Organ and tissue donation: baseline report 2021
Data about organ and tissue donation in Scotland prior to implementation of ‘The Human Tissue (Authorisation) (Scotland) Act 2019’, organised into three main categories: public attitudes, workforce, monitoring data.
Introduction
This baseline report presents data about various aspects of organ and tissue donation in Scotland prior to implementation of 'The Human Tissue (Authorisation) (Scotland) Act 2019' (hereafter referred to as 'the Act'). The Act, which came into effect on 26 March 2021 introduced a system of 'deemed authorisation' for organ and tissue donation for transplantation, changing the previous 'opt-in' system to an 'opt-out' system. To ensure a successful implementation of the Act, a package of supporting activities are also in place.
The Act stipulates that a review must be carried out at the end of a five year period, setting out objectives and assessing the extent to which these have been achieved. A Monitoring and Evaluation Plan has been developed, stating the intended outcomes of the legislation and its package of implementation activities, and how these will be assessed over the five year period. This baseline report is the first component of the Monitoring and Evaluation plan for the Act.
Summary of the Act
The Act introduces a system of 'deemed authorisation' for organ and tissue donation for transplantation. This means that if someone dies in circumstances where they potentially could become a donor, and they have not recorded a decision on donation, they would be presumed to be willing to donate unless their family provide information that the potential donor was unwilling to do so. The Act is predicated on the views of the donor taking primacy. The implementation of this legislation in Scotland included a package of implementation activities, such as training targeted at NHS staff, public information aimed at raising public awareness, and stakeholder engagement. This approach is supported by research conducted in other European contexts where there has been a change to an opt-out authorisation system, which demonstrated the importance of a broader package of implementation activities to support the efficacy of the shift to an opt-out system (Evanisko et al. 1998; Garcia et al. 2008; Muthny et al. 2006; Pelleriaux et al., 2008; Simpkin et al 2009; Symvoulakis 2014).
Impact of COVID-19 Pandemic on Data Landscape
The Act was originally planned for implementation in Autumn 2020, however due to the wide-spread impact of the COVID-19 pandemic on NHS services in 2020, implementation was postponed to March 2021. The pandemic appears to have had impacts on organ and tissue donation and transplantation activity in the UK. The NHSBT Annual Organ Donation and Transplantation Activity Report 2020/2021 reported significant drops in donation and transplantation rates at various points in 2020, which were not consistent with activity trends prior to March 2020.
For this reason, the majority of data in this report covers the period prior to the onset of the COVID-19 pandemic, namely up until 29 February 2020. Although this does create a missing year of data (March 2020 - March 2021), given the significant contextual changes created by the pandemic, exclusion of this data will provide a more accurate baseline view.
It should be noted that some information within this report does cover periods of time during the COVID-19 pandemic. This is because ongoing activities promoting public awareness and NHS staff understanding of the law change continued during the pandemic period. For example, the report includes findings from surveys conducted after March 2020 as part of a marketing campaign to raise public awareness of the donation law change, as well as findings from questionnaires from Autumn 2020 completed by NHS staff who undertook training sessions related to the implementation of the Act. It is important to understand the potential impacts of these activities on current public attitudes toward organ and tissue donation, and well as NHS staff confidence levels in the lead-up to implementation of the law.
Outcomes and Logic Model
The Monitoring and Evaluation Plan is based on a theory-based evaluation design. Theory-based designs address the challenges of attribution and impact within complex and changing policy and delivery landscapes. The aim of most evaluations is to determine whether the implementation of a new intervention or policy has produced long-term changes in the target outcomes as intended. Attributing changes to any one intervention or policy is challenging however, as longer term outcomes are influenced by a wide number of external and contextual factors. In the context of organ and tissue donation, the main challenge is evaluating the extent to which the legislative change to an opt-out system – alongside the supporting implementation activities – has impacted on the number of organ and tissue donations and transplants in Scotland.
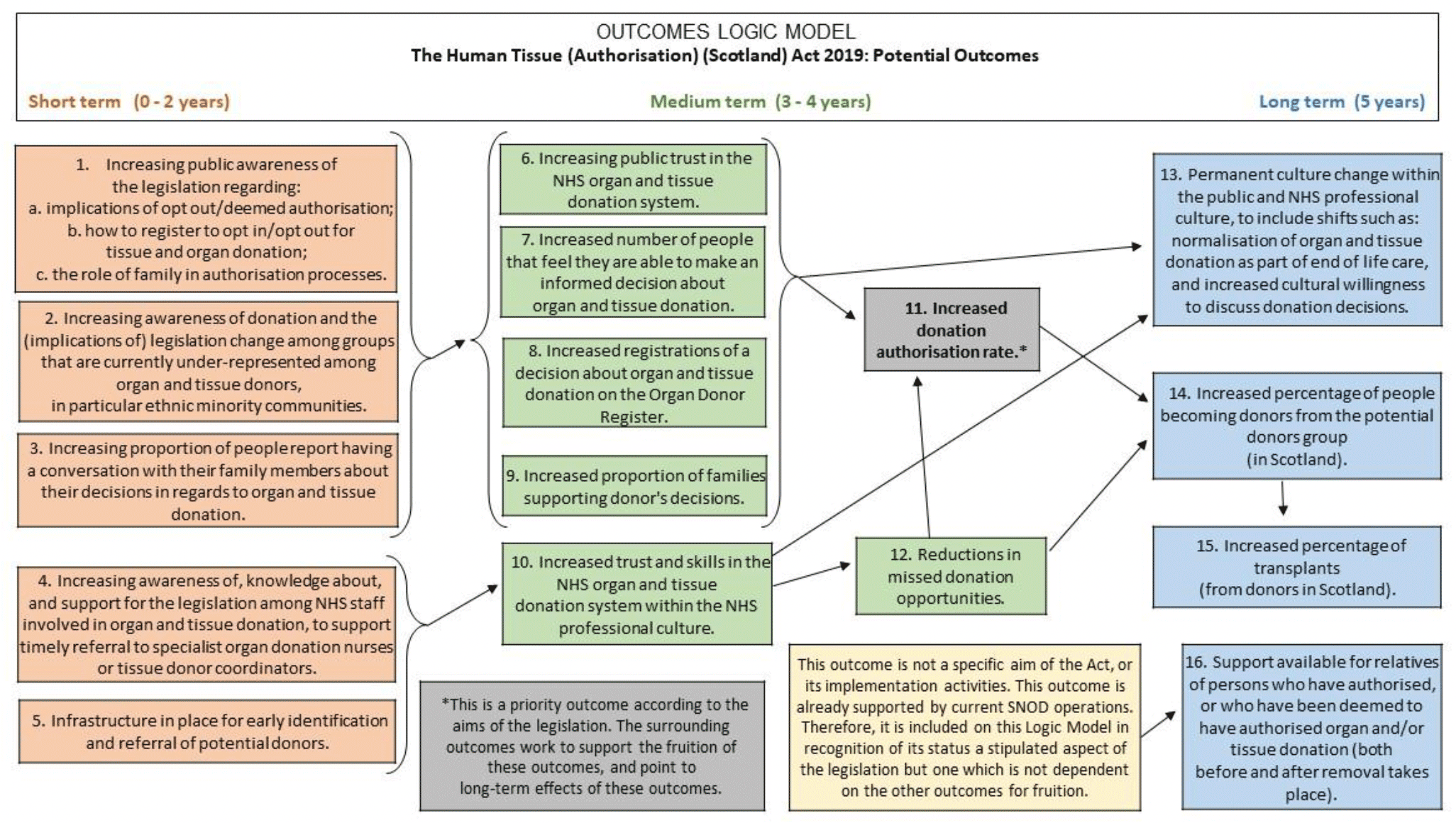
The theory based evaluation framework for the Act identified 16 outcomes:
Short term (1-2 years)
1. Increasing public awareness of the legislation regarding:
a. implications of opt out/deemed authorisation
b. how to register to opt in/opt out for tissue and organ donation
c. the role of family in authorisation processes
2. Increasing awareness of donation and the (implications of) legislation change among groups that are currently under-represented among organ and tissue donors, in particular ethnic minority groups.
3. Increasing proportion of people who report having a conversation with their family members about their decisions in regards to tissue and organ donation.
4. Increasing awareness of, knowledge about, and support for the legislation among NHS staff involved in organ and tissue donation, to support timely referral to specialist organ donation nurses or tissue donor coordinators.
5. Infrastructure in place for early identification and referral of potential donors.
Medium term (3-4 years)
6. Increasing public trust in the NHS organ and tissue donation system.
7. Increased number of people that feel they are able to make an informed decision about organ and tissue donation.
8. Increased registrations of a decision about organ and tissue donation on the Organ Donor Register.
9. Increased proportion of families supporting donor's decisions.
10. Increased trust and skills in the NHS donation system within the NHS professional culture.
11. Increased donation authorisation rate[1].
12. Reductions in missed donation opportunities.
Long term (5 years)
13. Permanent culture change within the public and NHS professional culture, to include shifts such as: normalisation of donation as part of end of life care, and increased cultural willingness to discuss donation decisions.
14. Increased percentage of people becoming donors from the potential donors group (in Scotland).[2]
15. Increased percentage of transplants (from donors in Scotland).
16. Support available for relatives of persons who have authorised, or who have been deemed to have authorised organ and/or tissue donation (both before and after organ/tissue retrieval takes place).[3]
It is important to note that while increased organ and tissue donation and transplantation rates are an aim of the legislation, they are not the most useful metric by which to measure impact of the Act. This is because there are range of contingencies, which are largely clinical in nature, between gaining authorisation for donation, and actually achieving donation and transplantation. Authorisation, referral, and approach rates describe areas of practice which are more directly impacted by a move to an opt-out authorisation system. So too are the normalisation of donation as an end-of-life care choice for patient families, and the normalisation of approaching families about donation as part of end-of-life clinical care practice. As such, a priority outcome of the Act is increasing the donation authorisation rate in Scotland (outcome 11).
The Scottish Government and Public Health Scotland developed a logic model (Figure 1), which illustrates the relationships and dependencies between the outcomes. In addition, the logic model illustrates the anticipated timeframes within which impacts on the outcomes may be seen as a result of the Act and its package of implementation activities.
For example, the success of raising authorisation rates (outcome 11) is projected to be a measureable trend toward the end of the five year monitoring and evaluation period. An increase in authorisation rates is likely to be supported by the success of outcomes 6-9 and 12, measurable at the midway point of the monitoring and evaluation period. These are in turn largely impacted by outcomes 1-3, which are likely to show first signs of impact from the introduction of the Act and its package of implementation activities. Furthermore, authorisation rates are positioned to impact on outcome 14, and in turn outcome 15.
Baseline Evaluation Questions
This report presents findings relating to key baseline evaluation questions (outlined below), which are directly related to the outcomes laid out in the logic model.
1. What are the public's views on, understanding and awareness of the new opt-out system? [outcomes 1, 6, 7, 13]
2. What are the public's views on the NHS organ and tissue donation system, and donation as part of end-of-life care? [outcomes 1, 6, 7, 13]
3. Are members of the public willing to discuss donation decisions with family, or willing to register their decision? [outcomes 3, 7, 8, 13]
4. What are NHS staff members' views on, understanding and awareness of the new opt-out system? [outcomes 4, 10, 13]
5. What are NHS staff's views on the NHS organ and tissue donation system, and donation as part of end-of-life care? [outcomes 4, 10, 13]
6. How can successful early identification and referral of potential donors, and successful authorisation processes best be supported? What supports a reduction in missed donation opportunities? What are barriers to the successful realisation of these aims? [outcomes 4, 5, 10, 11, 12, 13]
7. What are key areas that training should target to raise awareness and knowledge of, and support for tissue and organ donation, and the opt-out system among NHS staff involved in donation processes? [outcome 4, 5, 10, 11, 12]
8. What is the current authorisation rate for tissue and organ donations? [outcome 11]
9. What is the percentage of people becoming donors from the potential donor group? [outcome 14]
10. What are the number of transplants occurring (from donors in Scotland)? [outcome 15]
11. What kind of support is available for relatives of persons who have authorised, or who have been deemed to have authorised organ and/or tissue donation? [outcome 16]
Data Sources and Contextual Information
This report presents data relating to different aspects of the organ and tissue donation process linked to the intended outcomes of the Act. The aim is to provide evidence, where available, for the period preceding the implementation of the Act. The report also provides an overview of some of the activities conducted in support of, and preparation for, the Act's implementation to ensure its success across a range of outcomes. The overview of these activities provides context with which to understand how the impact on particular outcomes might have occurred – it does not serve to provide baseline evidence against which to measure impact over the five year period.
It should be noted that Outcome 2 (increasing awareness among under-represented groups) is currently not evidenced by data sources. It is, however, being addressed through implementation activities centred around stakeholder engagement and media marketing about the Act.
Data and information to evidence or contextualise these outcomes fall within three main strands:
- Public Attitudes: concerns the public's views on, attitudes toward and behaviours associated with donation
- Workforce: concerns the views, confidence, and practice of NHS Scotland staff members involved in donation processes
- Monitoring Data: refers to data currently collected by NHS Blood and Transplant (NHSBT) and Scottish National Blood Transfusion Service (SNBTS) on referral, authorisation, donation and transplantation rates
Further detail about the different sources of information that informed the baseline assessment are presented below. Table 1 shows which outcomes and information sources are associated with each of the three strands, while logic models for the three strands are presented the Annex.
Public Attitudes Strand
Data
Public Attitudes Survey
The Scottish Government commissioned the Scottish Health Council to survey members of the public about organ and tissue donation, using the Our Voice Citizen's Panel[4]. This survey collected information on awareness and understanding of the legislation, views on donation in general, as well as behaviours in relation to legislation and organ and tissue donation. The survey took place in June and July 2019.
Marketing Surveys
The Scottish Government's marketing unit commissioned five online omnibus surveys (in June 2019, September 2019, March 2020, September 2020, and January 2021) to monitor public views and attitudes towards the change to an opt-out authorisation system for donation, as well as the impacts of the media campaign to inform the public about the law change and to raise awareness about the importance of making a donation decision.
Academic and Public Sector Research
Academic research has investigated the views held by members of the UK public regarding donation and the opt-out legislation, specifically the relationship between emotional barriers related to donation and opt-in donor registrations (Miller et al 2019 and Miller et al 2021). The periods of data collection for these studies fall within the Baseline period set out in this report, namely from January – March 2018 (Miller et all 2019) and Nov 2019 – February 2020 (Miller et al 2021).
Implementation Activity
Media advertising campaign
The aim of this workstream was to inform the public about the donation law change and raise awareness about the importance of making a decision about donation, sharing that decision with one's family and registering the decision on the NHS Organ Donor Register. Awareness raising started in June 2019, culminating in a multi-media campaign from January to March 2021.
Engagement with partners and stakeholders
The aim of this workstream is to raise awareness with harder-to-reach groups, and groups with specific interests in relation to the opt-out system, to incorporate their views into the implementation of the Act. Engagement was done through targeted media channels but more specifically through stakeholder organisations working with these audiences.
Workforce Strand
Data
Qualitative research with NHS Scotland staff involved in donation
Between October 2019 and January 2020, a Scottish Government researcher undertook interviews and focus groups with staff involved in donation to gather their views. The participants included Clinical Leads for Organ Donation (CLODs), Specialist Nurses for Organ Donation (SNODS), Tissue Donation Coordinators (TDCs), Intensive Care Unit (ICU), Emergency Department (ED) clinicians and senior nurses.
NHS Staff training surveys
Confidence rating surveys pre- and post-training with NHS Scotland Staff, collected between Sept 2020 and March 2021.
Implementation Activity
NHS Scotland staff trainings
A variety of training sessions aimed at NHS Scotland staff involved in donation processes were run between Sept 2020 to Feb 2021, and an online resource was made available from Jan 2021. The aim was to ensure compliance and confidence with new legislative requirements among all operational staff involved in donation processes in Scotland.
Monitoring Data Strand
Data
NHSBT organ donation data
NHSBT publishes routine data collected on referral, family approach, authorisation, donation, and transplantation rates. This is published in the reports listed below:
- Scotland Organ Donation Services Team: Detailed Report Actual and Potential Deceased Organ Donation 1 April 2019 - 31 March 2020
- Organ Donation and Transplantation Activity Report 2019/2020
- Organ Donation and Transplantation data for Black, Asian and Minority Ethnic (BAME) communities: Report for 2019/2020
Additional Scottish data was provided by NHSBT to evidence particular outcomes, but which is not routinely published, for the purposes of this Baseline Report. This data will be made available to Scottish Government over the course of the Monitoring and Evaluation period as well.
SNBTS tissue donation data
Data is collected by SNBTS on tissue donation referral, family approach, authorisation, donation, and transplantation rates, however this data is not routinely published. This data was shared with the Scottish Government to establish baseline figures.
Organ Donation Register (ODR) data
NHSBT collects routine data on opt-in and opt-out registrations on the ODR.
| Strand | Information Source | Outcomes | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | ||
| Public Attitudes | Public Attitudes Survey | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||
| Marketing Surveys* | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||
| Academic and Public Sector Research | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||
| Workforce | Qualitative research with NHS Scotland staff | ✓ | ✓ | ✓ | ✓ | ||||||||||||
| Surveys with NHS Scotland Staff | ✓ | ✓ | ✓ | ✓ | |||||||||||||
| Monitoring Data | NHSBT: Organ Donation Data | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||
| SNBTS: Tissue Donation Data | ✓ | A | ✓ | ✓ | ✓ | ✓ | |||||||||||
| Organ Donation Register data | ✓ | ||||||||||||||||
| Implemen-tation (and potentially ongoing) activities | Activities in the section below offer monitoring information or contextual information about potential impact on the outcome, not data against which to measure impact. | ||||||||||||||||
| Media marketing campaign* | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |||||||||
| Engagement with partners and stakeholders* | ✓ | ✓ B | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||
| Training aimed at NHS Scotland staff involved in donation processes* | ✓ | ✓ | ✓ | ✓ | ✓ | ||||||||||||
| Routine, informal support offered to donor families by SNODs* | ✓ C | ||||||||||||||||
NOTES:
*The specific details of information sources marked with an asterisk (*) are still be determined, as long-term business planning within Scottish Government and the NHS is still underway.
A: SNBTS is currently reviewing how it will collect this information and the availability of this data source will be monitored.
B: There is no currently available evidence to address Outcome 2 (increasing awareness among under-represented groups) – the only available information comes from this stakeholder engagement workstream
C: Outcome 16 (support for relatives) is not impacted on by the Act's package of implementation activities.
Boxes are shaded/marked with a tick to indicate that a particular information source serves as an indicator for a particular outcome of the Act.
Contact
Email: socialresearch@gov.scot
There is a problem
Thanks for your feedback