A healthier future: Scotland's diet and healthy weight delivery plan
Sets out how we will work with partners in the public and private sector to help people make healthier choices about food.
Outcome 3: People have access to effective weight management services
Evidence tells us that there is an increased risk of developing serious diseases, such as heart disease, cancer and type 2 diabetes, for people who are overweight or obese, as well as potential psychological and emotional consequences. [45] But with nearly one third of children and two thirds of the adults in Scotland overweight and obese we know that for complex and wide ranging reasons maintaining a healthy weight in childhood and adulthood can be extremely challenging. [46]
This is why it is important that there is fair access to suitable, supportive and effective weight management services that provide support and advice, free from stigma and bias, to help more children, young people and adults in Scotland achieve and maintain a healthy weight.
There is already good practice happening across Scotland that provides effective support to those who need it. We want to build on this, focussing on prevention and early intervention, particularly for those adults where the signs of health harm are already indicated, to ensure there is good quality provision and equity of access right across our communities.
Weight management services for people with, or at risk of, type 2 diabetes
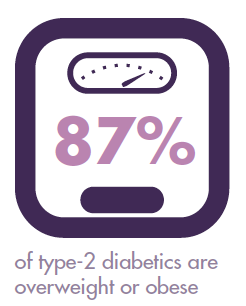
Type 2 diabetes can have a serious impact on people's lives – such as cardiovascular disease, sight loss and amputation – putting a significant amount of pressure on our health service. Worryingly, we are seeing the number of people in Scotland living with type 2 diabetes growing. In 2016, more than 250,000 people in Scotland (4.8% of the population) had a registered diagnosis of type 2 diabetes, and there are around 17,000 new cases each year. [47] Not all those living with type 2 diabetes have been diagnosed. It is estimated that around 10% of cases of type 2 diabetes remain undiagnosed. [48] Diabetes Scotland also estimates that over 500,000 people in Scotland are at high risk of developing type 2 diabetes. [49]
Evidence presented in the Scottish Government's National Clinical Strategy noted that clinicians may be too ready to move to medication rather than supporting people to make serious progress in lifestyle change to move towards a healthy weight. [50] We do know however that through changes in diet and lifestyle it is possible to delay, prevent and even reverse type 2 diabetes and its associated morbidity. [51]

By targeting support for those with, or at risk of, type 2 diabetes we could therefore change this trajectory and make a positive impact on our population health.
Action 3.1 The Scottish Government will invest £42 million over five years to establish supported weight management interventions as a core part of treatment services for people with, or at risk of, type 2 diabetes. This will be supported by a type 2 diabetes prevention, early detection and early intervention framework, to be published in summer 2018, which sets out national level guidance for Health Boards and their partners on designing and implementing an integrated type 2 weight management service.
Action 3.2 In 2018-19, the Scottish Government will work with 'early adopter' Health Boards and their partners to embark on the first phase of implementation of the framework. The early adopters will be East Region ( NHS Lothian, NHS Borders and NHS Fife), NHS Tayside and NHS Ayrshire & Arran. The learning from the early adopters will support and inform the second phase of the implementation of the framework to all Health Boards across Scotland from 2019-20.
Action 3.3 The Scottish Government will appoint a professional advisor in 2018 to work with Health Boards to deliver the framework and to support them to carry out community-led engagement and partnership, working as a core part of their service planning and delivery, in line with our wider approach to public health.
Action 3.4 The Scottish Government will monitor and evaluate the effectiveness of the framework through existing databases. Specifically, we will track the reduction in drug prescriptions for type 2 diabetes care, sustained weight management and incidence of type 2 diabetes, and introduce new measures to monitor uptake and completion of weight management interventions. In the longer term, we will monitor the incidence and prevalence rates of type 2 diabetes, and the reduction and delay of complications, such as cardiovascular disease, sight loss and amputation.
Action 3.5 The Scottish Government will run a media campaign to support the type 2 diabetes framework.
Source: Food Standards Scotland Situation Report 2018

Adults have access to effective weight management services
As well as a focus on type 2 diabetes, we want to continue to fund and encourage people to access appropriate weight management programmes and interventions that are tailored to their needs.
Action 3.6 The Scottish Government will continue to fund Health Boards to deliver weight management interventions to support sustained improvements to weight and diet for overweight and obese adults, focusing on those from deprived communities.
Action 3.7 NHS Health Scotland will work with its partners to develop evidence-informed and cost-effective minimum standards and pathways for weight management programmes for adults by 2019, with consistent monitoring of outcomes across Scotland by 2020. This is with the aim of improving the quality and equity of access to weight management services for adults across Scotland.
Action 3.8 In 2018-19, the Scottish Government will continue to fund healthy weight interventions designed and delivered by the third sector, such as Football Fans In Training ( FFIT). [52] FFIT is a 12 week programme aimed at improving both men's and women's health and wellbeing by supporting them to improve lifestyle choices, increase physical activity and reduce weight.
Children and parents have access to effective weight management services
Our primary focus is on prevention. However, too many children in Scotland are already an unhealthy weight. To make progress on our national ambition and reduce health risks in later life, it is essential that they, and their families, are well supported to achieve a healthier weight. We therefore need to have the means to monitor weight from birth through to adolescence, and to offer families appropriate support. There are systems we can build on, such as the child health reviews that include height and weight measurement, in the Universal Health Visiting pathway. [53] And every primary school in Scotland currently measures children at P1 (this data is then collated for the purposes of national measurement). However, if we are to grip the challenge of childhood obesity, we need a more robust approach.
Action 3.9 The Scottish Government will continue to fund Health Boards to deliver weight management interventions to support sustained improvements to weight and diet for at risk children, young people and families, focusing on those from deprived communities.
Action 3.10 To improve quality, and equity of access, NHS Health Scotland will continue to support Health Boards to deliver Child Healthy Weight Interventions and will, by 2020 develop evidence-informed and cost-effective minimum standards, referral pathways and outcomes.
Action 3.11 The Scottish Government will appoint a professional advisor in 2018 to support the development of consistent and systematic approaches to identification, referral and support for children and young people who are overweight and obese, and their families. As part of this work, we will explore current practice, evidence and cost-effective options for improving tracking, support and data beyond Primary 1.
People do not experience weight related stigma
Evidence shows that people with obesity experience stigma from employers, health professionals, the media and from family and friends. Obesity stigma and weight bias have been associated with low self-esteem, depression and avoidance of medical care, and therefore could be a barrier to accessing support that could help people live healthier and happier lives. [54]
Action 3.12 NHS Health Scotland will work with Health Boards to develop consistent and accessible healthy weight information and appropriate professional training - including training on weight bias and obesity stigma - by 2020.
Contact
There is a problem
Thanks for your feedback