Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME-CFS): good practice statement
Guidance to support the diagnosis and management of ME/CFS in primary care. This was originally published in 2010 and we have partially updated it to insert key recommendations from the NICE Guideline on ME/CFS published in October 2021.
4. Interventions, management and rehabilitation
4.1 General principles
Patient support and wellbeing are key – all patients will benefit from the general skills of good medical practice including being treated with respect, being listened to with empathy, and having the opportunity to build a rapport with their general practitioner. All treatment should be collaborative and clinicians should draw on their generic skills in chronic disease management. Imposed rigid programmes can be actively harmful.
In general clinicians should adopt a holistic approach in treating the symptoms of ME-CFS. No single treatment has yet been shown to be consistently effective. However, various rehabilitative approaches have often been found to be beneficial in modifying symptoms of this illness in some patients, and assisting the recovery process. While a variety of drug treatments have been suggested for people with ME-CFS, the results have generally been inconclusive or in some cases negative, when they have been subjected to well organised, randomised controlled trials (RCTs). This emphasises the continuing imperative for high quality research into the aetiology and management of ME-CFS (see also Section 7).
What works for one patient may not work for another and therefore it is crucial to tailor interventions to the needs and circumstances of the individual patient.
A standard approach to management will involve:
- It is important to give advice and support from the outset, even in the absence of a firm diagnosis.
- Acknowledge the reality of the patient's symptoms and the impact on their life.
- Share decision-making with the patient.
- Be explicit about diagnosis and co-morbidity (if relevant).
- Explain the possible causes, nature and fluctuating course of the illness, together with possible management options (benefits/risks), taking account of the person's age and the stage, severity and variability of their illness.
- Explore the range of management options that can be utilised, as appropriate to the particular patient's condition.
- Offer information on other sources of support (e.g. national charities, local groups and services). Please see Appendix 1 for further guidance.
NICE 2021 Update
Involve family members and care givers (where appropriate) when discussing care plans.
The following are usually helpful areas to discuss:
- Diagnosis: A clear diagnosis, with an explanation of why the diagnosis has been made in the particular patient's case, can be helpful and therapeutic.
- Give honest, realistic information about ME-CFS at diagnosis. Encourage cautious optimism.
- Facilitate discussion about the patient's acceptance of the diagnosis and the attitudes of other people in their life to the diagnosis.
- Suggest keeping a diary of activity levels over a four week period. Look for evidence of a 'boom and bust' approach to activity cramming lots into the 'good days' and 'paying for it' afterwards. Recommend a more consistent approach to activity planning.
- Acknowledge the difficulties in adjustment to coping with the illness.
- Offer advice on control of specific symptoms.
- Offer support and monitoring; listening, interpreting, guiding.
- Discuss the possibility of setbacks or more serious relapses and plan for how they might best be coped with.
- Support strategies with appropriate literature when available.
4.2 Interventions
Pharmacological interventions:
In general terms, it is usually beneficial to start with very low doses of medicines and then steadily increase over time. Side effects are often particularly bad during the first few weeks of exposure so try to avoid frequent changes to medication particularly between drugs in the same therapeutic class. Be alert to the problems of polypharmacy and stop medications that are not producing substantive benefits. Patients with ME-CFS are often very sensitive to the side-effects of medications (e.g. beta blockers and some antidepressants may be poorly tolerated). Note: The present evidence levels for individual interventions are summarised at the end of this section – this will evolve as further studies are published.
Pain Relief
Pain is often problematic. In addition to non-pharmacological interventions such as local heat therapy and gentle massage:
Simple analgesics – should be tried first, including – paracetamol or NSAIDs (systemic or topical), escalating to co-codamol or co-dydramol, if required. Avoid excessive use, or high doses of opiate analgesics.
- Neuropathic pain – a low dose of a sedating tricyclic, eg amitriptyline (nortriptyline is an alternative) can be used initially, especially if there is also sleep disturbance. If valuable the dose can be slowly increased. If tricyclics are ineffective, insufficient or not tolerated, gabapentin may be tried. Alternative licensed agents for neuropathic pain include: carbamazepine, duloxetine and pregabalin (the latter two may be particularly helpful if fibromyalgia is present and have level 1+ evidence for this).[7], [8], [9] Sodium valproate has also been used selectively in some patients, but it is not licensed for this indication.
- Muscle pain – sometimes accompanied by twitching, cramps and spasm. Cautious use of baclofen and benzodiazepines have been advocated by some in selected situations, but please note that there is level 4 evidence that they may do more harm than good in some cases (see below). In terms of non-pharmacological options, a TENS (Transcutaneous Electrical Nerve Stimulation) machine or acupuncture may be useful to relieve pain for some patients.
Sleep disturbance
The importance of a good sleep pattern should not be underestimated. Hypersomnia is a well-recognised problem, particularly in the early stages of the illness. It is appreciated that many mild to moderately affected patients rely on daytime and weekend sleep to allow them to work or undertake essential activities. Relaxation and meditation techniques may be useful.
A low dose of a tricyclic antidepressant or trazodone (25-50mg) should be considered to help re-establish normal sleep rhythm. As for their use in pain control, careful explanation should be given that these drugs are not being used in these situations as antidepressants. If clinically indicated, hypnotic drugs should be used in the short term only.
Headache
If migrainous, standard treatment should be used, as required. In addition to simple analgesics, 'atypical' analgesics may be tried if necessary for refractory headache. Acupuncture may also be tried for headache symptoms (see Complementary Therapies, below).
Abdominal symptoms
Treat as for irritable bowel syndrome.
Disorders of balance
Betahistine or cinnarizine may provide symptomatic relief when symptoms are intrusive or for travel and other likely triggers.
Complementary Therapies
Although unproven by clinical trials, individual patient reports suggest that acupuncture may help to relieve pain in some and that other therapies may have a role to play in improving wellbeing (see also Section 4).
Dietary regimes and supplements
Research into the efficacy of individual dietary regimens has been inconclusive. Some patients report intolerances to various foods as contributory to their gastrointestinal problems. A healthy diet should be encouraged – suggesting caffeine and alcohol minimisation, avoiding excessive intake of refined carbohydrates (sugars) and by taking frequent smaller meals and healthy snacks as required.
A normal healthy diet will include the Recommended Daily Allowances (RDAs) for essential nutrients. However if individuals are restricting their diet for some reason, nutritional supplements may be required. Many patients have reported that use of supplements may be helpful as part of a self-management strategy for their symptoms such as: vitamin B12, vitamin C, coenzyme Q, multivitamins and minerals, although the evidence base is lacking to support their routine use. The NICE Guideline recommends that all patients with moderate to severe ME-CFS should be encouraged to obtain adequate sun exposure and eat foods high in vitamin D see Section 7 for further discussion of vitamin D.
NICE 2021 Update
Those who suffer with nausea should be encouraged to maintain adequate fluid intake as well as eating small amounts regularly, Not eating or drinking can worsen nausea.
Those experiencing weight loss/gain or following a restrictive diet should be referred to a dietician with a specialist interest in ME-CFS for further assessment.
All patients who have low exposure to the sun because they are housebound or are confined to indoors for long periods of time should be advised to take vitamin D supplements.
4.3 Rehabilitation and re-enablement
In most cases the aim for management will be rehabilitation or re-enablement, in terms of regaining function, according to the patient's needs and circumstances. Re-enablement should encompass cognitive, emotional and social aspects as well as physical aspects.
Any rehabilitation or increase in activity should start from an agreed, stable and possibly very low baseline and should be gradual. Keep goals small and achievable.
Although a return to previous levels of functioning in the short to medium term is often unrealistic, patients can be encouraged to set goals that involve steadily increasing both physical and mental activities – once their condition has started to stabilise and increases in activity have been maintained consistently.
If it is felt that management strategies supervised by a therapist, experienced in ME-CFS, such as activity management and cognitive behavioural therapy (CBT) may be beneficial, the choice of programme, its components and progression must be agreed by the patient and therapist and that patient and therapist are viewed as a partnership. 'Rehabilitation' does not necessarily have to mean 'exercise' – it may refer to any activity.
NICE 2021 Update
Support from a physiotherapist/occupational therapist may be of particular benefit to those wishing to add physical exercise to their routine. The exercise should be tailored to those with ME-CFS rather than an exercise programme designed for the general population.
Progress must be regularly monitored a relapse must trigger a reassessment of the management plan. Fluctuations in the illness are natural and may include natural plateaux which may last for a number of years, setbacks or more substantial relapses. Such fluctuations would indicate a need to reassess the management plan or for activity levels to be slowed down. Not all patients may benefit from activity strategies and some have reported feeling worse from this therapy.
Other aspects are also important, particularly in young people e.g. education and training, development etc. Adults may also not be able to undertake their original job and may need careers advice and re-training. People with ME-CFS are as potentially disabled as those with other chronic conditions and are therefore entitled to apply to the Department for Work and Pensions for the full range of sickness and disability benefits – this is covered further in Section 8.
4.4 Physical functioning and mobility
NICE 2021 Update
When considering strategies to help maintain and prevent deterioration of physical functioning and mobility in the care and support plan it is important that these are in small amounts and spaced throughout the day.
Particular areas to consider are:
- Joint mobility
- Muscle flexibility
- Balance
- Postural and positional support
- Muscle function
- Bone health
- Cardiovascular health
It is important to be aware that those with severe to very severe ME-CFS and those with long periods of immobility will need assessed for the following at each clinical review:
- Pressure ulcers
- Deep vein thrombosis
- Risk of contractures
It is vital that those who are helping to support and care for the patient with ME-CFS are given advice on how to help maintain physical functioning and mobility. For example:
- Bed mobility
- Moving from lying to sitting to standing
- Transfers between furniture
- Correct use of mobility aids
- Joint mobility
- Muscle strength and stretching
- Balance
- Mobilising around the house including stairs
4.5 Energy management
NICE 2021 Update
NICE define graded exercise therapy (GET) as first establishing an individual's baseline of achievable exercise/physical activity, then making fixed incremental increases in the time spent being physically active.
After reviewing the evidence based on this definition of GET, the NICE guideline update in October 2021 does not recommend GET as an effective therapy for ME-CFS and that this approach should not be undertaken. It states that an individualised approach to physical activity/exercise should be taken instead. This supersedes the existing Scottish Good Practice Statement guidance.
Activity management or pacing is a way of managing the reduced 'energy envelope' of people with ME-CFS. Patient experience indicates that adequate and good quality rest is also important, especially in early stages and during relapses. Gaining the balance between activity and rest can be difficult. It will vary from patient to patient and also during the course of the illness in any patient. It is important to avoid periods of 'boom and bust' in energy expenditure, both physical and mental. Many patients will try to squeeze as many of the weekly activities and tasks into a 'good day' and 'pay for it' the next. Instead, it is advisable that activities should be spread out more evenly and regularly.
- Activity management is an approach that is customised to the needs of the person with ME-CFS. It is based on an understanding that all activities have physical, emotional and cognitive components, and on identification of those components.
- Pacing is largely a self-management technique with the underlying approach being to establish sustainable activity levels. A safe, consistent and often low baseline of activity (mental as well as physical) should be established which avoids setbacks (including delayed reaction). A diary may help to establish patterns of activity. This is widely considered by patients to be the most helpful intervention. Appropriate, good quality, literature is essential. Setbacks and relapses are crucial reasons to re-evaluate the management plan. Support can be obtained from literature from ME charities eg the Action for M.E. booklet on Pacing (see Section 8). This approach is currently being tested in a large randomised trial, which has now finished recruiting, and more will be known of its effectiveness in the near future.[10]
Graded exercise therapy (GET) is intended to redress decline in physical fitness due to inactivity.[11], [12] GET has proved to be a particularly controversial form of treatment which many patients have concerns about and some patients have indicated that GET has worsened their symptoms (see below). GET makes use of an exercise programme involving a gradual increase in exercise/activity. It must be delivered by a suitably trained GET therapist with experience in ME-CFS, ideally on a one-to one basis.[13] Where fibromyalgia is also present, supervised aerobic exercise therapy may help physical capacity and relieve pain symptoms.
Some patients with ME-CFS report that exercise programmes have been applied inflexibly at times, without consideration of individual circumstances and goals, sometimes with significant adverse responses. It is essential that agreement and negotiation are at the very centre of any GET programme.[14]
4.6 Cognitive behavioural therapy (CBT)
Counselling lacks a robust evidence base, but as with any chronic illness, counselling from a trained counsellor/nurse may be helpful, particularly in the early stages of the illness, in supporting patients as they learn to manage the consequences of ME-CFS.
Cognitive behavioural therapy (CBT) can be used, as in other chronic physical medical conditions, as a tool to aid people develop better ways of coping with symptoms such as fatigue, pain and sleep disturbance. CBT may be of value to patients when their symptoms have led to a psychological response that has compounded their problems.
NICE 2021 Update
NICE highlight that CBT has sometimes been assumed to be a cure for ME-CFS. However, it should only be offered to support people who live with ME-CFS to manage their symptoms, improve their functioning and reduce the distress associated with having a chronic illness.
It should only be offered after discussion with the patient and they would like to use it to support them in managing their symptoms, CBT for children and young people should be adapted to their cognitive and emotional stage of development.
CBT for ME-CFS does not assume people have 'abnormal' illness beliefs and behaviours as an underlying cause of their ME-CFS, but recognises that thoughts, feelings, behaviours and physiology interact with each other.
The sessions should help the person develop a self-management plan that is reviewed regularly if symptoms should change.
4.7 Managing flare-ups and relapses in symptoms
NICE 2021 Update
It is important to counsel patients that flare-ups and relapses can occur despite having well managed symptoms. It should not be assumed that new or changes symptoms are related to ME-CFS and should be assessed and investigated as needed.
A flare up is defined as experiencing a worsening of their symptoms that is beyond their normal day-to-day fluctuations that can last a few days.
A relapse is defined as sustained and marked exacerbation of symptoms lasting longer than a flare-up that needs substantial and sustained adjustment of energy management.
Preparation for a flare or relapse should be discussed in the person's care plan to allow them to react quickly.
Flare-ups:
- Identify possible triggers e.g. exercise, illness
- Temporarily adjust activity levels
- Monitor symptoms in case they develop in to a relapse
- Only return to normal activity levels once flare up has fully resolved
Relapses:
- Identify possible causes
- Reduce or even stop some activities
- Increase frequency or duration of rest periods
- Reassess energy limits to stabilise symptoms
If the care plan is robust the patient should be able to self-manage flare-ups or relapses. However if the strategies are not effective or there is a concern regarding symptoms they should seek support from their primary care team or ME-CFS specialist. Following a flare-up or relapse the person's care plan should be reviewed and amended as required. If there were clear triggers, strategies could be put in place to avoid these in the future.
In general those with ME-CFS should have their care and support plan reviewed in primary care on at least an annual basis At this review there should be discussion with regards to current and new symptoms, their general wellbeing and details of their support system. Future plans and goals should be recorded.
4.8 Evidence levels for interventions
At the present time[15] the strongest graded scientific evidence is in support of:
(1) pharmacological interventions for associated symptoms – duloxetine or pregabalin,where neuropathic pain and/or fibromyalgia are present; and (2) rehabilitative strategies – cognitive behavioural therapy (CBT)[16], [17] and graded exercise therapy (GET), recognising that such interventions need to be carefully matched to the needs of individual patients.[18]
The summary data from the Cochrane collaboration reviews, based on randomised controlled trial (RCT) studies data in 3789 patients (comprising 1043 patients in CBT studies for CFS, 470 in GET studies for CFS19 and 2276 subjects in supervised aerobic exercise for fibromyalgia),[19] which support these treatments, is provided in the grading below. Such treatments are in line with standard neurorehabilitation principles. It is often assumed that the efficacy of such treatments suggests that the underlying illness must be 'psychological'. This is not the case and there is now high quality evidence that CBT leads to demonstrable changes in brain functioning and structure.
However, as indicated above, CBT and GET will not be effective for all patients and remain controversial. In 2008, a survey of over 2760 people with ME-CFS, undertaken by Action for M.E. found that 82% of respondents had found pacing most helpful. 50% found CBT helpful and 45% of those who said that they received graded exercise therapy (GET) found it to be helpful. However, 34% of patients who said they had received GET or graded activity and 12% of those who said they had received CBT since 2005, reported that they felt worse. A further survey of 4217 patients and carers reported by the ME Association in 2010, found pacing most helpful (71% of respondents improved), 26% found CBT helpful and 22% found GET helpful. 5% felt worse on pacing, 20% worse on CBT and 57% worse on GET. This latter survey had a high proportion of respondents (44%, who indicated that their illness had been present for more than ten years.
These expressed concerns from patients with ME-CFS about CBT and GET, were reinforced by many comments received from patient representatives during preparation of this guidance. They clearly indicated that patients with ME-CFS should not be pressed into accepting unwanted treatments and as for all other medical conditions, had the right of refusal of any specific treatment offered.
If a patient wishes to explore these forms of treatment, it is important that such treatments are supervised by therapists working in teams with specific expertise in ME-CFS. The choice of programme, its components and progression must be agreed by the patient and therapist and that patient and therapist are viewed as a partnership.
The use of such rehabilitative treatments should not be confused with non-specific advice to be 'more active', or to go to the gym and 'do some exercise'. Such approaches are usually highly unproductive.
Grading of evidence
The grading of level of evidence has been made in accordance with the SIGN Guidelines approach.When coming to a decision about specific treatments for individual patients, and in keeping with recent SIGN developments, due weight must also be given to people's experience of living with ME-CFS. Research evidence continues to evolve and further details are available at Improving patient care through evidence‑based guidelines[20] This key issue is discussed further in Section 6, in relation to the importance of professional clinical judgement in the context of limited scientific evidence.
Interventions that benefit some, but not all:
(Level 1+ evidence)
- Duloxetine or pregabalin (for pain relief, where neuropathic pain and/or
- fibromyalgia present)
- Cognitive Behavioural Therapy (when delivered in centres with specific expertise in treating ME-CFS)
- Graded Exercise Therapy[21] (when delivered in centres with specific expertise in treating ME-CFS). Where fibromyalgia is present, supervised aerobic exercise therapy may help physical capacity and relieve pain symptoms.
Interventions that may benefit some, but not all:
(Level 4 evidence)
- Acupuncture (particularly for headache)
- Gabapentin
- Pacing
- 'Step 1' analgesics
- Transcutaneous Electrical Nerve Stimulation (TENS)
- Tricyclic antidepressant drugs (starting with a low dose)
Interventions that possibly work and are unlikely to do harm: (Level 2- evidence)
- Acetyl-L-carnitine and propionyl-L-carnitine supplements
- Essential fatty acid supplements
- Massage therapy
- Melatonin
Interventions for which trials have shown a lack of benefit:
(Level 2- evidence and above)
Acyclovir, acyclidine, alpha interferon, amino acids, ampligen, clonidine, dexamphetamine, fludrocortisones, fluoxetine, galantamine, ganciclovir, general dietary supplements, growth hormone, homeopathy, hydrocortisone, inosine pranobex, interferon, liver extract, low sugar/low yeast diet, magnesium, medicinal mushrooms, moclobemide, ondansetron, osteopathy, phenelzine, pollen extracts, selegiline, sulbutiamine, terfenadine, topical nasal corticosteroids.
Interventions that may do more harm than good:
(Level 4 evidence)
Amantidine, antifungal drugs, baclofen, benzodiazepines, methylphenidate, naltrexone, nimodipine, thyroxine (except where patients have a diagnosis of hypothyroidism), non specific advice on activity (e.g. 'go to the gym and do some exercise').
Interventions that do more harm than good:
(Level 2- evidence)
Immunoglobulins, oral NADH, Staphylococcus toxoid. The above appraisal of evidence levels draws on the systematic review undertaken by the Centre for Reviews and Dissemination, University of York in 2007.18 Research evidence continues to accrue into the management of ME-CFS,which is discussed further in Section 6.
4.9 Rating scales
When a patient presents to a GP with symptoms consistent with ME-CFS, it may be helpful to ask the patient to fill out a rating scale and complete a body pain map. These documents allow a lot of clinical information to be communicated succinctly. This may aid management. They can also be used in ongoing monitoring of the clinical condition. A severity rating scale is provided in Appendix 3. A sleep and pain profile is provided in Appendix 4. Both are adapted from the Canadian Consensus Document (see Appendix 2).
4.10 Referral for specialist assessment
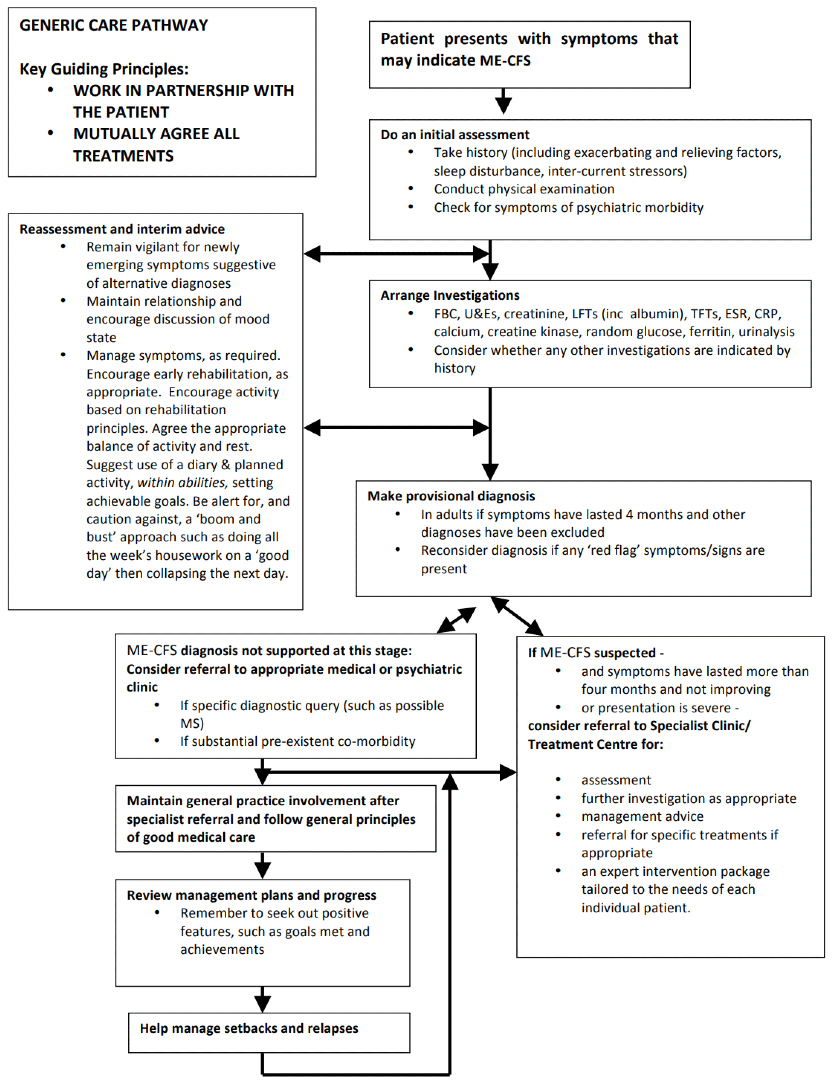
Care Pathway
At present services throughout Scotland are not uniform. It is hoped that the Scottish Public Health Network's Health Care Needs Assessment for people living with ME-CFS[22] and the NHS QIS Clinical Standards for Neurological Health Services[23] will help to resolve this. Different care pathways will need to be developed for groups with particular requirements such as children and young people (Section 5); those severely affected (Section 6), including housebound or bedbound; and those living in rural areas. Referrals may need to be made to designated clinical services, for assistance with the management of patients in those whom the diagnosis has been made or to the appropriate medical specialty in situations where there is diagnostic doubt.
A generic diagnostic, management and referral algorithm (care pathway) has been incorporated into the accompanying Quick Reference Clinical Guide and is reproduced again below, for ready reference.
4.11 Prognosis
The prognosis is variable. The majority of patients will show some degree of improvement over time, especially with treatment, although many will pursue a fluctuating course with periods of relative remission and relapse. Patients in primary care also present with milder fatigue states that have a much more favourable prognosis. However there is a significant minority, who are severely affected for many years and in extreme cases, for decades. Further studies are required to inform this issue.
Further Information on Clinical Management
Further information on the clinical management of adults with ME-CFS, is available in publications listed in Section 8 – References.
4.12 Diagnostic, management and referral algorithm/care pathway
Children and young people
Children and young people (CYP) can be as profoundly affected by ME-CFS as adults – it can significantly impact on the young person's development and academic progress. Symptoms may have similar severity to adults but the fluctuation in severity can be much more dramatic. Severe exhaustion, weakness, pain and mood changes make life very challenging for children (as well as adults) with ME-CFS.
It is recognised that the diagnosis and management of ME-CFS in children and young people is an area which needs to be developed in a specific Good Practice Statement. Detailed guidance has been prepared by the Royal College of Paediatrics and Child Health (2004), including an extensive literature review.[24]
In the absence of a specific Scottish Good Practice Statement for Children and Young People the following is therefore intended to provide summary, interim guidance only.
4.13 Prognosis
The limited evidence available suggests that children and young people with ME-CFS are more likely to recover than adults. Studies with extended follow up show 60-80% partial or complete recovery with an average duration of illness of 37.5-49 months, with about 20% of cases remaining incapacitated, some for many years. Severely affected young people may be bedbound and the impact should be recognised on the other members of the family, particularly other vulnerable children and adults.
4.14 Principles of care
The principles of care in children and young people are common to many chronic conditions. Most of the issues covered for adults also apply to children. Some need different emphasis. This can impact upon a young person's development and adversely affect family life. It is therefore crucial that the child and his/her parents or carers are carefully listened to.
Effective translation of the principles of the Scottish policy: Getting it right for every child (GIRFEC), into effective practice should occur to ensure that children and young people with ME-CFS and their families receive optimal care and support.
The GIRFEC principles for children, young people and their families are that they feel confident about the help they are getting; understand what is happening and why; have been listened to carefully and their wishes have been heard and understood; are appropriately involved in discussions and decisions that affect them; can rely on appropriate help being available as soon as possible; and that they will have experienced a more streamlined and coordinated response from practitioners.
Speedy diagnosis of ME-CFS is important to allay fears of other serious illness, to protect the patient from undue pressure and to allow symptom control and appropriate management to begin.
This should prevent further deterioration in many, but not all, cases. Management should be geared to the specific condition of the individual child or young person and agreed with the parents/carers.
NICE 2021 Update
When discussing the diagnosis it is important to take in to account the child or young person's age and level of understanding. They may have different communication needs and may benefit from interactive formats e.g. written materials and pictures, digital media or play activities.
4.15 Clinical presentation
The range of possible presenting symptoms is similar to adults (see Section 2). Children and young people tend to have numerous symptoms of similar overall severity, but their hierarchy of symptom severity may vary from day to day. Severe, generalised pain is a common feature. Debilitating fatigue (both physical and mental) is the most commonly reported symptom, typically exacerbated by exercise or activity. They may become tearful, physically weak and exhibit exhaustion or profound mood changes.
Loss of energy/fatigue
The loss of energy and weakness may be so profound as to make the child bedbound. Post-exertional fatigue and weakness will affect the ability to undertake exercise or sport. The severity of symptoms will affect the ability of the child to attend school (see below).
Cognitive problems
Slowing of thought processes occurs work involving abstract thought is difficult to perform in all cases. Even if the child usually starts a task well, a rapid deterioration in cognitive abilities often takes place, which may be accompanied by exacerbations of other symptoms. Impairment or 'fogging' of thinking and forgetfulness are common, as are attentional difficulties – poor retention and recall – e.g. lack of recollection of magazine articles read only a few minutes previously. Cognitive abilities may deteriorate particularly in topics requiring analysis, multi-task activities, fast-paced and confusing environments and with physical, mental and emotional fatigue.
Disordered sleep pattern
Phase delay and interruptions are the commonest reported problems.
Weight change
Both loss and gain occur, with reports that weight loss in the early stages can be significant. Maintenance of height and weight charts has been recommended in all paediatric cases of ME-CFS. Specific dietetic assessment is essential where weight loss is severe.
Gastro-intestinal disorder
Gastrointestinal upset is common.
Diarrhoea has been reported as particularly distressing in some children.
4.16 Diagnosis and investigations
Diagnostic criteria
As for adults, a significant problem in the literature is the lack of both an agreed paediatric definition of ME-CFS and a reliable instrument to assess it. This is discussed further in the Royal College of Paediatrics and Child Health (RCPCH) Guideline.[25]
Investigations
Similar investigations should be considered as for adults when pursuing a differential diagnosis of ME-CFS (see Section 2).
NICE 2021 Update
It is especially important to exclude alternative treatable causes of fatigue e.g. cancer or occult infection in a timely manner.
Time to diagnosis
Children may be diagnosed with ME-CFS when symptoms have lasted for more than three months. A working diagnosis may be made after a much shorter time.
NICE 2021 Update
Suspect ME-CFS in those children and young people who display the 4 key symptoms that are not explained by another condition for a minimum of 4 weeks compared to 6 weeks in adults.
4.17 Clinical management
The Royal College of Paediatrics and Child Health (RCPCH) Guideline[26] has advocated a comprehensive management plan including as a minimum:
- Activity management advice – including establishing a baseline of activity level and gradual increases as appropriate.
- Advice and symptomatic treatment – as required.
- Early engagement of the family as well as maintaining a therapeutic alliance throughout the illness, this is crucial for successful implementation of the management plan.
- Regular review of progress – particularly those who have not made significant progress, making it clear that it is not the fault of the child or young person.
Advice is also provided by the RCPCH Guideline[27] on diet, sleep problems, pain management, psychological support and co-morbid depression where present.
Careful attention to psychological wellbeing and potential co-morbidities is an important part of the assessment and management of ME-CFS in children and young people.
Further advice on interventions – CBT, GET[28] and pharmacological advice is also offered, including trying complementary therapies where patients and families express an interest, if it does not interfere with current treatment. The RCPCH Guideline[29] also notes that prolonged bed rest or complete inactivity should be avoided, wherever possible, as physical deconditioning is likely to exacerbate fatigue and weakness.
NICE 2021 Update
It is important that education or training is not the only activity the child or young person takes part in. They should aim to find a balance between education, family and social activities.
Care needs
A child can be so profoundly affected that the family may require practical help and support in the home setting. This may take the form of aids prescribed by a community occupational therapist (OT). Specific care packages may need to be drawn up for those more severely affected (see also Section 6).
Referral
GPs would normally consider this an area of specialist expertise and patients with suspected ME-CFS should be referred to paediatric services for further assessment.
As indicated above, diagnosis by 3 months is both possible and desirable in a child or young person with suspected ME-CFS. While referral should normally be made to a paediatrician in the first instance, the assessment and subsequent management should be a multidisciplinary process with the engagement of medical, nursing, AHP (allied health professional) staff and, if appropriate, child and adolescent mental health services.
NICE 2021 Update
It is important to involve the child's or young person's place of education early in the process to allow adjustments to be made where necessary.
Where a young person's mobility and daily living is affected with ME-CFS, referral to a community OT could also be valuable and would contribute to the overall needs assessment. It could be particularly useful in more severely affected cases where there are muscle problems and problems with mobility. There may be a need for appropriate training in ME-CFS for all relevant staff involved.
Hospital admission
The majority of children and young people with ME-CFS can be managed at home with appropriate support from the GP and the local paediatric team. However, there may be some circumstances when a hospital admission is helpful, for example the assessment or initiation of a management plan when the expertise is not available on an outpatient basis. Where admission is felt to be appropriate, the rationale should be carefully prepared and presented as a recommended option to young persons and their families.
Monitoring and review
The RCPCH Guideline[30] indicates that there is no research evidence on the effectiveness of different models of ongoing care for children and young people with ME-CFS but also notes that in one research study, the GP was the primary carer in 62% of cases and the paediatrician in 24%.
Children and young people with ongoing ME-CFS will require regular review and there should be a clear management plan in place, identifying the lead professional to coordinate care, particularly across health and educational sectors.
NICE 2021 Update
Recommend reviewing the CYP care and support plan at least every 6 months.
The lead professional role will depend on individual skills, preferences, local resources and illness severity, but must be identified and agreed with the child/young person concerned and their parents/carers, in accordance with GIRFEC principles. Robust communication lines must be clearly defined for all those involved in this process.
4.18 Schooling and higher education
As a result of physical and mental activity levels being reduced, pupils have difficulty at school or are unable to maintain a full school programme.
There is a substantial body of research showing that ME-CFS can cause a significant disruption to education. The length of school absence depends on illness severity, ranging from part-time attendances to absences of several years with home tuition as the only educational exposure. Children and young people with ME-CFS may miss more school than those with juvenile arthritis, cystic fibrosis or migraine. Children with better physical function are more likely to attend school.[31] In one UK study, 42% of pupils with certificated long-term school absenteeism were reported as suffering from ME-CFS. A further detailed study in Edinburgh secondary school pupils, has reported lower rates of absence (8%) due to chronic fatigue syndrome.
It is important to exclude and manage other defined causes of schools absence, for example school phobia or major depressive disorder, which have a different pattern to those depressive symptoms seen in patients with ME-CFS, if/when present as a co-morbid disorder. Cognitive difficulties, mental fatigue, disrupted sleep pattern, poor concentration, social withdrawal and the physical demands of travelling to school are likely causes of school absences, whilst in some cases family circumstances, social factors and anxiety may also play a part.
The school may require a supportive letter from the pupil's doctors (GP and/or paediatrician) outlining the patient's medical condition and the limitations this imposes, and advising on accommodations the school can make to take account of the impact of the illness on the child. Good and open communication between the school and the pupil's doctors is helpful. Arrangements should be responsive to the child's condition and take advantage of times when the child has more energy. Children attending school may not be able to undertake a full day and appropriate rest breaks in appropriate facilities should be organised. Where children are unable to attend school, home tuition support may be required and statutory guidance/provisions must be followed.
A close working relationship between the clinical team caring for the patient with ME-CFS and the school is recommended – and should begin as soon as a diagnosis is made.
This facilitates raising staff awareness, establishing the child's/young person's pre-morbid abilities and integrating educational needs into a comprehensive management plan, as and when appropriate. An appropriate individualised educational plan should be identified, implemented and monitored.[32] In more severe cases, the development of a coordinated support plan (CSP) would be appropriate. Additional Support for Learning (ASL) officers, based in local authorities, could also provide help and educational support for children and young people with ME-CFS.
Note: For further assistance – Children in Scotland runs Enquire, a telephone helpline for advice on educational support needs. (Email: info@enquire.org.uk; Children in Scotland).
Child protection issues
There have been concerns that misunderstanding and lack of information about ME-CFS in education and social services have led to inappropriate initiation of child protection procedures. Concerns have also been raised that child protection procedures have been initiated because of disagreements between families and health and education professionals over treatment plans. In addressing this area, the report of the Working Group on CFS/ME to England's Chief Medical Officer (2002), noted: "Neither the fact of a Scottish Good Practice Statement on ME-CFS[33] child or young person having unexplained symptoms, nor the exercising of selective choice about treatment or education for such a child constitutes evidence of abuse." This is a particularly worrying area for parents and carers of children with ME-CFS, requiring the highest levels of professional awareness and sensitivity. As for any other illness, children with ME-CFS may suffer harm and this should be considered as a possibility when preparing the differential diagnosis. As for other aspects of children's care, it is important to listen to the child, as well as to family members and patient/carers, to respect their experiences, and to give due weight to their views, especially the child's. Further guidance on child protection issues for professionals working in health, social services and education, is available from the Association of Young People with ME (AYME)[34] and Action for M.E.
NICE 2021 Update
NICE guideline states that recognising and responding to possible child neglect is complex and should be considered in the same way for those with confirmed or suspected ME-CFS as with any child with a chronic illness or disability. If a person requires a safeguarding assessment it should involve professionals with training and experience in ME-CFS as soon as possible.
It is important to recognise that those with severe or very severe ME-CFS are at risk of having their symptoms confused with signs of abuse or neglect. NICE state that the following are not necessarily signs of abuse or neglect in children with confirmed or suspect ME-CFS:
- Physical symptoms that do not fit a commonly recognised illness pattern
- More than one child or family member with ME-CFS
- Disagreeing with, declining or withdrawing from any part of their care and support plan either by them or by their patents or carers on their behalf
- Parents or carers acting as advocates and communicating on their behalf
- Reduced or non-attendance at school
RCPCH advise that if a child is thought to have severe/very severe ME-CFS resulting in withdrawal from school or school absence or has symptoms that manifest similarly to those that raise typical safeguarding concerns that more frequent in person reviews by a specialist would be of benefit to ensure wellbeing of the child: Myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome (ME/CFS) – Member briefing on new NICE guideline | RCPCH
Transition to adult services
In many cases where ME-CFS is ongoing into early adulthood, and the patient is presently being cared for by a paediatric team, formal handover of care to another health specialist service may be required. This process, often referred to as transition, can be difficult for patients, especially where it involves the ending of a positive relationship between the paediatric team and their patients built up over a substantial period of time. Any transition may require increased input from services – eg from childhood to adolescence to adulthood, starting or stopping school – and represents an opportunity, if not a requirement to review the management plan with patient and parents/carers. A multidisciplinary meeting might facilitate the smooth transition of care, particularly for complex cases. The RCPCH Guideline[35] recommends that paediatricians should ensure that their clinic or hospital has a policy for the transition of care of adolescents with chronic illness. This policy needs to be flexible enough to be adapted to meet the individual requirements of adolescents with ME-CFS.
Further information
Further information on the management of children with ME-CFS is available in the Royal College of Paediatrics and Child Health Guideline[36] and from other publications listed in Section 9 – References. Further information on Getting it right for every child is available from The Scottish Government.[37]
Contact
Email: Clinical_Priorities@gov.scot
There is a problem
Thanks for your feedback