Mental health and wellbeing strategy
Strategy laying out our approach to improving mental health for everyone in Scotland.
8. Delivering our key priorities: what success looks like
The table below provides an overview of key priorities within each of our three areas of focus: Promote, Prevent, Provide. The table outlines which outcomes (section 4) each of our priorities contribute to and which challenges and opportunities (section 7) they seek to address.
Priority: Promote
Tackle mental health stigma and discrimination where it exists and ensure people can talk about their mental health and wellbeing and access the person-centred support they require.
Outcomes: 1,2,3,4,6Challenges and opportunities:
- Stigma and discrimination
- Delivering supports and services
- Primary and community care
- Workforce
Priority: Promote
Improve population mental health and wellbeing, building resilience and enabling people to access the right information and advice in the right place for them and in a range of formats.
Outcomes: 1,2,3,4,6,7Challenges and opportunities:
- Global challenges
- Stigma and discrimination
- Delivering supports and services
- Primary and community care
- Workforce
Priority: Promote, Prevent, Provide
Increase mental health capacity within General Practice and primary care, universal services and community-based mental health supports. Promote the whole system, whole person approach by helping partners to work together and removing barriers faced by people from marginalised groups when accessing services.
Outcomes: 1,2,3,5,6,7,8Challenges and opportunities:
- Global challenges
- Stigma and discrimination
- Delivering supports and services
- Primary and community care
- Data and evidence
- Workforce
Priority: Prevent, Provide
Expand and improve the support available to people in mental health distress and crisis and those who care for them through our national approach on Time, Space and Compassion.
Outcomes: 1,2,3,4,6,7Challenges and opportunities:
- Stigma and discrimination
- Delivering supports and services
- Primary and community care
- Workforce
- Trauma and adverse childhood experiences
Priority: Promote, Prevent
Work across Scottish and Local Government and with partners to develop a collective approach to understanding and shared responsibility for promoting good mental health and addressing the causes of mental health inequalities, supporting groups who are particularly at risk.
Outcomes: 1,2,3,4,5,6,8Challenges and opportunities:
- Global challenges
- Stigma and discrimination
- Delivering supports and services
- Primary and community care
- Workforce
- Data and evidence
Priority: Promote, Prevent, Provide
Improve mental health and wellbeing support in a wide range of settings with reduced waiting times and improved outcomes for people accessing all services, including CAMHS and psychological therapies.
Outcomes: 1,2,6,7,9Challenges and opportunities:
- Delivering supports and services
- Primary and community care
- Workforce
- Benefits of investing
Priority: Prevent, Provide
Ensure people receive the quality of care and treatment required for the time required, supporting care as close to home as possible and promoting independence and recovery.
Outcomes: 1,2,3,4,6,7,9Challenges and opportunities:
- Delivering supports and services
- Primary and community care
- Workforce
- Benefits of investing
Priority: Promote, Prevent, Provide
Continue to improve support for those in the forensic mental health system.
Outcomes: 1,2,3,6,7,9Challenges and opportunities:
- Stigma and discrimination
- Delivering supports and services
- Workforce
- Trauma and adverse childhood experiences
- Benefits of investing
Priority: Promote, Prevent, Provide
Strengthen support and care pathways for people requiring neurodevelopmental support, working in partnership with health, social care, education, the third sector and other delivery partners. This will ensure those who need it receive the right care and support at the right time in a way that works for them.
Outcomes: 1,2,3,4,5,6,7,9Challenges and opportunities:
- Stigma and discrimination
- Delivering supports and services
- Primary and community care
- Workforce
- Benefits of investing
Priority: Promote, Prevent, Provide
Reduce the risk of poor mental health and wellbeing in adult life by promoting the importance of good relationships and trauma-informed approaches from the earliest years of life, taking account where relevant adverse childhood experiences. We will ensure help is available early on when there is a risk of poor mental health, and support the physical health and wellbeing of people with mental health conditions.
Outcomes: 1,2,3,4,5,6,7Challenges and opportunities:
- Global challenges
- Stigma and discrimination
- Delivering supports and services
- Primary and community care
- Workforce
- Benefits of investing
We will set out specific actions we will take in each of these areas in our Delivery Plan. Many of the activities undertaken in one area will also contribute to or overlap with the aims of others. For example, action to tackle stigma and discrimination is a key part of promoting positive mental health and wellbeing, but it can also prevent mental health issues from escalating and help ensure people are provided with the right support.
We have included a range of case studies to show existing work that demonstrates the three areas – Promote, Prevent, Provide – in action. Although each example appears under one of the three headings, many of them crossover with the other areas.
Promote
While awareness of mental health and wellbeing has improved, there is still work to do to increase understanding around both and tackle the stigma associated with mental health issues.
Promotion of mental health and wellbeing starts with all of us as individuals, families and communities. Promotion should ensure we understand it and what we can do to look after our own mental health and wellbeing and that of others in our communities.
To tackle these inequalities, we need a collective effort from local and national government, public and private bodies and organisations, the third sector, Health Boards, and our communities. All public bodies must comply with the public sector equality duty when they carry out their functions to help inform decisions.
We will work with partners and people with lived experience to shape and influence our approach to increasing awareness and understanding surrounding mental health and wellbeing and what that means. We will also ensure clear points of access for advice, proactive access to self-care opportunities, and community supports and connections for those who experience mental illness and are at risk of self-harm or suicide.
Essential to this are the vital roles that local authorities, community planning partnerships, communities and third sector organisations (which include charities, social enterprises and voluntary groups) play in developing resilience, providing social infrastructure and supporting mental health and wellbeing nationally and in local communities.
We know that employers can play a key role in tackling mental health stigma by creating workplace cultures where open and honest discussion about mental health and wellbeing is supported and where discriminatory behaviour is challenged. We want to ensure that employers have the support they need to promote and support the conditions that enable individuals to experience good mental health at work. Supporting and promoting good mental health and wellbeing at work benefits both the individuals and employers.
This includes improved productivity and business growth, fewer days lost to sickness and absence and lower staff turnover and recruitment costs.
Case Study: Aileymill Primary School
Aileymill Primary School decided to take a school-based community approach to tackle issues of stigma and discrimination surrounding mental health.
The project was initially developed to improve staff knowledge and confidence so they could recognise mental health needs and support pupils and colleagues where appropriate. Moreover, the project aimed to introduce mental health terms and educate the pupils – with a focus on stigma and discrimination and how to challenge this in a positive and empowering way.
Attitudes towards mental health improved significantly, which had a profound impact on the ethos of the school. Pupils reported feeling more confident when talking about mental health and said they could recognise signs and symptoms of poor mental health and provide pathways to support themselves, their peers and their families.
An additional unexpected, but welcomed, impact of the school-based community approach was that pupil behaviour within the school improved significantly. Aileymill Primary School partly attribute this to adapting the school ethos and culture to be more open, warm, compassionate and non-judgemental.
Case Study: Scotrail
Nadya Kuhl, Occupational Health Manager at ScotRail, shares how they dealt with stigma through the Workplace Equality Project:
"We got involved in the project as we saw it as a brilliant opportunity to try and emphasise the fact that Scotrail as a business want to try end the stigma around mental health.
With the initial survey, I was already aware of the fact that stigma is present throughout the workforce. It showed that they want to end stigma within the workplace. If they're passionate, that gives us again the opportunity to work with them.
If members on the ground can see people from high up that are passionate about this, then they're not going to be scared about coming forward. If one of their managers comes forward and says I've got depression, anxiety or PTSD [post-traumatic stress disorder], then they'll maybe think: 'Oh, it's okay, I've got that too. He's/she's spoke out about it then I can speak out about it as well.'
We've taken steps in that we've got our managers starting on a training programme, we're working through that. We're also in the process of designing ZCards which have information about the support that ScotRail and other agencies that provide help can offer. We're looking at introducing mental health first aiders, that's another one where people who may not feel confident speaking to their managers could then speak to a mental health first aider who could point them in the right direction for support."
Case Study: Peer Support
Angela experienced mental health difficulties for a number of years and finally received a diagnosis of personality disorder. She felt she needed to know more about the diagnosis and the proposed therapy and discovered a peer support group run by a local mental health organisation.
Angela found in the peer support group a place where she can be herself and share how she is feeling with others who understand and shared some of her own experiences. When she finally gets the course of therapy, the group helped her make sense of it and figure out how to put the insight and tools learned into practice.
Through the peer support group, Angela has new friends and has joined a local walking group and gardening club. Having things to look forward to and friends who understand make Angela feel that she can live the life she wants and better manage her mental health challenges.
Case Study: The Impact of a Trauma-Informed Approach
The National Trauma Training Programme (NTTP) supports a trauma-informed workforce and services and includes funding for a network of Transforming Psychological Trauma Implementation Co-ordinators (TPTICs) based in every Health Board across Scotland who provide advice, training and implementation support.
Through the TPTIC network, a request was received by a counsellor working in mental health services for help to identify a trauma-informed dentist for a client.
The counsellor was put in touch with the Chief Dental Officer who had attended the NTTP Scottish Trauma Informed Leaders Training, and in turn, he was able to put the counsellor in touch with an appropriate local dentist. Three months later, the NTTP team received the following feedback from the counsellor:
"I just wanted to say a big thanks for putting me in contact with the Head of Dentistry. I was able to have contact with a dentist who accommodated my patient and worked great with her in regards to her trauma to get her along to an appointment and check-up of her teeth. The client gave me great feedback on how well the dentist worked with her in terms of not feeling judged about the poor condition of her teeth (she needs a full extraction done upper and lower), taking the consultation one step at a time (she called my client to introduce herself before the appointment was even set), and of working with the client step by step to get into the chair and open her mouth under the light all in the client's own time. What a fantastic team we have. I can't thank you and everyone enough that we were able to do this for my client and that she was very thankful for everyone who made it possible."
Prevent
By prevention, we mean preventing mental health issues from occurring or intensifying and tackling underlying causes and inequalities wherever possible. Early identification of mental health and wellbeing issues and provision of early advice and support will continue to be an important part of our approach. This includes providing support, care and treatment for those in distress, and improving our response to people experiencing crisis, keeping them safe and preventing their situation from escalating further.
We will continue to develop ways of working to increase access to a range of early intervention initiatives and services in primary and community settings, recognising the substantial support needed and provided within GP settings. In doing so, we aim to prevent people from becoming so unwell that they require more intense interventions and treatments that may have a negative impact on their daily lives. We will also ensure provision of a range of support for self-management approaches, including digital options, to promote good mental health and wellbeing and sustain recovery.
We will work more closely with the third sector and support communities to recognise and respond to people's needs and take a whole family approach to support. Investment in mental wellbeing will support new dedicated mental health supports and services, including raising the profile and importance of peer support relationships in helping people with mental health and wellbeing challenges, particularly throughout recovery from mental ill health.
We know that there is a higher risk of unemployment amongst those with mental health issues, and that mental health issues can be a significant factor in the cause of economic inactivity for those with long-term health conditions. As well as the significant impact this may have on individuals, it can also be costly for employers. However, research[12] shows that for every £1 spent on mental health interventions, employers can expect a return of £5 on their investment in reduced sick days and increased productivity.[13] By focusing on prevention and early intervention approaches, individuals can be supported to sustain secure employment with less cost to employers through fewer days lost to sickness and absence.
Integral to early intervention will be recognising and targeting evidenced-based approaches for particular groups and communities who are at greater risk of poor mental health. This includes people with long-term physical health conditions, ensuring they are not further stigmatised.
We will also seek to improve links between different parts of the system to ensure people are connected directly to the advice and support they need, wherever they first seek help.
Case Study: Pachedu
Pachedu, a charity working with diverse minority ethnic groups across a broad range of protected characteristics, received funding for a variety of activities based around improving their community members' mental health.
Activities range from advocacy work, cooking, gardening, focus groups exploring the development of a Mental Health Toolkit, community wellbeing map and social events for men and women. One participant from such an event shared:
"This is such an amazing experience to participate [in]. As people from the minority group, we always need opportunities to socialise and eventually be in the position to support each other through our daily hassles. Please keep the ball rolling."
Case Study: Perinatal Support
Inaya and her husband Maaz want to have a baby. Inaya has bipolar disorder and takes medicine to help stay well. They see Inaya's psychiatrist for advice, and she explains there is a risk of Inaya's illness returning after the birth of her baby. However, there are several things that can reduce the risk. She suggests they meet with the specialist perinatal mental health team for advice on medicines in pregnancy and ways of staying well. The team arrange regular contact with their psychiatrist and community nurse, and Inaya also has help from the team nursery nurse to prepare her for caring for her baby.
After birth, Inaya remains well but struggles as they have no other family close by and finances are tough. She finds it hard to relate to her baby. Her health visitor sees her regularly, and the team parent–infant therapist provides appointments with Inaya, Maaz and baby Hasan to improve their developing relationship. The team put her in touch with the Mental Health and Money Advice Service and contact Amma Birth Companions who arrange for Inaya to attend a peer support group. She makes friends with other mothers, and Hasan's development blooms through playtime and social interaction.
A year later, Inaya continues to have the support of her local mental health team, and the couple are thinking of having another baby.
Case Study: Occupational Therapy
Traditionally, occupational therapists work in acute services, community-based rehabilitation, secondary care services and social work teams, supporting people when ill health or disability has had a significant, detrimental impact on day-to-day functioning. Lisa is part of an occupational therapy team working in GP practices where they provide early intervention for patients. She said: "GP colleagues have been surprised at the range of ways that we can help their patients. By incorporating occupational therapy in primary care, we have been able to:
- Educate people with long-term conditions on how to manage work and home tasks so they have the energy to maintain a well-balanced life.
- Support people who struggle to access their local community due to anxiety or poor mobility.
- Recommend changes to a person's workplace or job role to help them remain at or return to work.
- Provide equipment to make it easier for someone to carry out self-care tasks at home.
- Connect people with health, social care and community services through signposting or referral.
Patients have been overwhelmingly positive about the difference that occupational therapy has made to their lives. They tell us:
- They feel more independent in their homes.
- They cope better with stress and anxiety.
- They are engaging with activities in their local area.
- They socialise with friends and family more often.
It is understood that when people do what is important to them, they generally feel happier, require less health and social care support, and are more likely to be at work. Evaluation of our service also suggests that it reduces referrals to secondary care and leads to reductions in spending on prescriptions, social care and welfare benefits."
Case Study: Financial Support Models
As part of their early intervention and prevention approach, North Ayrshire Council considered how acting on the social determinants of wellbeing can influence mental health. During local consultation, children, young people, families and professionals were asked, "What are the most common types of issues you believe children and young people and their families are facing?" Thirty-eight per cent of respondents cited poverty or financial hardship. Recognising that financial insecurity can be a key driver of poor mental wellbeing for children and families, North Ayrshire Council considered a number of models that offer financial support, including one where there was a full-time Welfare Rights Officer (WRO) working across seven of the nine secondary schools.
The intended outcome of the model is shown below:
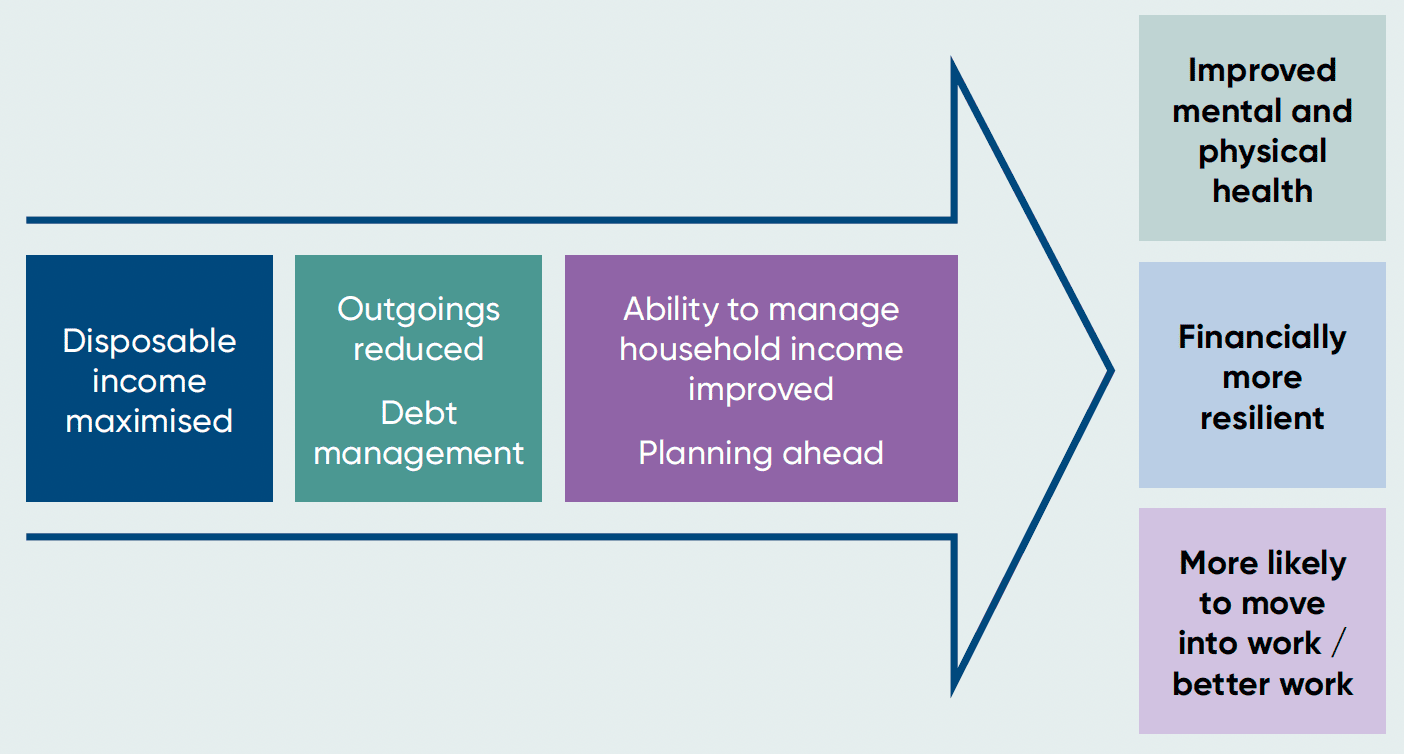
Graphic text below:
Disposable income maximised
Outgoings reduced, Debt management
Ability to manage household income improved, Planning ahead
- Improved mental and physical health
- Financially more resilient
- More likely to move into work / better work
Types of support offered to families include money/budgeting advice, debt advice, welfare rights advice, health and wellbeing advice, and signposting to employability support services.
Strong links have been established across the system to support access to the WRO. Pastoral Teams can signpost parents and carers to the WRO, and the WRO attends events for parents and carers to raise awareness of the service. Social media has been used to communicate details of the service, and the WRO has been able to develop a close partnership with education staff, delivering training on financial insecurity.
To date, this has had financial gains for families of over £500,000, and qualitative evidence indicates this has had a positive impact on family wellbeing.
Provide
People who live with mental health conditions, as well as those who experience poor mental health at points throughout their life, should benefit from timely access to safe, effective and compassionate person-centred and whole-family approach to support, care and treatment. This will mean continuing to work closely with Health Boards and local partners to ensure waiting time standards are met and that services are responsive to the experiences of those who use them.
We are committed to providing high-quality mental health and wellbeing support and care. This means people can access the right care, in the right place, at the right time. Our whole system approach sets out the different kinds of support and care people might need to access at different points in their lives. This means responding to the different needs of children, young people and adults, as well as marginalised groups.
We will continue to improve and enhance mental health supports and services, giving consideration to suitable digital and new technology services (where evidenced and appropriate) and other non-digital formats, to ensure people receive quality care and treatment as close to home as possible that meets individual needs. Scottish Government will also continue the successful partnership work with Police Scotland, the Scottish Ambulance Service, NHS 24, Health Boards and others, including the third sector to ensure those in crisis can access the best care as quickly as possible.
As with actions required under 'Promote' and 'Prevent', we know doing more of the same and providing investment in the same system will not deliver the change needed. For mental health services, setting clear outcomes and priorities for change will be necessary to drive improvement.
We will set out clear expectations for what mental health services will look like and how we will provide assurance of high-quality care. As part of this, we will continue to work with partners to improve the forensic mental health system.
Scottish Government will continue working with partners to develop Quality Standards and Specifications for mental health services, setting out clear expectations for what services will look like, recognising the need for local flexibility, whilst also providing assurance of high-quality care. These will be informed by the principles in this Strategy.
Scottish Government will work with partners to strengthen the scrutiny and assurance of the delivery of mental health services. The quality and safety of NHS mental health in-patient services are important in supporting positive outcomes. Whilst some environments are modern and enable the provision of high quality care, others need improvement. A national tool will be developed to assess and support improvement in the quality and safety of the mental health built environment.
Alongside this we will continue to develop accurate and reliable data with systems that are fit for purpose to report on progress towards improved outcomes.
Case Study: Pamis
David is an active dancer and storyteller. At a young age, he was diagnosed with multiple learning disabilities. This means he requires additional support to participate in mainstream education, as well as significant engagement and support across CAMHS services, children's services, social work and community organisations.
With support from Promoting a More Inclusive Society (PAMIS), an organisation that supports people with profound and multiple learning disabilities and their families, carers and professionals, David and his mother have been able to use the organisation's Digital Passport to set down his needs and preferences. These range from providing a background on his family, to his likes and dislikes, to his stated preferences in the event in-patient care needs to be provided. This tool is owned by David and his family and is used to communicate across the different settings and with practitioners providing support.
This passport enables David to have agency in leading on decisions around his mental health care with the support of the people around him, teaching people how to communicate with him and bringing a digital approach to a group of people who are largely excluded from technology.
Case Study: Mind To Mind
Bob, a 68-year-old from Edinburgh, has shared the mental health challenges he's experienced on the online Mind to Mind platform at NHS inform and what he has found helpful following a diagnosis of post-traumatic stress disorder.
Encouraging people to reach out and speak to someone if they need help, Bob said:
"There are plenty of professionals out there that will give you all the help you need, you just have to reach out and take the first step. But for your own and your family's sake, it's best to take that step. Don't feel you're alone, remember many others are going through the same thing.
To be honest, support group therapy was probably one of the best and most positive experiences for me. I found it tremendously helpful to be able to talk to people who shared the same sort of experiences. It makes you listen and makes it easier for you to relate to things that you think only you go through.
I would urge anyone if they can find someone or a group of people they can trust to speak to them. I learnt that most people have at some stage gone through some sort of mental health issue, whether that be to a greater or lesser degree. This is why I emphasise the idea of trying to speak to someone because you just don't know. Hearing from other people is what can help you, essentially. It's what helped help me.
I will always have PTSD [post-traumatic stress disorder], but what I have learnt is that it's how you cope and manage which is the most important thing."
Contact
There is a problem
Thanks for your feedback