Myalgic Encephalomyelitis/Chronic Fatigue Syndrome NICE guideline: stakeholder review
An independently-produced stakeholder review of the NICE guideline on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). It makes recommendations regarding the implementation of the guideline in Scotland, and identifying and addressing priorities for service improvement in ME/CFS care.
4. Findings: Implementation of the NICE guideline
4.1 A key element of this review was to explore the views of stakeholders as to how the NICE guideline could be practically implemented in Scotland. In holding those discussions, stakeholders were asked about one of the approaches the Scottish Government was considering, which was an implementation note, and all stakeholders were asked what would shape any document that could help to put the new guideline into practice.
Guidance to support implementation in Scotland
4.2 The responses from stakeholders varied in terms of what should shape the content of any guidance and then how the guidance could be applied. There was agreement across all stakeholder types that they did not want to wait for SIGN[2] guidance to be developed. They recognised that this would take years to develop and that something actionable in the shorter term was required.
Implementation Note
4.3 The suggestion of an implementation note received some positive feedback from a few stakeholders in that it could be a very simple solution to communicating the changes introduced in the NICE guideline and that this, potentially, could be produced in a timely fashion. However, there were also queries about how it would be developed and who would be involved. The stakeholders who raised these concerns felt that GPs would traditionally look to NICE or SIGN guidelines so questioned whether it needed to be endorsed and what status it would have, "where would an implementation note sit?" (Clinician)
Scottish Good Practice Statement refresh
4.4 The majority of those familiar with the Scottish Good Practice Statement (SGPS) felt that it was still very relevant. They explained that it had been more forward-thinking than the original NICE guideline and once sections were updated in line with the new NICE guideline, e.g. information on children and young people, severe ME, refreshing the biomedical evidence that has emerged since 2010, that this was a better option than the implementation note. They felt that the SGPS contained very practical elements like specific mention of medications, tests, and investigations; all aspects that supported those who used the document.
4.5 A few people with ME/CFS went on to explain that they had found the SGPS helpful because even though their GPs were unfamiliar with it, it was a useful reference for them to know what to ask for. "I referenced it in a meeting with a GP and they had not heard of it" (Person with ME/CFS)
4.6 As well as the main guidance document, the companion documents to the SGPS, aimed at different audiences, were also considered useful. They were described as effective quick reference guides, more likely to be read by professionals and the easy read version that supported people with ME/CFS in "being their own professional".
4.7 For the stakeholders familiar with the SGPS, they felt that updating it and the companion documents was the most appropriate approach to implementing the new guideline.
Awareness-raising of any guidance
4.8 There was consensus across all stakeholders about the need to promote whatever guidance is produced. They were clear that any awareness raising of the resource was reinforced with training, investment, and leadership.
"it's not enough to put it out there and hope people take notice…it needs to be backed up by ongoing education and quick reference resources". (Clinician)
4.9 The importance of recognising the demands on clinicians' time and information overload was highlighted by all stakeholder types. They emphasised that any resource needed to be disseminated but questioned how this could be achieved without more visible commitment and leadership from within the existing systems and structures. "How do we get people to look at the good practice note? If it sits outside healthcare structures/ communications, a lot of professionals won't see it" (Clinician)
Practical tools and approaches to support the design of the guidance
4.10 When considering the practical tools or guidance that can update SGPS or inform another type of guidance note, the stakeholders suggested resources and approaches to support implementation.
4.11 For informing the design of the practical guidance note, suggestions included:
- The NICE online tool that aids understanding of the guideline;
- Drs with ME guide 'Putting it into practice - what the NICE guidelines means for ME/CFS' (Putting it into Practice: What NICE ME/CFS means for GPs - Doctors with M.E.);
- Materials from the free online learning module[3] promoted by four of the ME/CFS charities developed by Nina Muirhead and based on 10 ME/CFS patient stories Myalgic Encephalomyelitis | Chronic Fatigue Syndrome | CPD Course (studyprn.com); and
- Physios for ME information Home | Physiosforme.
4.12 To support the implementation, there were also suggestions as to what actions could be taken to roll out or reinforce whatever guidance is produced. These varied from additional tools and mechanisms to support improved knowledge of the guideline, to strategic actions to raise the profile of ME/CFS and its management. Stakeholders proposed:
- vehicles for disseminating information and raising importance - letter from Chief Medical Officer, Chief Executive Letter (CEL) about ME.CFS from Minister;
- approaches to CPD for clinicians - small group practice-based learning where GPs tackle a different topic every month, protected learning time to look at guidance and understand more about ME/CFS, delivery of ME/CFS training about diagnosis and care, peer to peer sharing of knowledge - it was felt that this was more powerful "doctors listen to doctors and likely to have more impact than hearing it from lived experience / third sector" (third sector ME/CFS organisation);
- resources to support clinicians and build confidence - revised NES module on ME/CFS; quick reference guide for clinicians, incorporate more information into existing systems, e.g. in NHS Lothian the searchable GP system RefHelp sets thresholds and gives advice on when and where to refer people to.
Services
4.13 Within the NICE guideline the need for specialist services and care and support managed by multi-disciplinary teams was identified as vital to delivering appropriate provision.
4.14 When asked to consider the current management of ME/CFS in Scotland there was a consistent response about the absence of a referral pathway, the paucity of provision, a lack of understanding from generalist services, and, if support was available, it was inconsistent and disjointed. "There isn't really an infrastructure specific to ME - no specialist teams to refer people to - more interested individuals - tends to be the luck of the draw" (Clinician).
4.15 With the exception of the ME/CFS specialist nurse in NHS Fife, who was described as having a huge caseload, long waiting lists and limited resources, stakeholders of all types struggled to identify examples of good practice. If there was awareness or recognition of some good experiences and 'pockets of interest' it was about particular GPs. The current state of provision was summarised by one clinician and echoed the views of people with ME/CFS "Individual GPs and paediatricians are doing good practice…[but] my view is that it's mainly a disaster area."
4.16 Stakeholders living with ME/CFS and third sector organisations explained that a large amount of patients are self-managing and there was anecdotal sharing of information as to which "doctors to look out for - who are the most damaging" (Person with ME/CFS).
4.17 In addition parents of children and young people faced additional challenges when accessing services. They were concerned about allegations of Fabricated or Induced Illness (FII) and the parents interviewed as part of this review described their fear that an allegation of FII could be made if they appeared too knowledgeable or challenged the opinions of professionals: "Safeguarding is a fear I have to live with" (Parent of child or young person with ME/CFS). As a result of these concerns, parents described their wariness in interacting with medical professionals and suggested that some parents are too scared to accept care because of the potential safeguarding consequences. The absence of specialist services in Scotland was perceived to increase the risk of false FII allegations.
Aids and barriers to implementation of the NICE guideline
4.18 Whilst a few clinicians expressed concerns about communicating the implementation of the guideline when there were no pathways and limited services to refer into or access, a few other stakeholders noted that this, 'blank sheet' could be used as an opportunity to build an appropriate ME/CFS service. Stakeholders identified existing services and supportive third sector organisations as elements of the existing infrastructure that could support the implementation of the NICE guideline, but all stakeholders identified several barriers that would make implementation more challenging.
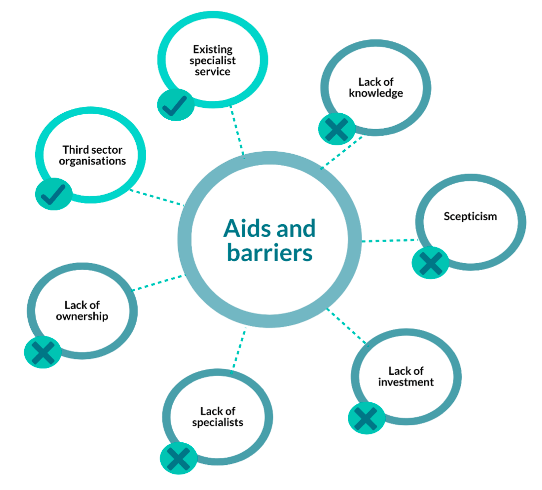
Aids to implementation
4.19 Although there are very limited ME/CFS services, some do exist, and these were considered a starting point or building block to develop more provision and support the implementation of the guideline. The service that stakeholders were most aware of, and which was referred to frequently, was the specialist ME/CFS nurse in Fife. There was an almost unanimous view that this post should be rolled out to other health boards: "an enabler but massively under-resourced - need an immediate extension and similar nurses in other areas" (Third sector ME/CFS organisation).
4.20 The work delivered by this postholder was considered a good example of how a small specialist service could be delivered. As well as NHS Fife the services in NHS Lothian at the Astley Ainslie in Edinburgh and in NHS Greater Glasgow and Clyde the Centre for Integrative Care in Glasgow were highlighted as potential starting points for expanding provision. Stakeholders from all three services felt that their existing services could be expanded to support more people with ME/CFS.
4.21 The role of third sector organisations was seen as an aid to implementation by all stakeholder types. Their potential was recognised for both the support they provided to people with ME/CFS in understanding the new guideline, and as an important bridge between clinicians and patients, "seeing more muscle from community link workers, making people aware of what's available in the third sector - a whole network who aren't active in the NHS, some have useful skills" (Clinician).
Barriers to implementation
4.22 Whilst these positive supports were acknowledged, the challenges to implementation were viewed by stakeholders as more significant. These are discussed in turn.
Lack of ownership
4.23 Stakeholders noted that the support a person with ME/CFS requires is provided by different teams within the health and social care system. However, the World Health Organisation (WHO) defines ME/CFS as a neurological condition. Nevertheless, clinicians, third sector organisations and individuals with ME/CFS expressed frustration that some neurologists shied away from leading on the condition.
"[ME/CFS] is a neurological condition as defined by WHO, meaning the logical starting point is for neurologists to get involved, they're not in the most part at the moment" (Third sector ME/CFS organisation). "They are reluctant to embrace ME as part of their canon" (Person with ME/CFS).
4.24 A few clinicians highlighted this as well, noting that, "Neurology provides support for a lot of conditions but doesn't seem to be particularly engaged with ME".
4.25 This response and absence of ownership from some neurologists was considered a stumbling block for implementation of the guideline and further development of services.
Lack of knowledge
4.26 Stakeholders identified a lack of training and knowledge about ME/CFS amongst GPs. This can lead to a delay or unwillingness to commit to diagnosing ME/CFS. Consequently an investment of time and resources would be required to increase the knowledge and understanding in such a pivotal role for providing support to help people to live with and manage their ME/CFS.
Scepticism
4.27 From individual clinicians to Royal Colleges, aspects of the NICE guideline have been questioned and this has emphasised the disbelief that some clinicians share about the condition and how it should be treated and managed. This is viewed as another barrier to implementation. One person with ME/CFS said "Royal Colleges are where most people go to continue their professional development and some don't educate on ME - some still believe in GET approach". Another emphasised the impact of the Royal Colleges' position "Royal Colleges [are] not supportive of NICE guidelines so will hamper their dissemination" (Person with ME/CFS)
Lack of specialists
4.28 Stakeholders highlighted the limited knowledge across clinicians both in primary and secondary care. This means that, unlike other conditions, there are a lack of specialists or clinicians with an interest in ME/CFS and where there is expertise it is held within a small pool of people. So, alongside the general awareness raising amongst clinicians there was a need for more people who could fill a range of specialist ME/CFS roles. A few stakeholders felt that specialists would "emerge as it becomes more acceptable to express and pursue an interest in ME and as research is better funded" (Clinician)
Lack of investment
4.29 The lack of funding and resources created an obstacle not only in the financing of the education of key clinicians but also to the investment in services that could deliver new pathways and much-needed support to people with ME/CFS. A few stakeholders also saw this as a signal that this condition is overlooked and ME/CFS is not a priority for healthcare plans or services.
Contact
Email: Clinical_Priorities@gov.scot
There is a problem
Thanks for your feedback