Organ and tissue donation - opt-out system: five year monitoring and evaluation plan
Five year monitoring and evaluation plan of the organ and tissue donation opt-out system, as stipulated by the The Human Tissue (Authorisation) (Scotland) Act 2019.
Introduction
This document outlines a five year monitoring and evaluation plan of the organ and tissue donation opt-out system. The requirement for monitoring and evaluation was stipulated by the 'The Human Tissue (Authorisation) (Scotland) Act 2019' (hereafter referred to as 'the Act') which introduces the opt-out system. This plan outlines:
- The outcomes (short, medium and long term) that the Act is aiming to influence
- The evaluation logic model
- The data sources and indicators that will be used to monitor progress
- A proposed monitoring and evaluation timeline
This is a working document, and therefore time points and activities may be changed over the monitoring and evaluation period as necessary.
Policy Context
The Act introduced a system of 'deemed authorisation' for organ and tissue donation for transplantation, changing the current 'opt-in' system to an 'opt-out' system. This means that if someone dies in circumstances where they potentially could become a donor, and they have not recorded a donation decision, they would be presumed to be willing to donate unless their family provides information that the potential donor was unwilling to do so. The Act is predicated on the views of the donor taking primacy.
The implementation of this legislation in Scotland included a package of implementation activities, such as training targeted at NHS staff, public information aimed at raising public awareness, and stakeholder engagement. This approach is supported by research conducted in other European contexts where there has been a change to an opt-out system, which demonstrated the importance of a broader package of implementation activities to support the efficacy of the shift to an opt-out system.
Approach to Developing the Plan
The Scottish Government (Health and Social Care Analysis Division) developed a draft evaluation plan in 2018, in collaboration with NHS Health Scotland, who facilitated an evaluability assessment workshop[1]. The result was an initial logic model outlining the various implementation activities and intended outcomes of the changed legislation, a draft set of evaluation questions and proposed methods for answering each. This version of the monitoring and evaluation plan builds on this previous work and was informed by further discussions with the Act implementation team.
This plan is based on a theory-based evaluation design. Theory-based designs address the challenges of attribution and impact within complex policy and delivery landscapes. The aim of most evaluations is to determine whether a new intervention or policy has produced the intended long-term changes. However, attributing changes to any one intervention or policy is challenging, as longer term outcomes are influenced by a wide number of external and contextual factors. This makes it difficult to assess the impact of the intervention activities.
In the context of organ and tissue donation, a challenge will be to evaluate the extent to which the legislative change to an opt-out system – alongside the supporting implementation activities – have impacted on a number of the long-term potential outcomes. This is particularly the case for outcomes related to numbers of organ and tissue donations and transplants in Scotland. This is because there are a number of contingencies between gaining authorisation to proceed to donation and successful donation and/or transplantation, which are largely clinical in nature. An opt-out system cannot impact on these contingencies. As such, whilst increased donation and transplantation is the ultimate aim of the legislation, these measures do not provide a direct read-across by which to understand the success of the change to an opt-out authorisation system, or its package of implementation activities.
Outcomes and Logic Model
Outcomes
The theory-based evaluation framework for the Act identified 16 potential outcomes, listed below. These outcomes underpin the data that will be collected on the donation process for the purposes of monitoring and evaluation.
It should be noted that Outcome 11 – increased donation authorisation rate – is a priority outcome to achieve the ultimate aim of the legislation to increase donation and transplantation. The other intended outcomes of the Act work to support the fruition of this outcome, for example, by supporting a positive donation culture in the public sphere and within the NHS, as well as supporting an infrastructure which supports donation as a normalised end-of-life care choice.
The full list of outcomes of the Act are:
Short term (1-2 years)
1. Increasing public awareness of the legislation regarding:
a. implications of opt out/deemed authorisation
b. how to register to opt in/opt out for tissue and organ donation
c. the role of family in authorisation processes
2. Increasing awareness of donation and the (implications of) legislation change among groups that are currently under-represented among organ and tissue donors, in particular ethnic minority groups.
3. Increasing proportion of people who report having a conversation with their family members about their decisions in regards to tissue and organ donation.
4. Increasing awareness of, knowledge about, and support for the legislation among NHS staff involved in organ and tissue donation, to support timely referral to specialist organ donation nurses or tissue donor coordinators.
5. Infrastructure in place for early identification and referral of potential donors.
Medium term (3-4 years)
6. Increasing public trust in the NHS organ and tissue donation system.
7. Increased number of people that feel they are able to make an informed decision about organ and tissue donation.
8. Increased registrations of a decision about organ and tissue donation on the Organ Donor Register.
9. Increased proportion of families supporting donor's decisions.
10. Increased trust and skills in the NHS donation system within the NHS professional culture.
11. Increased donation authorisation rate[2].
12. Reductions in missed donation opportunities.
Long term (5 years)
13. Permanent culture change within the public and NHS professional culture, to include shifts such as: normalisation of donation as part of end of life care, and increased cultural willingness to discuss donation decisions.
14. Increased percentage of people becoming donors from the potential donors group (in Scotland).[3]
15. Increased percentage of transplants (from donors in Scotland).
16. Support available for relatives of persons who have authorised, or who have been deemed to have authorised organ and/or tissue donation (both before and after organ/tissue retrieval takes place).[4]
Notes:
- Outcomes 14 and 15: Whilst increased donation and transplantation is the ultimate aim of the legislation, there are a number of factors (often clinical) which mean that authorisation does not always lead to successful donation or transplantation. The move to an opt out system does not change these contingencies.
- Outcome 16: Availability of support for donor's relatives is not a specific aim of the Act. However support for donor families is an important part of the donation process and so this outcome is included as part of the evaluation requirements, but is one which is not dependent on the other outcomes for fruition. This outcome is already supported by current, NHS Blood and Transplant (NHSBT) and Scottish National Blood Transfusion Service (SNBTS) practice.
Outcome strands
The outcomes fall within three main strands:
| Strand | Refers to | Outcomes |
|---|---|---|
| A. Public Attitudes | Public's views on, attitudes toward and behaviours associated with donation | 1-3, 6-9, 13-15 |
| B. Workforce | Views, confidence, and practice of NHS Scotland staff members involved in donation processes | 4, 5, 10, 12, 13 -15 |
| C. Monitoring Data | Data currently collected by NHSBT and SNBTS on referral, authorisation, donation and transplantation rates | 11, 12, 14-16 |
Logic Model
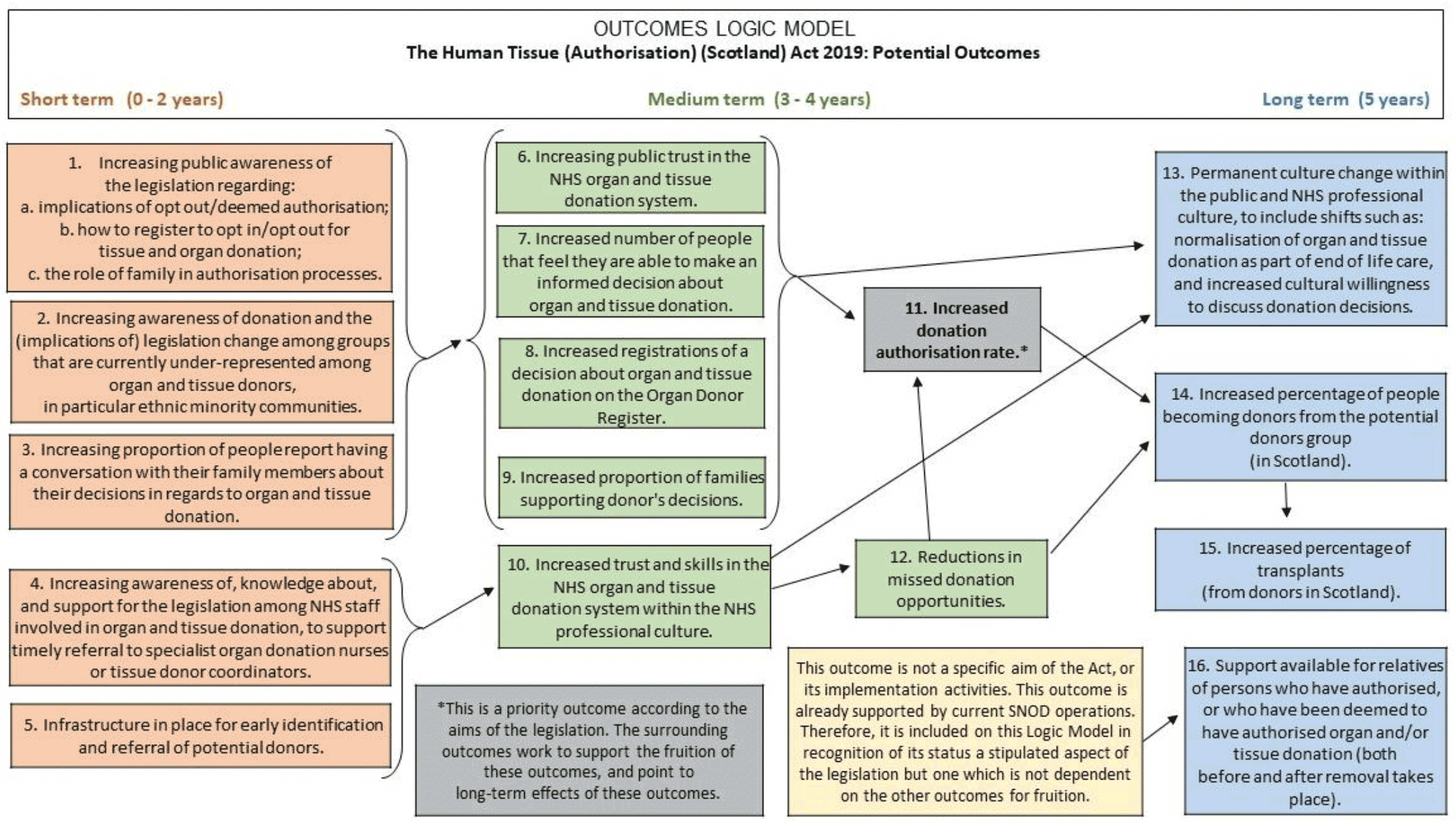
The logic model below (Figure A) illustrates the relationships and dependencies between the outcomes. It demonstrates which outcomes are projected to impact on the achievement of other outcomes. In addition, the logic model illustrates the anticipated timeframes within which impacts may be seen as a result of the implementation of the Act and its package of implementation activities.
For example, the success of increasing authorisation rates (Outcome 11), a priority outcome of the Act that is linked to donation and transplantation rates, is projected to be a measureable trend toward the end of the five year monitoring and evaluation period. An increase in authorisation rates is likely to be supported by the success of Outcomes 6-9 and 12, measurable at the midway point of the period. In turn, these are largely impacted by Outcomes 1-3, which are likely to show first signs of impact from the implementation of the Act and its package of supporting activities. Furthermore, authorisation rates (Outcome 11) are positioned to impact on Outcome 14, and in turn Outcome 15.
Three further logic models are included in Annex 1 to illustrate which outcomes fall within each of the three strands (Public Attitudes; Workforce; and Monitoring Data).
Contact
Email: socialresearch@gov.scot
There is a problem
Thanks for your feedback