outcomes.
Layers of public health and the role of AHPs
Public Health can impact different levels of society, which can be regarded as layers. These layers refer to sections of society and cover the individual level, community and whole populations:
1. Individual – This is the provision of care to individuals across all settings, taking into account their family, social and environmental links together with consideration of the wider determinants of health. This is where AHPs have the opportunity to apply their breadth of skills and work across settings through early intervention and prevention, by providing advice and support to individuals at risk regarding preventable causes of illness or premature mortality.
2. Community – This is the work with the public and communities to improve health and well-being and reduce inequalities. Developing resources to support the improvement of health and wellbeing and the reduction of inequalities within communities.
3. Population – The health outcomes of a group of individuals, often geographical populations such as nations or communities, but also other groups such as ethnic groups, disabled persons, prisoners, or any other defined group. Ensuring the right infrastructure and processes are in place is important to support regional and national strategies to improve health and wellbeing and reduce inequalities.
AHPs make a significant contribution across each of these levels of public health through their routine work providing integrated care in health, social care, education, voluntary sectors and private sector settings. Our vision is that AHPs will continue to demonstrate leadership and impact with renewed effort to reduce health inequalities, enable and empower people and communities to take positive action for health and wellbeing.
The broad social and economic circumstances that together determine the quality of the health of the population are known as the 'social determinants of health.'
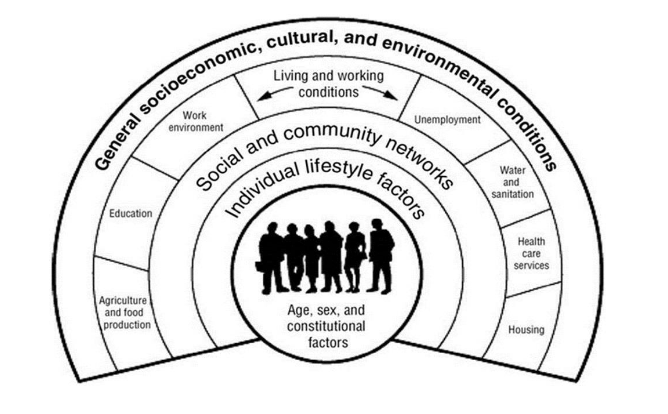
Source: Dahlgren and Whitehead (1991)
This shows:
- personal characteristics occupy the core of the model and include sex, age, ethnic group, and hereditary factors
- individual 'lifestyle' factors include behaviours such as smoking, alcohol use, and physical activity
- social and community networks include family and wider social circles
- living and working conditions include access and opportunities in relation to jobs, housing, education and welfare services
- general socioeconomic, cultural and environmental conditions include factors such as disposable income, taxation, and availability of work.
It is recognised action on health inequalities will require AHP action across all of the social determinants of health and across the life course.
Contact
Email: abigail.parkin@gov.scot
There is a problem
Thanks for your feedback