Pain management service delivery framework: implementation plan update
The implementation plan update (2023) sets out our priorities and the actions we will take to reduce the impact of chronic pain on quality of life and wellbeing and improve information, care and services for people in Scotland.
Updated Actions
Aim A – Person Centred Care
1 We will continue to develop chronic pain information and resources - Long Term
2 Establish a Chronic Pain knowledge hub for healthcare professionals to promote understanding and learning on chronic pain - Medium Term
3 Develop a pain informed care toolkit for healthcare professional to promote care in all settings - Medium Term
4 Enhance coordination of community and third-sector support for people with chronic pain - Long Term
5 We will work with people with lived experience to identify issues for public awareness - Medium Term
Aim B – Accessible Care
6 Improve co-ordination and planning of specialist pain services - Long Term
7 We will work with Health Boards to deliver a new digital approach to improve the choice of people with chronic pain in how they engage with services - Medium Term
8 Convene a national expert working group to identify opportunities for improving pain services and their delivery - Short Term
9 We will work with the Scottish National Residential Pain Management Programme and relevant stakeholders to consider the services offered to ensure the programme best meets the needs of patients across Scotland - Medium Term
10 We will work with key stakeholders to consider the creation of National Standards for Chronic Pain Management - Medium Term
Aim C – Safe, Effective Support
11 Update clinical guidelines for management of chronic pain to deliver evidence based care and support - Medium Term
12 Promote safer, more effective prescribing for people with chronic pain - Medium Term
13 Delivering a national approach to specialist interventions for chronic pain - Long Term
14 We will set up a SLWG to consider how national workforce planning solutions can help address challenges for the chronic pain workforce - Short Term
Aim D – Improved Services and Care
15 Deliver new pain management training pathways for specialist and non-specialist healthcare professionals - Medium Term
16 We will work with Public Health Scotland to improve how we capture and report national data on chronic pain - Short Term
17 We will gather data through the Scottish Health Survey to improve the planning and design of care and support for people with chronic pain - Short Term
18 We will identify shared research priorities to enhance care and services - Medium Term
Timeline
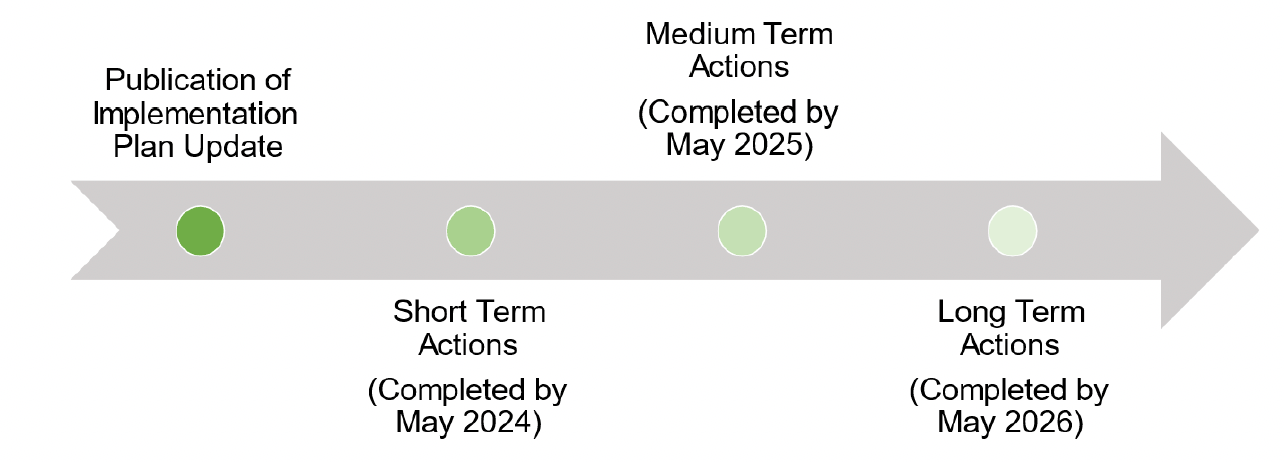
We have set out our priority Actions where people with chronic pain have told us they wish to see rapid improvement. Many of these Actions are focused on improving the infrastructure underpinning the delivery of the information, services and support accessed by people with chronic pain. Other Actions begin the task of addressing more complex issues which are likely to be realised and implemented over a longer period.
Our approach is also informed by feedback from NHS staff, service managers, Health Boards and lived experience. We are mindful of the pace of change which is realistically possible in the coming months and year ahead and feel that this is reflected in Actions which are both impactful but proportionate.
Aim A - Person Centred Care: Community-based support, quality information, compassionate care.
1. Develop chronic pain information and resources.
During the first year of the plan, we established a short-life working group to drive and oversee delivery of Aim A. This group provides a focus for evaluating existing resources at the local and national level and makes recommendations to ensure a more coordinated, national approach to chronic pain information and self-management tools and resources. This has included the improved and updated NHS inform pages driven by lived experience consultation. The group will continue their work to update the quality and consistency of information provided by Health Boards, to reduce duplication and build a collaborative, cross-sectoral approach to information provision and advice. This group will also focus on establishing a robust framework to support lived experience engagement both locally and nationally to continue to drive forward local service innovation and national policy. All of the work undertaken by the group will have a focus on considering how to reduce existing inequalities in order to ensure wider promotion and easier access to the right information, at the right time, to enhance how people with chronic pain find and engage the support and services they need.
2. Establish a Chronic Pain knowledge hub for healthcare professionals to promote understanding and learning on chronic pain.
The need to further promote awareness and understanding of chronic pain amongst the health and care workforce was identified in the creation of the Implementation Plan. To improve the consistency and quality of clinical care and advice provided to people with chronic pain, we are making it easier for healthcare professionals at all levels to access and navigate high-quality, up to date information and resources,, through a national Chronic Pain Knowledge Hub. Underpinned by the work of the National Pain Education Group we are developing a ‘one stop shop’ national resource for healthcare professionals, service managers and other delivery partners. This will be hosted on the TURAS platform, NHS Education for Scotland’s (NES) national platform which promotes health and social care professional learning and training and provides a tool that supports collection and sharing of best practice. TURAS accounts are open to anyone who works or volunteers in the public sector, including the third sector. It will also offer service planners and national networks a platform to share information which will support improved collaboration and shared planning to drive down unwarranted variation in care and service delivery.
3. Develop a pain informed care toolkit for healthcare professional to promote care in all settings.
Given that chronic pain is often experienced alongside other health conditions, and that most people will access support from local, non-specialist health and care services, we will take action to increase awareness and understanding of pain and its impact amongst staff in all healthcare settings. We will build on the success of the Scottish Government’s progress in trauma-informed care to deliver a package of measures to support a ‘Pain-Informed’ approach to the planning and development of health and care services. There is evidence to indicate that there are links between adverse experiences and the incidence and impact of pain, which similarly demand an approach to care that prioritises empathy and kindness in order for it to be effective. To inform this approach we will draw on the expertise of people with lived experience of chronic pain, healthcare professionals working in specialist and community pain services, the third sector and other key stakeholders. Together we will develop a knowledge and skills framework supported by training modules to enable staff across all sectors of health and social care develop the necessary skills to support people living with chronic pain more effectively. Delivering this Action, initially through our National Pain Education Group will lead to a better experience of health and care services, and more effective, person-centred care for people with chronic pain.
4. Enhance coordination of community and third-sector support for people with chronic pain
People with chronic pain are already experts in managing the impact of their condition on their everyday lives. However, we know that pain and its impact is often felt unequally across our society and there are many people who could benefit from additional support outwith public health and care services, to improve their quality of life. We will work with the third sector, and other community-based partners, to make it easier for people with chronic pain to access a choice of person-centred support in their local area. We will ensure alignment to other work underway to improve cross-sector working in relation to improve access to rehabilitation support and services.
To support this action, we will continue explore opportunities to develop a network-based approach to third sector engagement to act as a forum to draw on the experience of charities already providing services and support to people with chronic pain. Together, and through participation in other working groups established to deliver the Framework, this Network will focus on the opportunities and challenges of delivering local person-centred care and working at the interface with Health Boards and local authorities. This work is intended to lead to a nationally shared approach to collaboration between public and third sectors at the local level to ensure a more sustainable relationship around commissioning and coordinating community-based support for people with chronic pain as part of health and care pathways. A report on the challenges faced by the third sector and a directory of resources will be published by the network.
5. We will work with chronic pain experts to identify opportunities and develop ideas to target and raise public awareness of the condition.
In our most recent phase of stakeholder engagement, we heard from the chronic pain community a desire for more public awareness of issues related to chronic pain. Varying from increasing awareness of managing symptoms to knowing when and where to get appropriate support. We will work with people with lived experience, clinicians and third sector partners to develop a proposal for a public health campaign informed by those who know the condition best to identify where there are opportunities to reduce health inequalities and educate and inform the public through a targeted campaign.
Aim B - Accessible Care: Coordinated services, specialist support, more access options.
6. Improve co-ordination and planning of specialist pain services.
There is further opportunity to improve coordination of care for people referred to specialist chronic pain services. We will continue to support the established Service Managers Network to promote shared planning and service development across Health Boards, with a focus on opportunities to address key shared issues, including resourcing, waiting times and financial challenges.
This Network will also engage with the Short Life Working Group (SLWG) for Aim B in order to ensure there is greater synergy and coordination between primary, community and specialist services. The Network forum will continue to evolve national dialogue between local specialist services and the Scottish Government to ensure a more rapid, supportive and collaborative response to the challenges of pain management service delivery.
7. Deliver a new digital approach to improve the choice of people with chronic pain in how they engage with service.
Remote Healthcare Pathways use digital monitoring technology to enable people to receive, record and share relevant information about their current health and wellbeing with public services. In partnership with the Scottish Government’s Technology Enabled Care (TEC) Programme, people with chronic pain and local Health Boards, we piloted and evaluated a new ‘digital pathway’ at NHS Highland to enable people with chronic pain to use technology to engage with specialist pain services. This work was in line with the principles of the TEC Programme including inclusion, fairness, and choice to ensure no one is left behind in the design and delivery of new services and pathways.
The findings from the evaluation were shared at a national level and a plan made to implement the ‘digital pathway’ across all NHS Boards, to improve services and enhance the experience of people with chronic pain. Outputs from this work will continue to identify opportunities and challenges to digital delivery of care for people with chronic pain, including improved data collection and reporting, better service design and inclusive engagement of people with chronic pain in the services they use.
8. Convene a national expert working group to identify opportunities for improving pain services and their delivery.
It is accepted that demographic and geographic differences across the country inform how local services are delivered. However, a priority of this Implementation Plan is to ensure action is taken to reduce the unwarranted variation in experience and care faced by people with chronic pain. We have established a Service Managers Network to provide leadership, oversee and drive delivery of this Aim. This Network will evolve and be augmented with stakeholders who have clinical expertise of Chronic Pain alongside people with lived experience.
This group will continue to scrutinise differences in provision of local NHS and care services used by people with chronic pain to identify areas of best practice and opportunities for improvement. They will examine how the Scottish Service Model for Chronic Pain is currently being delivered across Health Boards to better understand the challenges and opportunities for service planning. They will continue to review previous work to improve the interface between community, primary and secondary care services, and identify opportunities for further tests of change and/ or scale-up of effective local pathways. This group will also make recommendations for increased collaboration across local, regional and national collaborative service planning, with the aim of improving the use of resources across clinical pathways and enhancing the sustainability of pain services and support at all levels. In addition, we will continue to work with the Centre for Sustainable Delivery to identify, develop and scale-up innovative approaches to pain management service delivery to deliver higher quality, person-centred, sustainable services. This includes delivery of projects between the primary and secondary care interface and identifying which approaches should be rolled out nationally.
9. We will work with the Scottish National Pain Management Programme and relevant stakeholders to consider the services offered to ensure the programme best meets the needs of patients across Scotland.
The Scottish National Pain Management Programme (SNPMP), hosted by NHS Greater Glasgow and Clyde, accepts referrals from all Scottish Health Boards and provides highly specialised support for people with chronic pain. We will continue to work with the National Services Division (NSD) of NHS National Service Scotland (NSS) who commission, and performance manage national specialist services on behalf of NHS Scotland, and consider how the programme is delivered, to best meet the needs of people with chronic pain across Scotland and ensure its sustainability. This will involve those working within primary and secondary care alongside, people with lived experience and other relevant stakeholders.
This work is expected to identify opportunities to evolve the service and harness its expertise and skills to enhance service delivery and promote best practice of pain management programmes and supported self-management as a core element of clinical practice. This will provide a more consistent and higher quality experience of care for people with chronic pain in a broader range of settings.
10. We will work with key stakeholders to consider the creation of National Standards for Chronic Pain Management
We have heard from people with lived experience and other key stakeholders for the requirement to have National Standards for Chronic Pain Management that span Primary and Secondary Care. It is acknowledged that there are Core Standards for Pain Management services in the UK Faculty of Pain Management Core Standards and a National Clinical Guideline SIGN 136 for the Management of Chronic Pain SIGN 168 guidelines in Scotland; National Standards will seek to draw best practice and guidance from these guidelines along with other sources of best practice.
To explore this action, we will establish a SLWG to look at the feasibility and the associated scope of creating National Standards. This SLWG will be created in conjunction with people who have lived experience, existing Chronic Pain Networks and SLWGs.
Aim C - Safe, effective support: Consistent care, safe use of medication, sustainable care.
11. Update clinical guidelines for management of chronic pain to continue to deliver evidence based care and support.
Scotland was the first country in the world to introduce national clinical guidelines to support non-specialist healthcare professionals deliver high-quality, evidence-led care for people with chronic pain (SIGN 136 – Management of chronic pain). The guidelines are based on systematic review of the scientific literature and aimed at aiding the translation of new knowledge into action. Since the SIGN 136 guideline was published in 2013 it has been reviewed once, to update content related to opioid prescribing for pain management. We have carried out initial work with the developing Pain Clinical Networks and the NHS Research Scotland Pain Steering Group to assess the requirement for a further update of the guideline. This has identified areas where there has been growth in the evidence for pain management approaches or treatment across a range of clinical fields, including physiotherapy, pharmacy and psychology. The update to SIGN has been agreed and the committee has been formed and met. At the first meeting the key questions to be addressed by the guideline were agreed and the sub-groups have been allocated. This will contribute to the continued improvement of standards of care for people with chronic pain and we will consider how to support successful dissemination and implementation of any output. In 2018 the Scottish Government Published its Quality Prescribing Strategy for Chronic Pain which will be revised in 2022. We also recognise the challenges presented by an absence of evidence, and the need to identify opportunities for ongoing collection and analysis of data, which has informed our approach to Aim D.
12. Promote safer, more effective prescribing for people with chronic pain.
While there is evidence that rates are now decreasing, prescribing for chronic pain in Scotland increased by 66% over the ten years from 2006. Many of the commonly prescribed medications included classes of medicines for which there is less evidence for their prolonged use for non-cancer chronic pain, such as opioids and gabapentinioids. There are also other risks associated with their use, including dependence.
The Scottish Government has already taken action to improve the use of medication for chronic pain through the Quality Prescribing for Chronic Pain Guide for Improvement 2018 – 2021. Additional resources have already been developed to support the implementation and use of this advice, including patient information leaflets, prescribing checklists and tools to aid healthcare professional decision making. In order to ensure we continue to promote safe and appropriate prescribing of medication as an element of pain management strategies we will update the Guide to reflect new evidence and emerging practice. This will help to ensure more appropriate consideration, prescribing and monitoring of pain medication.
13. Delivering a national approach to specialist interventions for chronic pain
Healthcare professionals may consider specialist intervention, including injections, are offered for some patients with chronic pain, depending on individual circumstances and diagnosis. From our engagement with clinicians and people with chronic pain, it is clear there continues to be significant variation not only in provision of these treatments across Scotland. There is also debate on the factors contributing to this issue, and potential solutions, including workforce and staffing challenges, patient expectations and outcomes, and differences in clinical opinion on the efficacy of certain treatments.
This is a complex challenge and we are committed to working towards a more consistent, national approach to provision of specialist interventions for people with chronic pain. In this Action we will continue to build on previous and ongoing service improvement activity and expert guidance such as that from the Faculty of Pain Medicine. We will also seek to involve and consult the expertise of the new Pain Medic Network, other clinical areas and the views of people with chronic pain to drive progress on this issue. This will include assessing existing local provision and access pathways for specialist interventions, reviewing the evidence and requirement for guidance to inform and improve clinical practice and decision making and the potential for more standardised treatment outcome measures and assessment. This Action will also help to guide deliberation of opportunities for increased regional (e.g., mutual aid) and national pathways to improve the coordination and sustainability of services, as well as improving timely access to effective support for people with chronic pain. We have requested that Scottish Health Technologies, part of HIS, review the evidence base for specialist interventions. Any recommendations received from the group will be used to improve the quality and equity of services across Scotland.
14. We will set up a SLWG to consider how national workforce planning solutions can help address challenges for the chronic pain workforce.
Stakeholder engagement has shown the need to build a sustainable chronic pain workforce fit for the future. We will continue to align with the vision of The Health and Social Care: National Workforce Strategy which sets out a series of commitments to recover, grow and transform the workforce, including shaping future training programmes to support the development of the pain management workforce. We will consider how national workforce planning solutions can help address capacity challenges for the chronic pain workforce. Working with stakeholders, we will also examine how workforce planning can improve delivery throughout and quality of services for people with chronic pain.
We will undertake work to create a baseline of the current chronic pain workforce and understand future pain workforce needs and opportunities to support implementation. This will help to ensure greater coordination and alignment of workforce actions to ensure they maximise benefit for people with chronic pain and those working in our health and social care services.
Aim D - Improved services are care: Skilled healthcare, data-driven care, innovative care.
15. Deliver new pain management training pathways for specialist and non-specialist healthcare professionals.
Rapid developments in medicine, including evolving technologies, treatments and care models require the healthcare workforce to have the right skills and qualifications to deliver these advancements and meet the future needs of patients. We will continue to support the delivery of new training pathways for chronic pain which recognise the prevalence of the condition, and to reflect the modern multidisciplinary nature of pain medicine.
The Scottish Government is working with the Faculty of Pain Medicine (FPM) and NHS Education for Scotland (NES) to support the development of new credentials for Pain Medicine Specialists. Credentials are discrete modules of learning, regulated by the General Medical Council or NES, which can be accessed flexibly by trained doctors at any stage in their career (e.g., after they have specialised in a particular field) and are based on patient and service need. The Pain Medicine Specialist credential intends to expand the knowledge and skills of a wider cohort of expert clinicians across anaesthetics, rheumatology, neurology, rehabilitation medicine and palliative care. The credential will be available both before and after completion of specialist training (pre-/ post-CCT) and for existing speciality grade clinicians.
Work is also underway to develop and implement a Credential for Advanced Care Practitioners in pain management for those working out with specialist services, including GPs, paramedics, psychology, AHPs and other related roles. These new training and development programmes will ensure a more holistic approach to pain medicine from a larger cohort of practitioners, increasing the quality of care available for people with chronic pain within and across a range of care pathways.
16. We will work with Public Health Scotland to improve how we capture and report national data on chronic pain.
Chronic pain waiting times for specialist services are reported on a quarterly basis by Public Health Scotland (PHS). PHS has taken steps to increase the quality and transparency of the data available, with the waiting times report enhanced to provide a greater level of detail and a more complete picture of waiting times.
We have been working with PHS and NHS service and clinical leads to review this work to ensure there is appropriate oversight of pain service performance as models of care continue to evolve. This has included evaluating the existing data collection and identifying opportunities to implement improvements in reporting to more appropriately and fully reflect the pathways patients now follow as they access chronic pain services. (See Annex A (3) for more detail).
17. We will gather data through the Scottish Health Survey to improve the planning and design of care and support for people with chronic pain.
Improved data collection on chronic pain at the population level supports a better understanding of the prevalence of the condition and its impact on wider society. For the first time, in December 2023, questions on chronic pain will be in in the Scottish Health Survey which will help to provide a more detailed picture of the health of people with chronic pain and the other factors which impact on their quality of life and wellbeing such as other health conditions, physical activity and deprivation.
We will support dissemination of outputs from the survey data and will identify opportunities through delivery of the Implementation Plan to encourage improved decision making at the local, Health Board and national level. This includes understanding the barriers and opportunities for the use of local-level chronic pain data to guide how Health and Social Care Partnerships (HSCPs) and Integration Authorities (IAs) consider and address the needs of their local populations. We will also identify opportunities for the data to inform other health policies and cross-Government actions to ensure they take into account the needs of people with chronic pain. This Action will increase the profile of the broader spectrum of challenges experienced by people living with chronic pain in Scotland, and promote the design and delivery of more person-centred, effective care and services.
18. We will identify shared research priorities to enhance care and services.
Research on chronic pain has continued to improve standards of care and ensure an evidence-based approach to service design. In Scotland we benefit from a vibrant pain research community driven by the NHS Research Scotland Pain Network (NRS Pain). We will work with this network, and people with chronic pain to identify shared research priorities including those suggested from consultation on the Framework, to improve treatment, management, quality of life and wellbeing for patients.
Contact
Email: chronicpain@gov.scot
There is a problem
Thanks for your feedback