Coronavirus (COVID-19) asymptomatic testing programme: evaluation - November 2020 to June 2021
This evaluation report examines the asymptomatic testing programme in Scotland. It covers the period November 2020 to June 2021.
Attitudes and Behaviours
Introduction
This chapter explores attitudes towards and behaviours surrounding testing. All pathways have been able to return some data on attitudes and behaviours, though this varies in extent and quality of information.
Where surveys or other research into attitudes and behaviours has been undertaken it is important to bear in mind that this is not likely to be fully representative of the population being tested. Those people who have responded to the surveys are likely to be those who are more likely to be participating in testing and represent a more "engaged population". The only exception to this is the Scottish Government polling undertaken by YouGov, which provides a representative sample of Scottish adults aged 18 and over.
Why are people taking up the offer of testing?
There are a wide range of reasons for getting tested, including:
- To generally reassure themselves that they do not have Covid-19
- Before/after socialising
- As part of workplace testing
- To prevent further outbreaks
- To protect the local community
- To keep and enable freedoms
- If have been in contact with a case or have symptoms (though this evaluation focuses on pathways designed for asymptomatic testing)
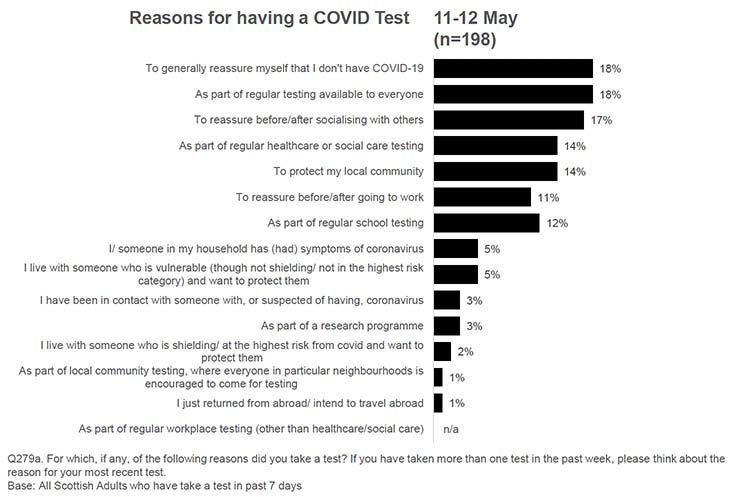
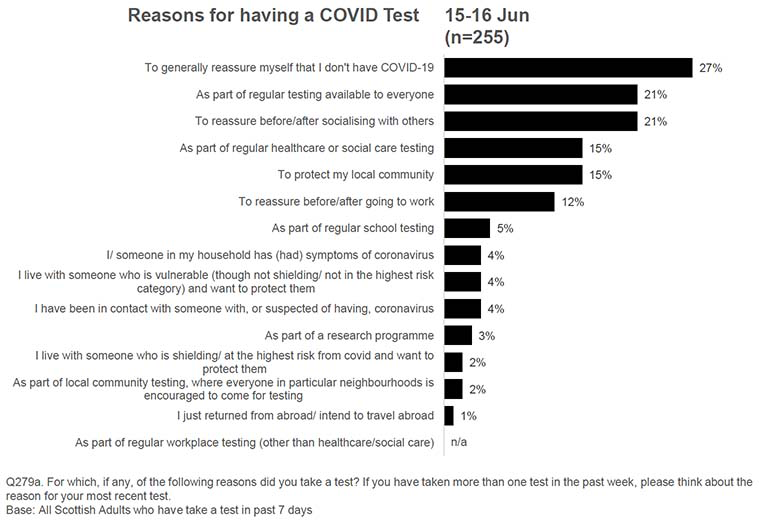
Evidence from the Scottish Government's regular polling[16] on reasons why people take a test can be seen below, covering these main reasons (for both symptomatic and asymptomatic testing), over time, in Figures 9, 10, and 11. More detail on four key themes for those taking up asymptomatic testing across the pathways is provided below.
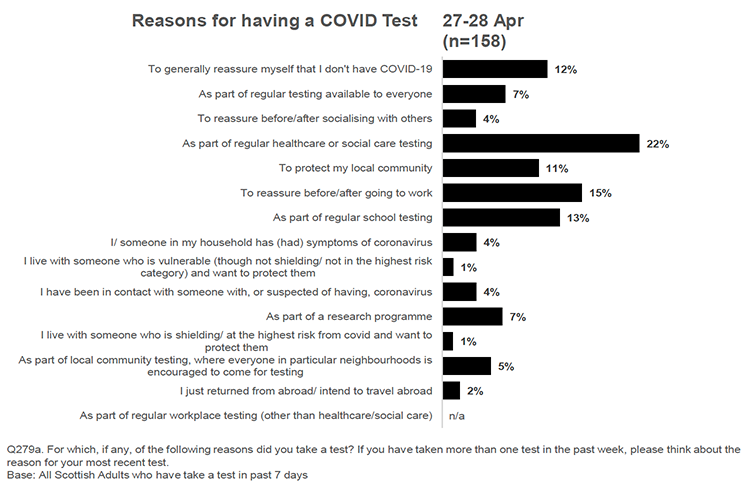
(Source: Scottish Government polling data – please note, this question covers both symptomatic and asymptomatic test)
(Source: Scottish Government polling data – please note, this question covers both symptomatic and asymptomatic test)
(Source: Scottish Government polling data – please note, this question covers both symptomatic and asymptomatic test)
Reassurance
Individuals are concerned about their risk of catching Covid-19 and are reassured by having access to asymptomatic testing to keep themselves, their families, and communities and workplaces safe. This relates to a desire to control the virus and reduce outbreaks. Indeed, 63% of participants responding to Scottish Government regular polling said they were reassured that universal testing is now open to everyone (1-2 June). Individuals taking part in the prisons pathway noted that they were not yet vaccinated and testing provided reassurance in the meantime. Please note again the time period that this evaluation covers: November 2020 to June 2021. Different cohorts were at different stages of being invited to vaccination over this period.
Reassurance was key to the highest risk group (formerly described as 'shielding') who noted that one of the main reasons to use regular testing was to reduce anxiety and that the universal testing offer had helped in this regard. Sixty-two percent of highest risk respondents reported a reduction in anxiety and 68% said their household's anxiety levels had reduced. Other benefits connected with reassurance were also mentioned:
- It offered me peace of mind and reassurance (70%)
- It made me feel more protected (55%)
- It helped me find out quickly if I had Covid-19 or not (55%)
- It helped me find out quickly if someone in my house had Covid-19 or not (46%)
Research conducted in England shows a similar sense of relief and reduced feelings of anxiety among those participating in asymptomatic testing, with participants feeling more confident going to school or work, or visiting vulnerable family and friends, knowing they were not spreading the virus. For more details, please refer to Annex B (p. 66). See also p. 80 for a study highlighting how testing is often used as a reassurance after risky situations rather than as a screening endeavour.
Protecting others
Testing was cited as an important way of providing reassurance for the individual, but also of protecting others from Covid-19 infection. This could be family, friends, the local community, or workplace. Eighty-three percent of those responding to the school staff survey said they participate in regular asymptomatic testing to keep themselves and their household safe and 76% said it was to keep their school/childcare community safe. Seventy-three percent of children and young people who responded to the survey for secondary school pupils said they participate to keep themselves and their families safe (with a lower percentage saying it was to keep their school community safe – 53%). Staff in the prisons testing pathway also wanted to act as a role model for prisoners and in doing so encourage greater testing uptake and protection across the prison estate.
Civic duty and the altruistic motivations of engaging in testing have also been identified as key drivers to getting tested in other UK studies. Annex B (p. 75 and pp. 79-80) presents some examples of how decisions to engage in testing programmes have been related by participants to pride in knowing that they were contributing to a collective pandemic response, a desire to protect the community and a belief that testing could help the return to normality.
Practical considerations
There were also more practical reasons for taking part in asymptomatic testing. Participants in the prisons pathway (which provides asymptomatic PCR testing) noted that they may require a negative result as proof when going elsewhere (at the time this was a potential consideration for travel, for example). The Community Testing pathway also found that a reason some people attended a community test site was that they wanted to learn how to use the test kit under specialist guidance, before potentially doing so themselves at home via another pathway.
Encouraged or required testing
Work is a key place for people to test and expectations from work encourage people to stick with the demands of regular twice- (and for some pathways, thrice-) weekly testing. For example, 52% of those responding to the school staff survey said they took part in testing because they had been encouraged to do so by the school and 90% of Social Care workers responding to the relevant evaluation survey were testing twice weekly and most recorded their results. The research from the community testing pathway also found that being 'sent' for a test by a workplace (or the NHS) was a reason given for attendance.
Enablers of testing
Some pathways mentioned specific enablers of testing. These made testing easy and convenient. Participants in the prisons pathway noted many of these, saying they: found it easy to book tests; all their queries had been answered; they were well supported to carry out the first test; and they could test quickly, privately and get results within 24 hours. Social Care staff said their employers had supported them to work through any barriers to testing they encountered, thereby enabling them to continue testing.
Why are people not taking up the offer, or testing less frequently?
As with reasons for testing, the reasons for not taking up the various offers of asymptomatic testing are wide-ranging. These have been pulled into relevant themes below. To note, community testing is likely always to have mixed take-up as the amount of testing undertaken will depend on prevalence in local areas – it is not expected to maintain a constant steady rate as the aim is to target communities with increased or enduring transmission, or to protect at risk communities.
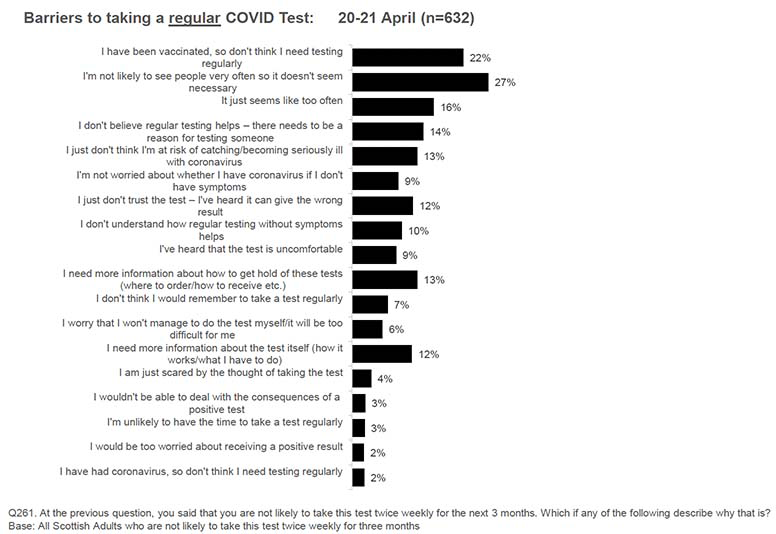
Perceived lack of risk from the virus
Across pathways and for testing in general, vaccination is emerging as a key reason people give for not seeing themselves as requiring regular asymptomatic testing. This can be seen in Scottish Government polling, where 28% of people at 18-19 May selected this reason, but there was evidence in almost all pathways of this viewpoint.
Furthermore, the Scottish Government polling found that people may not see themselves as at great risk because they do not see others often or because they think they are not at great risk of negative outcomes even if they do contract the virus. See Figures 12 and 13 for views over time.
The link between testing and risk perception is further explored in the evidence review presented in Annex B. Perceiving oneself to be low risk has been associated with vaccination status, having had Covid-19 in the past and younger age groups (see p. 70). This risk perception does not necessarily correlate with a person's objective risk.
(Source: Scottish Government polling data)
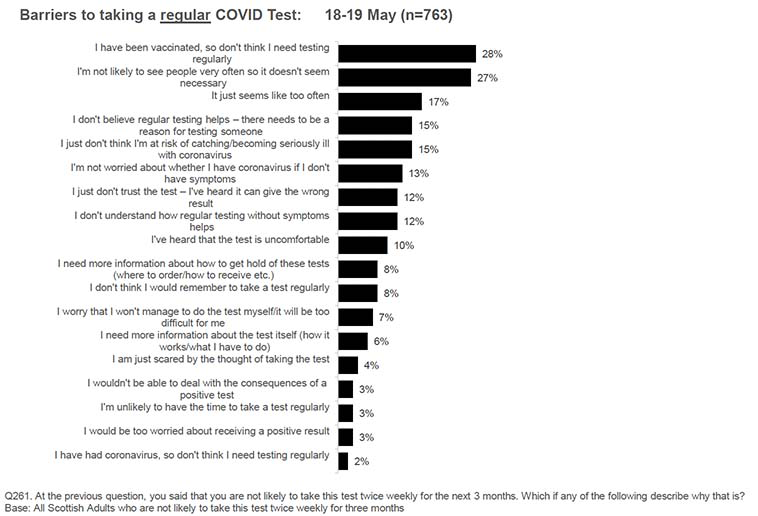
(Source: Scottish Government polling data)
Concerns about the test
Across the Schools, Childcare, Health and Social Care workforce, and Community Testing pathways test discomfort is a consistent theme and a reason for being discouraged from testing or actively giving testing up. Furthermore, concerns about the accuracy of the test were also cited (see more below under 'Navigating the System'). This is also highlighted in the literature which suggests that a test that is seen not only as reliable, but quick, easy to administer, and less uncomfortable has higher chances of being done (see Annex B, p. 78).
The community testing pathway also found that some individuals were concerned about attending for a test because of the fear of infection at sites and on public transport.
Practical considerations
The prisons pathway has seen fairly steady numbers of tests being taken throughout the period of evaluation (see Table 3). Where people signed up but have then not taken part in testing, reasons participants in this research gave are mainly practical, such as forgetting, running out of time on shift, or not being available when the testing was undertaken.
Police Scotland and Scottish Fire and Rescue Service colleagues noted a range of practical considerations, which include those mentioned above but also problems with using the online portal to record results (a common issue across pathways, discussed more below) and not having time/capacity to complete and/or record the result. The issue of time and capacity also emerged from the social care workforce research. The Police Scotland and Scottish Fire and Rescue Service pathway also found that regular testing had resulted in 'testing fatigue'. Police Scotland and SFRS were careful to maintain directive communications encouraging testing and reporting in a communications style known to their staff. NHS Board leads concurred, stating that the main issue for them over the next 6-12 months would be maintaining motivation to test.
Furthermore, people may have been taking the tests, but not recording negative results. This is also a common concern and is discussed in more detail below. Several NHS Boards reported that staff found the results portal difficult to use and it took up too much staff time, leading to staff taking LFD tests but not recording results.
The excessive work burden emerges in the UK and international literature as one of the main barriers to testing. A number of studies discuss how testing programmes in the workplace have resulted in added responsibilities and increased workload for already over-burdened members of staff who are not consistently paid for time to get tested, sometimes resulting in poor adherence to LFD testing protocols. These issues are further explored in Annex B, p. 73 and pp. 74-75.
The University and College pathway also noted a decline in uptake after an engaged start and in often cyclical demand (e.g. demand on Fridays before weekend activities or going home or during local outbreaks). This decline is largely attributable to far fewer students and staff being allowed to return to in-person learning after the Christmas break in January 2021.
In the Schools testing pathway, qualitative feedback from parents suggests that asking pupils to collect tests from a school office may not work well in practice for everyone (e.g. they may forget). Another practical issue raised was that some young people may not have someone at home who can help them to do the tests (or they may lack encouragement at home).
Confusion about pathways, or finding other pathways easier to access, was also mentioned as a reason for not participating within a specific pathway by those in the Prisons, Police and Fire Service, and Community Testing pathways.
Attitudes and understanding
Attitudes towards asymptomatic testing, including a sense of a lack of clarity around the benefits or understanding of the process could have a serious impact on uptake. In the Community Testing pathway there was concern that the benefits of testing are not always clear and, despite strong promotion of testing, this may mean people do not attend. Scottish Government polling found a stable fifth of people report not understanding how regular asymptomatic testing helps to stop the spread of Covid-19.
There is also some evidence arising from research with the highest risk cohort that some of that population may not understand that LFD testing is currently only to be used when asymptomatic. Some responses noted that they only intended to use the tests if they/their household became symptomatic. This is an important point that may extend beyond the highest risk cohort. Though the pathways evaluated here are intended for asymptomatic testing only it is likely that people do not necessarily always use them in this way, potentially using the universal offer, for example, as a means to check symptoms as they emerge. The fact we can see some suggestion of this in the highest risk cohort is particularly important – communications about appropriate and best use of the different tests available is required.
A number of other UK and international studies reported that individuals find it difficult to understand differences between the PCR and LFD tests, why a test is needed in the absence of symptoms, and how and where to get tested. For a discussion of these barriers to testing, please see Annex B (pp. 68-69).
Although Scottish Government regular polling shows that the majority of people can see the theoretical benefits of regular testing, this does not necessarily translate into active participation. For example, looking at the universal offer, 37% of the sample said they had taken up this pathway (29-30 June), but then just 22% of this sub-sample were actually testing twice weekly with 16% using them about once a week, 20% saying they used the tests occasionally when they thought they had a reason to and a further 22% saying they had not yet used the tests at all (some of these people were saving them for a special occasion). This equates to just under one in ten of the Scottish population (8%) using the universal offer as intended (that is twice a week). This increases to 14% if those who test around once a week are also included. Polling data (18-19 May, n=763) found 17% of the Scottish population think twice weekly testing is just too frequent. The wider literature also highlights this issue and the importance of explaining to the public that lateral flow tests are more likely to detect positive cases when testing is frequent. For a detailed discussion on this point, see Annex B (p. 69).
From empirical research undertaken across pathways, it can also be seen there are also those who just do not agree with the testing programme and therefore choose not to participate (for example, seeing it as a waste of NHS resources).
What would encourage testing uptake
When asked what would encourage participants who said they were unlikely to take part in asymptomatic testing to test, similar reasons are cited to those given by those willing to take part in testing: to prevent outbreaks, protect the local community, if local case numbers were high, and to keep or enable freedoms. The most common reason though, is if an individual thought they had been in contact with someone who has had Covid-19. See Figures 14 and 15 for views over time.
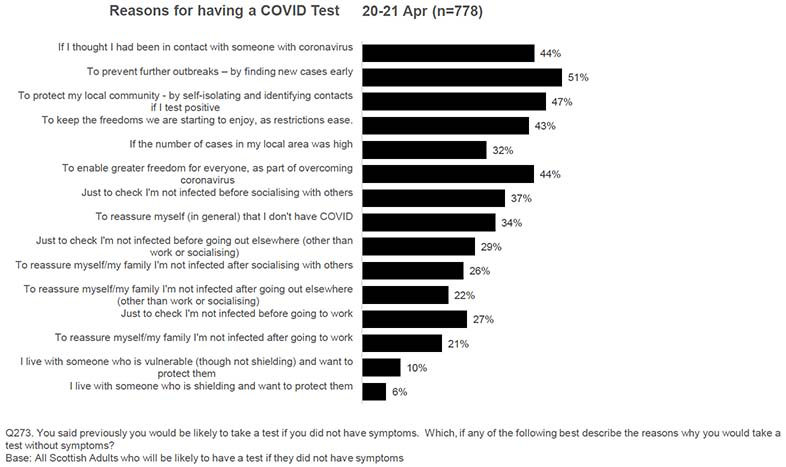
(Source: Scottish Government polling data)
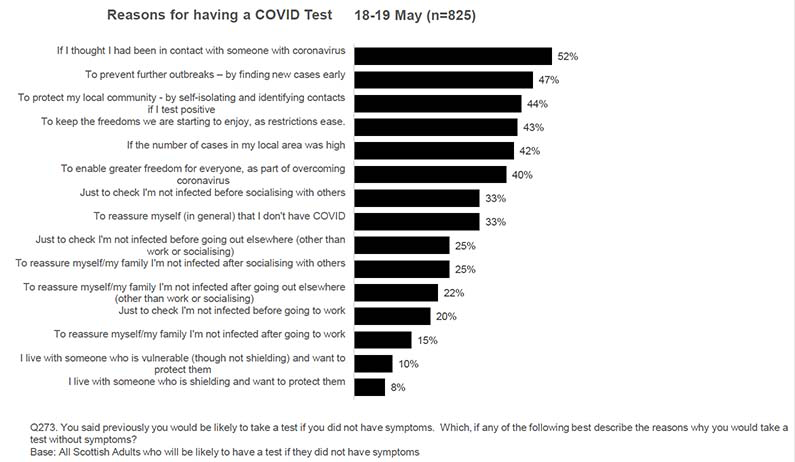
(Source: Scottish Government polling data)
NHS Board leads shared some examples of good practice to encourage uptake, including sharing staff stories to increase engagement with testing; using peer to peer video messaging across different staff groups to enable staff to support one another; and having strong support for staff including training workshops, a dedicated point of contact for staff to ask questions, supportive leadership, and regular communications.
Which channels are used and do people switch between channels?
Available data does not allow the evaluation to robustly explore whether participants in testing pathways use one or a range of channels. It also does not allow us to see if there may be specific pressure points or reasons why an individual may choose to 'switch' between testing channels.
However, evidence across the majority of pathways has found that the range of available testing options is confusing to people. The opening up of the universal offer has blurred the boundaries between pathways – people may use tests from the universal offer but record them as workplace results, or may use workplace testing but record as 'Other' on the online portal. It may not always be clear to someone turning up at a test centre for tests whether they are accessing the universal offer or community testing.
This blurring may put people off testing by making the process seem opaque and confusing, with expectations not being met. Partnerships in the Community Testing pathway think the universal offer has reduced footfall and created an expectation that people can pick up tests to take away without first conducting a supported test onsite. They feel the testing landscape could be simplified.
It also means that each pathway cannot be fully certain about the level of testing and recording of results within its domain as there may be crossover with other pathways. This is a limitation of the data and our understanding of the performance of testing across the piece. However, we recognise all testing potential contributes to case finding and is therefore a positive in public health terms.
What were people's experiences of navigating the system?
Detailed information on models of delivery is provided in chapter 4. This section looks at comments from individuals who participated in our research about their experiences.
There were positive comments from participants in testing pathways about the testing system and its delivery. Over 80% of those responding to the survey for school and school-based childcare staff said they had been given information about testing and how to test, and almost all who had been given this information had found it useful. Fifty percent of staff taking part in the social care workforce research said their employer had helped to overcome any barriers they had faced. The social care workforce research also found that the majority of employers who responded felt satisfied with the testing programme as a whole, and viewed it as a helpful part of wider prevention strategies.
However, there were also a range of issues in navigating the testing system reported. Highest risk individuals noted difficulty in ordering tests online, though unfortunately no further detail was supplied. Participants in the University and College pathway also noted that registering on the NHS website was too lengthy and difficult a process for international students. However, the main concerns about navigating the system that were reported across pathways were knowing what testing was available, carrying out tests, and recording test results.
Knowing what testing is available – information and communications
Though a minority of parents in the schools pathway said they did not have enough information on testing (2% of those who responded to the survey), other parents were keen to note that the system seemed useful and reassuring, but that there should be greater communication about its availability and benefits to counteract misinformation and peer pressure on children and young people not to take part. The need for clearer communication about the nature and the benefits of testing has been reported in other UK studies and is explored in Annex B, pp. 76-77.
Staff in childcare settings found information useful where available, but a small proportion of respondents indicated that they would have liked to receive guidance and information in an alternative format, including video with British Sign Language, audio format, Braille, or a language other than English. The importance of promoting equitable access to tests is further discussed in Annex B, p. 79.
For social care workers communication needs extended to the wider approach and overall guidance, where they were looking for:
- consistency between settings (social care vs NHS) and training materials (this may reflect the early implementation of testing in these settings, with change over time).
- A need for ongoing communication on accuracy and interpretation of tests and the purpose of testing as contexts change.
Several NHS board leads also noted the importance of national communications, with one noting that any lack of engagement from staff reflects that of the wider community, so testing communication need to also be targeted at that wider community and not just healthcare workers.
Carrying out tests
There was concern about the reliability and accuracy of tests results and where there is lack of trust there is greater disengagement with programmes. For example, in the schools pathway, some parents were reporting hearing that the tests are only 50% effective. This incorrect information was resulting in them deciding not to keep children off school. This speaks to the previous point made by parents around concerns that misinformation was spreading about testing. Social care staff also wanted more information on the accuracy of the tests. In part this seems to be fuelled also by concern about taking the test correctly. The Scottish Government polling also finds that there is mixed confidence in asymptomatic self-administered test results in the population. When asked the extent of their agreement with the statement 'I am confident that self-administered tests give a reliable results', 32% agree/strongly agree, 31% disagree/strongly disagree, and 32% neither agree nor disagree (4-5 May).
This issue was cited (together with discomfort) as one of the top three barriers to testing in the Community Testing pathway:
- Worry about the test itself – this includes perceptions the test is unpleasant or uncertainty around how to carry out the test
Doubts about the accuracy of LFD tests have been reported in other studies (see Annex B, p. 69), and recommendations made on how to target such concerns, promote transparency and trust, and help dispel myths (pp. 76-77).
Recording results
Recording results was brought up in several pathways as inconvenient and burdensome. Police Scotland and Scottish Fire and Rescue Service colleagues reported:
'issues with recording the result on the online portal (e.g. difficulties accessing the system with unique password provided, difficulties choosing the unique organisation number (UON) when recording, having to re-insert personal details and/or UON repeatedly after first login etc.)'
Parents and guardians reported finding the process of recording results too time consuming, in particular the requirement to input their child's/children's details every time. Indeed some parents reported finding the process so frustrating that it was suggested that parents and families might give up and/or only record a positive result. There were calls to streamline the process to make it quicker and more straightforward to record test results – for example, by making it possible to create an account per child, to save having to enter the same information every time. Alongside creating accounts/storing details, one parent queried whether the testing programme could use QR codes, so that a pupil or parent could simply scan a test kit's unique code and select 'Positive' or 'Negative'.
Though most staff in the Social Care Workforce testing research had attended training that had made them more confident with the testing process, they said they would have liked more information on using the results portal. Those who said their experience of testing was negative were more likely to cite lack of information as a problem. It also takes time out of their day to record results and this was cited as a barrier to participation by employers/providers. It is worth noting that those in this pathway who said they were less positive about their overall experience of testing were also less likely to say they were still testing as often as when they started. NHS Board leads noted that the results portal was difficult to use, leading to staff disengaging and not recording results. Boards said that it is very difficult to re-engage staff to record the results once they have disengaged.
Pathways use different systems for reporting results and some pathways require registration prior to recording results. These different systems and approaches to reporting do appear to have had an impact on usability and satisfaction with the overall testing pathway.
Annex B examines reporting issues with recording results in the wider literature. This literature raises questions about the validity of collected data and the risk of spreading the virus, especially if positive results are not uploaded (pp. 67-68).
How do people behave following a positive test result? What does this behaviour vary by and why? What do we know about specific groups?
There is very limited data on what people do after receiving positive results, but cautious comments can be made on the steps people take to record results, take a confirmatory PCR test, and self-isolate.
Following an asymptomatic LFD positive test result there are several steps an individual should follow. If positive, they should record the result, self-isolate immediately, and they should also book a confirmatory PCR test. People's behaviour at each step is key to understanding prevalence and reducing transmission.
From the available evidence, it does appear that people report positive results. There is greater agreement across pathways that this is important to do, whereas reporting negative and void results is not always seen as significant (more on behaviour after a negative result below).
In the schools pathway 1% of staff (49 respondents) and 1% of pupils (18 respondents) responding to the relevant surveys reported that they had received a positive result. Numbers responding as testing positive among children in the parent and pupil surveys were small. However, comparing surveys suggests that staff were more likely to take actions such as informing their school/setting, taking a confirmatory test, or immediately self-isolating than pupils were. Summaries of the relevant pupil and staff survey results are below:
| Reported action taken after a positive result | Secondary School Pupil Survey, percentage (and number) | Staff Survey, percentage (and number) |
|---|---|---|
| Self-isolated immediately | 44% (8 of 18) | 90% (44 of 49) |
| Booked a confirmatory PCR test | 28% (5 of 18) | 90% (44 of 49) |
| Informed school/setting | 56% (10 of 18) | 86% (42 of 49) |
| Took another LFD test | Less than 33% (fewer than 5 of 15) | 20% (10 of 49) |
| Did none of the above actions | Less than 33% (fewer than 5 of 15) | Less than 10% (fewer than 5 of 49) |
(Source: Schools Asymptomatic Testing Programme surveys)
The Scottish Government polling relating to the universal offer does not allow for good comparison between those testing negative and those testing positive as such a small sample tested positive. Only limited insight into the behaviours of the highest risk group can be gathered from available evidence as well, as only 2 respondents to the survey of nearly 2000 reported testing positive. These participants self-isolated at home and sought information and support from the Scottish Government website, the NHS website and from their Local Authority on what to do after getting a positive test.
As discussed in chapter 2, 72% of reported positive LFD results were followed up with a confirmatory PCR test. This does mean nearly 30% of reported positive LFD results were not followed up with a confirmatory PCR test.
Wider research by the Scottish Government into experiences of and compliance with self-isolation found that the majority of people report being fully compliant with self-isolation.[17] A measure of participants' compliance was gathered from whether they started isolating straight away, whether they left home for a disallowed activity during the 10 day isolation period, and how long they isolated for. Those who complied on all measures were categorised as 'fully compliant', while those who managed to comply on one or two measures, but not all three, were categorised as 'partially compliant'. Those who did not comply on any of the measures were 'non-compliant'. Seventy-four percent of index and contact cases report being fully compliant, 25% partially compliant, and 1% non-compliant.
Though most people report good compliance, there are some differences relating to 'partial compliance' and test result. (To note, when this research was carried out policy was that all contact cases must test during their self-isolation period, but should continue to isolate regardless of the result.) Those who test positive are more likely to be 'fully compliant' than those who test negative (80% versus 75%). Of those who are partially compliant, testing positive means they are less likely to isolate straight away (88% compared with 97%) and more likely to carry out a 'disallowed' activity before isolating (18% compared with 10%). They are then more likely to stay compliant for the remaining 10 days than those who test negative. This suggests that those who test positive are more likely to leave the house to do 'one last thing' before isolating fully.
How do people behave following a negative test result?
There is very limited robust evidence on what people do following a negative test result, but some cautious comments can be made on reporting results and self-isolation.
Across pathways there is a concern that people are not reporting negative tests. For example, in the universal offer pathway, of those who had used a test, nearly 40% of them did not record their results online (29-30 June). An earlier survey wave (25-26 May) showed that of those who did not record their result online, no-one claimed to have tested positive.
More generally in the polling data, participants who reported not recording their result were asked their reason for not doing so (25-26 May, n=63), and the most commonly selected reason was not knowing they had to (31%). Twenty-two percent said their result was recorded by their school or workplace, while 16% said they didn't think it was important to record the result. Fifteen percent said they forgot to do so, and 11% said they did not know how to do so. Please note, more than one answer could be selected so participants may have mentioned a mix of reasons. All of those who reported not recording their result said they had tested negative.
These reasons are common across testing pathways, with all pathways finding some evidence that negative results are being underreported. This is also reported in other UK research (see Annex B, pp. 67-68). This suggests that there may not be enough information about the need to record negative test results and why this is important. More guidance and information could be provided to those testing on handling negative (and void) results.
Wider research into self-isolation and testing finds that contacts of cases, who test negative, are more likely than those testing positive to: leave home during the self-isolation period (14% left at least once for a non-test related activity, compared with 10% testing positive); and isolate for too few days (11% isolated for under 10 days when testing negative, compared with 1% of those testing positive).[18] Though people who test negative seem more inclined to start self-isolation immediately than those testing positive, ensuring that they complete the 10 days should be a key concern.
Contact
Email: socialresearch@gov.scot
There is a problem
Thanks for your feedback