Benzodiazepine use - current trends: evidence review
This paper presents an overview of current knowledge of trends around benzodiazepine-related deaths, hospital admissions, police seizures and prescribing practices in Scotland.
2. Key trends
2.1 Motivations for use
There is a general lack of evidence relating to the reasons for increased prevalence of benzodiazepines in Scotland, although a number of recent studies indicate a complex range of factors. These include changes in prescribing practices (specifically a significant decrease in benzodiazepine prescribing throughout the 2000s); widespread availability due to illicit overseas imports; and vastly increased domestic production of illicit benzodiazepine tablets. There are similarly a range of other issues associated with drug dependency and problematic drug use in Scotland, such as high rates of deprivation, high social inequality and historical social policy.[4]
Motivations for use have been varyingly explored in literature, broadly encompassing a range of psychological, social, economic and supply-driven factors. For example, benzodiazepines are often used to self-manage psychiatric disorders, anxiety, insomnia, substance withdrawal symptoms, and as a means of coping with traumatic experiences, grief and loss, boredom, and isolation. They are also used for their pleasurable effects and their ability to both alter perceptions of time and enhance the effects of opioids and other substances. Their affordability and ease of access likewise comprise motivations for use.[5] [6]
A recent long-term ethnography of polydrug use in Scotland Roe, 2020 explored in part the experiences of people who use benzodiazepines, including motivations for use and contextual factors underpinning substance dependency.[7] Participants in the research, most of whom considered heroin as the main drug on which they were dependent, often used benzodiazepines on an everyday basis, frequently in combination with other substances.[8] Roe states that, at times, benzodiazepines were purposefully combined and taken with other drugs, and at others different drugs were taken opportunistically over the course of the day. Several participants noted the ability of benzodiazepines to ease feelings of stress, anxiety and loneliness, and to distance painful or traumatic memories, effects that were strengthened when used in combination with heroin, alcohol and other substances. Participants also described a distinct bodily pleasure and even at times sense of 'fulfilment' afforded by benzodiazepines, alongside their ability to provide moments of relaxed calm amidst often strenuous and volatile circumstances.
Roe also notes that benzodiazepines, particularly when combined with other substances, often produced particular effects on the passage of time, such as slowing or halting time, or removing one from time altogether. Altering time perception constituted a particular motivation for use, as intoxication acted to counter time was that felt as overwhelming fast-paced or chaotic, or else time that was experienced as empty, dragging or overly repetitive. For instance, the author quotes a female participant describing the effects of Valium on time, who stated, "Downers like Vallies just slow everything right down, in a nice way though. Relax you. [. . . ] Things just fall away, ken, nothing matters."[9]
The physiological effects of combining benzodiazepines with heroin, alcohol and/or cocaine were pleasurable, but could equally be severe and unintentional, such as "physical and emotional distress; extreme nausea; hallucinations; extreme memory and time loss/fragmentation" as well as non-fatal and fatal overdose.[10] Research participants equally spoke of effects of benzodiazepines lessening over time and the need to continually increase doses. There were a limited number of instances in which participants, who were not involved in treatment services remarked that they had purchased diazepam and methadone in order to detox themselves from heroin and alcohol.
Other works have explored the exceptional availability and affordability as significant motivations for benzodiazepine use.[11] McAuley and colleagues note that benzodiazepine prescriptions increased throughout the 1990s until the mid-2000s, at which point there was a shift in clinical guidance in response to escalating drug-related deaths. The diversion of benzodiazepine prescriptions to the illicit market increased its use among populations who used drugs, with decreases in prescribing coinciding with the emergence of novel psychoactive substances (NPS), including new benzodiazepines.[12] Vast quantities of new benzodiazepines, such as phenazepam, began to be imported into the UK. A shift has occurred, however, in recent years towards the domestic production of benzodiazepines, particularly etizolam, in Scotland, with "domestic industrial laboratories capable of producing millions of pills per day," at extremely low cost to consumers.[13]
Qualitative and ethnographic studies have likewise noted high frequency of benzodiazepine use among substance-using populations, and that benzodiazepines are commonly used in combination with other drugs, using a variety of consumption methods; including oral, snorting, intramuscular and intravenous.[14]
2.2 Role of benzodiazepines in drug-related deaths (DRDs) in Scotland
There were 1,339 drug-related deaths in Scotland in 2020, the highest number ever recorded and a continuation of upward trends since 2014. Benzodiazepines were implicated in 974 deaths (73% of all drug-related deaths), continuing the steep rise in benzodiazepine deaths since 2016.[15] Between 2008 and 2015, for instance, benzodiazepines were implicated in fewer than 200 deaths per year, before rising to 426 in 2016; 552 in 2017; 792 in 2018 and 902 in 2019 (Figure 1).
The increase of benzodiazepine-related/implicated deaths over the past five years appears largely attributable to street benzodiazepines.[16] For instance, deaths where street benzodiazepines were implicated have risen from 58 in 2015 (8.2% of total DRDs) to 879 in 2020 (66% of total DRDs). These were largely related to etizolam, a substance which only emerged on the market in the mid-2010s and has risen sharply in its implication in deaths to 806 in 2020 (Figure 1).[17]
Deaths for which 'prescribable' benzodiazepines were implicated have remained relatively stable, with the figure for 2020 (210 deaths) being lower than in 2017 and 2018 (234 and 238 respectively). Diazepam was formerly the most commonly implicated in benzodiazepine-related deaths until the mid-2010s when illicit street benzodiazepine-implicated deaths sharply increased.
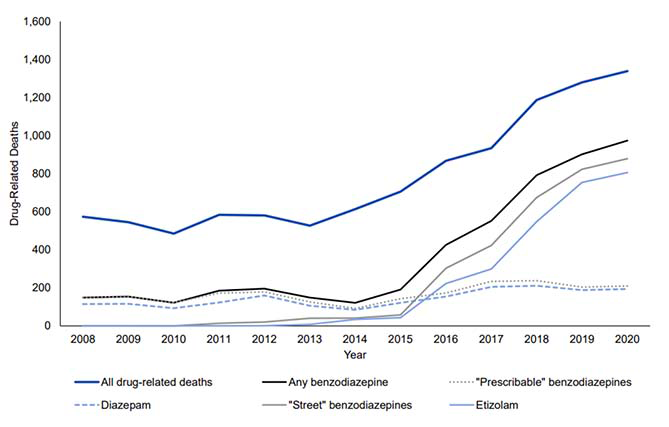
Source: NRS 2021
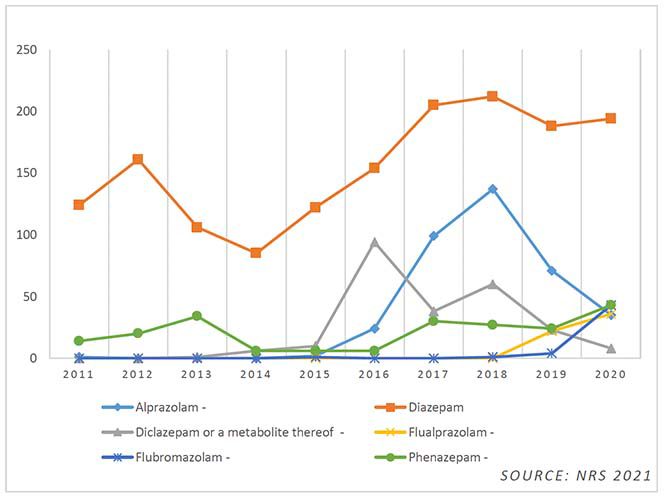
While etizolam remained the most prevalent street benzodiazepine in 2020, more detailed toxicology data within the NRS drug-related deaths report also evidence broadly increasing prevalence of different variations, such as alprazolam (Xanax), diclazepam, flualprazolam, flubromazolam and phenazepam (Figure 2). As of 28 February 2021, the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) was monitoring 30 new benzodiazepines through the EU Early Warning System.[18] Of these, more than 80% were detected for the first time between 2014 and 2020. Etizolam and many other street benzodiazepines, such as flualprazolam and diclazepam, were not controlled substances in the UK until the Psychoactive Substances Act of May 2016, before being included under the Misuse of Drugs Act in May 2017.
As unregulated imitations of prescription drugs, street benzodiazepines are often widely variable in potency, much more potent than their prescribed counterparts, and may contain a number of unmarked harmful substances. For example, etizolam is roughly 6-10 times more potent than diazepam. Etizolam is, however, a licensed prescription medication in Italy, India and Japan, and shows relatively comparable signs of harm to diazepam when used therapeutically.[19] The harms of street benzodiazepines largely stem from their illicit manufacture and to their often being disguised and sold as genuine medications, with exceptionally high availability and affordability leading to consumption of huge quantities.[20] The use of higher doses – often supratherapeutic or 'megadoses' – greatly increase the risk of overdose, dangerous drug interactions and adverse effects. Additionally, both their generally shorter half-lives and common side-effect of memory loss likely lead to more frequent dosing.[21]
*These data are reported on the bases of the Office for National Statistics (ONS) 'wide' definition of Drug poisoning deaths rather than the NRS drug-related death definition.
**Etizolam, by far the most common benzodiazepine, has been excluded from this chart for scale.
As Figure 2 demonstrates, a distinct shift is apparent in 2016 with a severe rise in drug-related deaths attributable to street benzodiazepines.[22] Implicated deaths for alprazolam and phenazepam have continued to fluctuate, while flualprazolam and flubromazolam have emerged to show potential indications of following the trajectories of etizolam, although there is currently insufficient data to predict trends.
Drug-related death data also highlight that benzodiazepines are likely to be used in combination with other drugs. In 2020, 98.7% of benzodiazepine-implicated deaths had more than one drug present, with a total of 13 deaths in which only one benzodiazepine was implicated. Eight of these deaths were implicated solely by etizolam, meaning only 1% of etizolam-related deaths involved etizolam alone. Opioids were implicated in 94% of benzodiazepine-implicated deaths, with heroin/morphine being implicated in 49% of all benzodiazepine-implicated deaths (Figure 3).[23] This trend is widely mirrored in all DRDs, of which 184 (14%) involved only one drug.
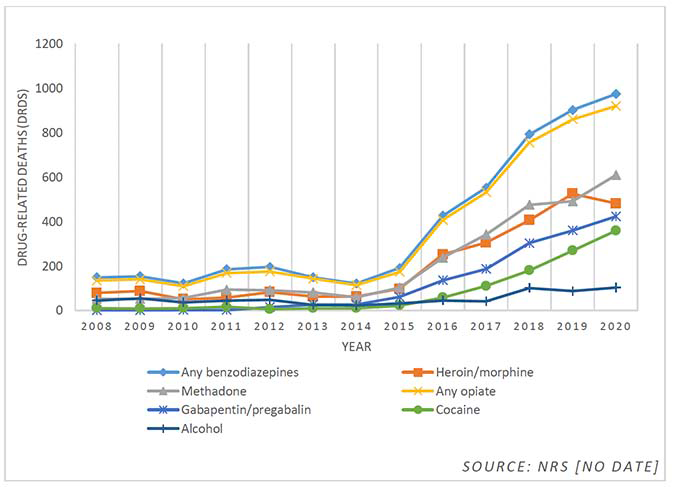
Figure 3 demonstrates that in 2020 the most common combinations of substances in benzodiazepine-implicated deaths were:
- Any opiates/opioids: implicated in 94% (920) of benzodiazepine-implicated deaths.
- Methadone: implicated in 63% (609) of benzodiazepine-implicated deaths.
- Heroin/morphine: implicated in 49% (481) of benzodiazepine-implicated deaths.
- Gabapentin/pregabalin: implicated in 43% (423) of benzodiazepine-implicated deaths.
- Cocaine: implicated in 37% (359) of benzodiazepine-implicated deaths.
- Alcohol: implicated in 11% (103) of benzodiazepine-implicated deaths.
2.2.1 Benzodiazepine-implicated deaths by age, gender, deprivation profile and NHS board
Overarching trends in all drug-related deaths in 2020 suggest an ageing cohort of users and higher overall deaths among men, although with a sharper increase in DRDs among women.[24] DRDs across all substances are strongly associated with poverty and deprivation, with people in the most deprived quintiles[25] being 18 times more likely to have a drug-related death than those in the least deprived quintiles. These trends are largely consistent with benzodiazepine-related deaths. In 2020, as with all DRDs, the rates of benzodiazepine-implicated deaths were highest for those in the 35-44 year age bracket, closely followed by those aged 45-54 years.
Men accounted for 717 (74%) of benzodiazepine-implicated deaths in 2020, relatively consistent with recent years, while 257 (26%) benzodiazepine-implicated deaths were in women. These figures are also closely mirrored in deaths implicated by street benzodiazepines, and etizolam specific deaths, when broken down by sex.
Most NHS boards had similar percentages of benzodiazepine-implicated deaths to that of the overall figure for Scotland, in the range of 72-79%. The lowest rates belonged to Grampian with only 57% of DRDs implicating benzodiazepines, while the highest rates were in Forth Valley (81%).
There were notable differences between areas in which prescribable benzodiazepines and street benzodiazepines were implicated in deaths. Compared against the overall figure for Scotland of 16% (of all DRDs having prescribable benzodiazepines implicated), the highest rates of deaths implicated by prescribable benzodiazepines were Lothian (42%, or 66 out of 159); Grampian (40%, or 40 out of 99) and Fife (26%, or 17 out of 65), while the lowest rates belonged to Greater Glasgow & Clyde (2%, or 11 out of 444), Ayrshire & Arran (3%, or 3 out of 106), and Lanarkshire (4%, or 7 out of 185).[26]
The highest percentage of deaths implicated by street benzodiazepines were in Tayside (76%, or 80 out of 105) and Forth Valley (74%, or 57 out of 77), while the lowest were in Grampian (33%, 33 out of 99) and Lothian (52%, or 83 out of 159). Table 1 presents data for deaths in which benzodiazepines were implicated by NHS Board. [27]
Table 1. Drug-related deaths by selected drugs reported in 2020 and NHS Board area.
| NHS Board | All drug-related deaths | Percentage implicated by any benzodiazepine | Percentage implicated by any prescribable benzodiazepine | Percentage implicated by any street benzodiazepine |
|---|---|---|---|---|
| Scotland | 1,339 | 73 | 16 | 66 |
| Ayrshire & Arran | 106 | 73 | 3 | 71 |
| Borders | 18 | 72 | 11 | 67 |
| Dumfries & Galloway | 22 | 73 | 5 | 73 |
| Fife | 65 | 78 | 26 | 71 |
| Forth Valley | 77 | 81 | 21 | 74 |
| Grampian | 99 | 57 | 40 | 33 |
| Greater Glasgow & Clyde | 444 | 73 | 2 | 72 |
| Highland | 49 | 78 | 53 | 51 |
| Lanarkshire | 185 | 72 | 4 | 70 |
| Lothian | 159 | 72 | 42 | 52 |
| Orkney | 3 | 67 | 33 | 33 |
| Shetland | 4 | 25 | 0 | 25 |
| Tayside | 105 | 79 | 19 | 76 |
| Western Isles | 0 | 0 | 0 | 0 |
Source: NRS 2021
2.2.2 Scotland's benzodiazepine-related deaths in comparison with England and Wales and wider Europe
Benzodiazepine-related deaths in Scotland are substantially higher than in England & Wales, although rates have been increasing in both areas. Figure 4 displays the absolute numbers of benzodiazepine poisoning deaths in Scotland and England & Wales between 2009 and 2020.[28] Given Scotland's smaller population, the rates of benzodiazepine poisoning deaths are markedly higher.
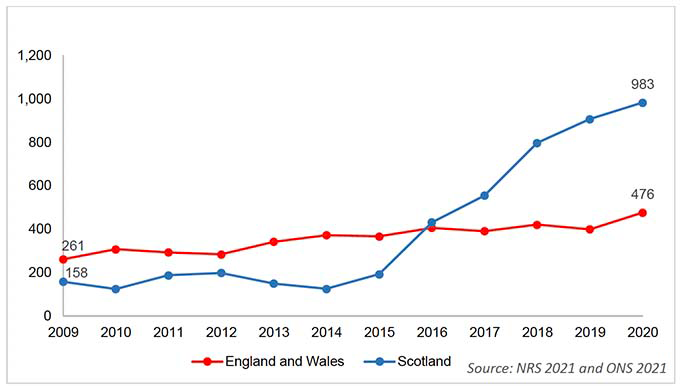
The EMCDDA notes that benzodiazepines are related to an increasing proportion of drug-related deaths in several countries, and highlights Scotland as a primary country of concern.[29] [30] The EMCDDA also note growing concerns across Europe around increasing availability of benzodiazepines through prescription diversion or the proliferation of unlicensed benzodiazepines on the illicit market.[31]
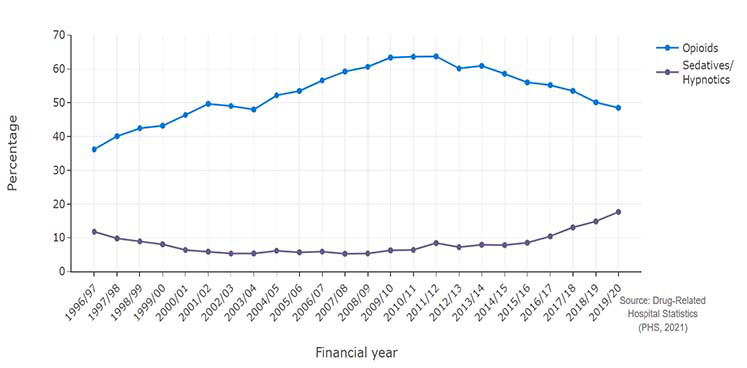
2.3 Benzodiazepine-related hospital stays
The overall number of drug-related hospital stays decreased in 2020/21 (from 284 stays per 100,000 population in 2019/20 to 270 per 100,000 in 2020/21), likely as a result of the COVID-19 pandemic. However sedative/hypnotic-related hospital stays (including benzodiazepines) increased to their highest rate on record.[32]
Out of 14,310 stays in 2020/21, the highest stay rate was associated with opioids at 127 per 100,000, which constituted a decrease from 140 per 100,000 in 2019/20. Sedative/hypnotic-related hospital stays (including benzodiazepines), increased from 50 stays per 100,000 in 2019/20 to 54 stays per 100,000 (2,643 stays) in 2020/21, the highest recorded rate since 1996/97, reflecting the continuation of a stark upward trend since the mid-2010s. For further comparison, the percentage of stays related to opioids dropped from 50.11% to 48.5% between 2018/19 and 2019/20, while sedative/hypnotic stays increased from 14.84% to 17.65%.
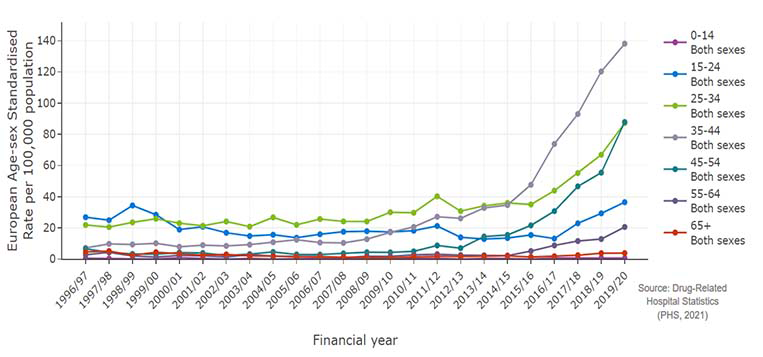
2.3.1 Benzodiazepine-related hospital stays by age, gender, deprivation profile and NHS board
General drug-related hospital stay data for 2019/20 reflect similar trends to drug-related deaths, evidencing highest rates among those aged 35-44. Stay rates specific to sedatives/hypnotics (including benzodiazepines) show an increase across all age groups, with the highest rates belonging to the 35-44 age bracket, closely followed by the 45-54 age bracket (Figure 6). Those aged 45-54 years evidenced the sharpest rise in rates between 2018/19 and 2019/20, with rates increasing from 55.54 per 100,000 population to 87.88 per 100,000.
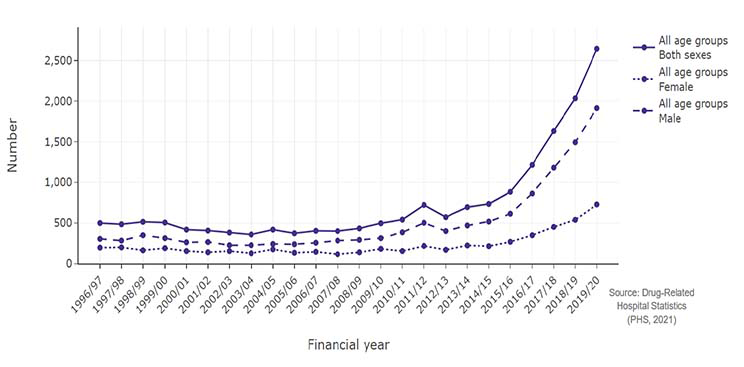
Men accounted for 72.5% of patients (1,914) who had a sedative/hypnotic-related hospital stay in 2020/21, and women for 27.5% (729), figures broadly consistent with rates for all substances. Between 2010/11 and 2018/19, the rate of sedative/hypnotic-related stays for men was consistently more than double that of women, before beginning to increase more sharply. The rate of stays is now 2.5 times higher for men than women (Figure 7).
57.8% of patients whose stays were related to sedatives/hypnotics in 2020/21 were from the most deprived quintile, consistent with rates across the time series. In 2020/21, these patients were 25 times as likely to be from the most deprived quintile as from the least deprived, compared with 16 times as likely when considering rates for all substances.
Broken down, by NHS Board, the area with the highest rates of hospital stays for sedatives/hypnotics were Greater Glasgow and Clyde, which accounted for 41% of all stays across Scotland relating to sedatives/hypnotics, or 93.49 per 100,000 population. This was followed by Ayrshire and Arran (61.45 per 100,000); Fife (55.59 per 100,000) and Forth Valley (53.91 per 100,000), while the lowest rates per 100,000 population belonged to the Western Isles (0 per 100,000), Grampian (11.97 per 100,000); and Shetland (17.78 per 100,000).
2.4 Benzodiazepine supply and seizure data
Between April 2019 and March 2020, approximately 5.3 million benzodiazepine tablets were seized in total by Police Scotland for both supply-related crimes and possession-related crimes, compared with 2.1 million tablets seized in 2018/19.[33] For comparison, in England & Wales, 1.1 million doses of benzodiazepines were seized by police forces and Border Force between April 2019 and March 2020, presenting a stark contrast to figures for Scotland.[34] [35] It should be noted that seizures are not an accurate indicator of supply, and that figures are prone to substantial fluctuation year on year, as single instances of drug seizures can dramatically affect annual statistics. Seizure quantities in Scotland are, however, consistently higher than England & Wales, especially when taking population size into account.
Etizolam accounted for an estimated 94% of benzodiazepine seizures in Scotland in 2019/20, and was also the second most commonly seized drug, following herbal cannabis. It is not possible to provide a breakdown of the number of seizures that occurred in Scotland in 2019/20, although Police Scotland have previously stated that seizures are often connected to large scale, industrial pill presses.[36] The EMCDDA have similarly noted that the demand for tablets in Scotland has resulted in, "several large-scale producers setting up illicit production sites in the west of Scotland" and that the "detection of these production sites illustrates that professional equipment (such as multi-station rotary pill presses) [are] being used by illicit manufacturers to enable quick and efficient large-scale production.[37]
For supply-related crimes in 2019/20, benzodiazepines comprised the main Class C drugs seized by Police Scotland, totalling 4.9 million benzodiazepine tablets (the vast majority of which were etizolam, although it is not possible to present separate figures for etizolam, diazepam and other benzodiazepines).[38]
From a sample of drug possession crime, it was estimated that 14% of drug possession crimes in 2019/20 involved etizolam, compared with 48% involving herbal cannabis, 9% involving cocaine and 8% involving heroin. This again reflects an upward trend since the mid-2010s; for example there were no etizolam-related possession crimes recorded up to and including 2016/17. There were a total of 4,300 possession crimes relating to etizolam in 2019/20. Contrastingly, diazepam accounted for only a very small proportion of seizures for drug possession crimes, not reaching the level required to be reported in 2018/19 and 2019/20.
It is not possible to provide a breakdown of the characteristics of offenders by specific substances, however 85% of overall offenders were male, with a median age of 29.
2.5 Prescribing practices
2.5.1 Prescribing trends for the adult population in Scotland
Data from PHS reveal that in 2019/20, 5% of the adult population in Scotland (225,000 in total) received a benzodiazepine prescription in the last year, compared with, for example, 21.6% of the population receiving antidepressants; 17.8% receiving opioid pain medications; and 3.2% receiving z-drugs.[39] In 83.8% of cases for new patients – those who had not had a prescription prior to 2015 – benzodiazepines were not prescribed for less than three months.
There has been a broad decrease in benzodiazepine prescription trends over the past ten years, with 265,000 adults receiving at least one prescription for benzodiazepines in 2010/11 compared with 240,000 in 2014/15 and 225,000 in 2019/20. Prescription rates for z-drugs have conversely broadly increased in the past ten years, from 120,000 people in 2010/11 to 145,000 people in 2019/20. However, this is a drop from 2018/19 in which 150,000 people were prescribed z-drugs.[40]
2.5.2 Prescribing trends for the adult population in Scotland by age, gender and deprivation profile.
Data available for the general adult population in Scotland demonstrate a pattern of increasing benzodiazepine use up until age 49 on average, followed by a period of slight decline and then increasing use in older age.[41]
Women are currently 1.8 times more likely to receive a prescription for benzodiazepines than men. 6.3% of the adult female population in Scotland in 2019/20 received a benzodiazepine prescription, compared with 3.6% of the adult male population. However, in 2019/20, men were up to 1.2 times more likely to receive long term prescriptions (12 months or more) than women were.
Deprivation has a consistent effect across all classes of prescription, with higher proportions of those in the most deprived quintiles receiving at least one prescription throughout the year. Although not as high as other drug classes, those from the most deprived areas are more than twice as likely to receive benzodiazepines than those in the least. Deprivation is also associated with longer treatment duration, with those from the most deprived areas being between 1.3 times as likely to receive benzodiazepine prescriptions for 12 continuous months or more, than those in the least. Trends for benzodiazepine prescribing according to deprivation quintile have been stable for the past ten years.[42]
2.5.3 Prescribing trends for specialist drug treatment
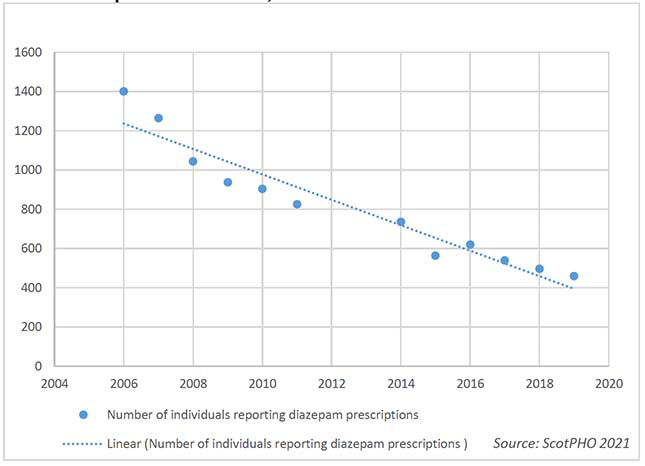
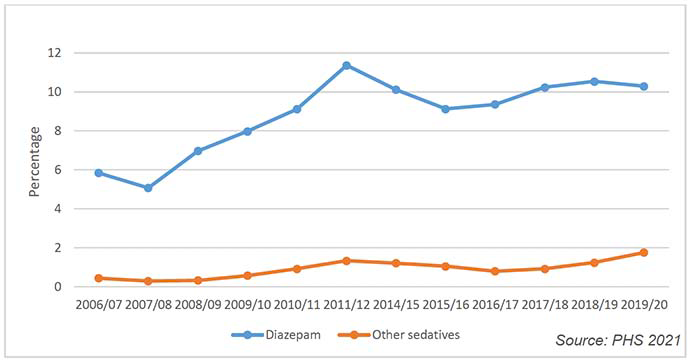
The Scottish Drug Misuse Database (SDMD) shows that up until 2011/12, diazepam was the most commonly prescribed non-Opioid Substitution Therapy (OST) drug in specialist drug treatment.[43] [44] Diazepam prescriptions for specialist drug treatment have markedly decreased since 2006/07 (before which data is not available) (Figure 8).
For instance, in 2006/07, 27% of people who reported receiving prescriptions for the treatment of addiction reported a prescription for diazepam. In 2019/20, 9% reported a prescription for diazepam, following a consistent decrease across the time series.
Though now dated, the 2018 report on the National Drug-related deaths database (NDRDD) evidences similar trends.[45] 15% of people who had a DRD in 2016 were prescribed diazepam in the 90 days prior to death compared with 24% in 2013, following a decreasing trend since 2009.
Recent diazepam prescribing decreased over the time series (2009-2016) among individuals prescribed OST, while there was no clear trend among the non-OST group. Between 2009 and 2016, those prescribed OST were more likely to be prescribed diazepam (23%) than those who were not (15%).
2.5.4 Drug use prior to treatment
Data available for those assessed for specialist drug treatment in 2019/20 show patterns of illicit drug use in the month prior to treatment.[46] Out of 10,900 people recorded on SDMD, 8,573 (79%) used illicit drugs in the month before entering treatment, with 2,495 (29%) using diazepam. Other benzodiazepines used prior to treatment are not recorded. For comparison 3,561 (42%) reported using heroin; 3,060 (36%) using cocaine/crack cocaine, and 2,486 (29%) using cannabis.
In 2019/20, 882 people out of 8,573 individuals assessed for a new specialist drug treatment episode (or 10%) recorded diazepam as the main drug for which they were seeking treatment, with the most common drug being heroin (3,109 people or 36%), followed by cocaine/crack cocaine (1,760 or 21%) and cannabis (1,544 or 18%). Reporting of diazepam as the main drug increased from 6% in 2006/07 to 11% in 2011/12, and has since remained in the range of 9% to 11% (Figure 9).[47]
Contact
Email: socialresearch@gov.scot
There is a problem
Thanks for your feedback