Summary Report of the National Review Primary Care Out of Hours Services
A Summary Report of the independent Review of Primary Care Out of Hours Services Chaired by Prof Sir Lewis Ritchie. The Main Report, which accompanies this summary version, provides a more comprehensive overview of the Review, its methodology, findings and rationale for the recommendations proposed.
1 Key Messages
Purpose: This Section provides key messages about Primary Care Out of Hours Services and answers questions about what future services might look like and how that might happen. It differs from the Key Messages section in the Full Report - in order to improve accessibility
Person-Centred Care
- Putting the person at the centre of care is a fundamental principle of the Scottish Government's future vision for the people of Scotland. In this Review, the 'person' refers both to those who need services - their carers and families - and those who provide services. We need to both deliver excellent care in partnership with patients and we need to value the staff who provide it.
- Urgent care services for problems and care needs that cannot wait for a routine appointment should be more easily accessible and navigable for all but need to be valued and used responsibly.
Service Demand and Sustainability
- During the one year period 1 May 2014 to 30 April 2015, almost 1 million contacts were made with primary care OOH services.
- The demand for urgent care is growing - particularly for rapidly increasing numbers of frail older people with multiple long-term conditions and complex care needs.
- The present situation for OOH services is fragile, not sustainable and will worsen, unless immediate and robust measures are taken to promote the recruitment and retention of sufficient numbers of GPs and other multidisciplinary team members working in both daytime and OOH services.
What will the future look like?
- Future service design and delivery should be based on best meeting the needs of the public and those who deliver services. This should enable tailored advice, support and self care, and where required, direction to the right service, at the right time.
- Patients can no longer expect always to see or receive telephone advice from GPs for urgent care. Future care will be delivered by well trained and well-led multidisciplinary teams. Patients will be seen by the right clinical or caring professional according to need. That could be a GP, an advanced nurse practitioner, a community nurse, a paramedical practitioner, a pharmacist, an allied health professional (AHP) such as a physiotherapist, social services or other team member who might work for the third or independent sector or another agency. GPs must continue to be an essential part of multidisciplinary urgent care teams, providing clinical leadership and expertise.
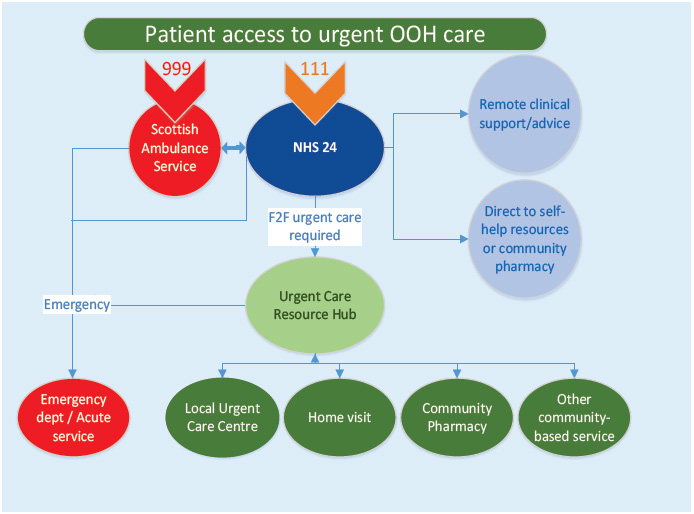
Figure 1 - A new model of out of hours care
How will that be organised?
- At the moment care can be fragmentary and communications can be difficult between professionals to the detriment of best patient care. A new model of urgent care is proposed by developing Urgent Care Resource Hubs - see Figure 1 above. These hubs would provide a coordinating area and locality wide function for multidisciplinary urgent care and should provide remote telephone or video-link support for care professionals from all care sectors. While primarily established for OOH services, they should be considered for 24/7 urgent care coordination. They will need to be piloted and tested to inform future progress.
- An area Urgent Care Resource Hub would normally be networked to several local Urgent Care Centres.
- Local Urgent Care Centres (which are presently known as Primary Care Emergency Centres) should be located to facilitate patient access for care, but also for service resilience. They should be fit for purpose for service delivery and training.
How will out of hours care be accessed?
- In the case of genuine medical emergency care that will continue to be by 999 phone call, to access the Scottish Ambulance Service (SAS), or by direct attendance at A&E services.
- In the case of urgent care for a medical problem - care that cannot wait for a routine appointment, when GP practices are closed, by dialling 111 to access NHS 24, as now. NHS 24 will provide the right advice for self care or direction to the right care service - routed to the area Urgent Care Resource Hub nearest to the patient's location. This Hub will coordinate best care by requesting the patient or carer to visit a local Urgent Care Centre or, if required, by arranging a house call or by direction to another community care service. A house call might be done by an advanced nurse practitioner, by a GP, or parmedical practitioner (paramedic). Some callers will be directed to attend Accident & Emergency services and a small number will have a 999 ambulance dispatched for their immediate assistance.
What will be different?
- NHS 24 and SAS already work closely together, but we have asked them to look again at their care pathways to ensure better coordination of care. This should provide better experience and outcomes for patients and their carers.
- We would expect the public to make greater and better use of local community pharmacies in the future to seek advice and treatment for minor ailments both during daytime and OOH. There is insufficient awareness of the services delivered by community pharmacists and that should change.
- We have looked at a small number of groups of patients with specific needs - children, palliative care patients, frail older people, people with mental health conditions and those who are living in deprived circumstances or who have problems accessing services for a number of reasons. We would expect their care to be improved with better access to services according to need. The work is preliminary only - we suggest that there is much more to do. We identify further work that needs to be considered for prisoner care and for forensic clinical services.
- Increasing use will be made of telehealth and telecare, with remote video-consultations increasing. We have advised that mobile applications 'apps' should be developed and evaluated in order to support self care and best use of services.
- We would expect the third sector, already a large and important provider of care - particularly for vulnerable people - to be playing a greater role in future services in collaboration with all other sectors.
- For the care home sector we would expect better remote professional support and improved recording systems.
- We indicate that greater use could be made of the Scottish Fire and Rescue Service, for prevention and care in the community, if available. They are already working closely with SAS to assist cardiac arrest victims as their vehicles carry defibrillators. We have suggested consideration of further expansion of their first-responder role to help clinical care, in the absence of timely ambulance availability.
- In some remote island communities the RNLI lifeboat service may be deployed to evacuate urgent cases when other transport may not be available or unsuitable, particularly in adverse weather conditions. We have asked for a Memorandum of Understanding to be drawn up between RNLI, SAS and HM Coastguard.
- We would expect the specific needs of remote and rural communities to be taken into account particularly for transport and communication issues. Greater use of remote video consultations may help matters.
How can the public and patients helped to make better access and use of services?
- We have made recommendations about promoting better understanding and use of services. We wish to raise the profile of the meaning of 'urgent' and 'emergency' to promote responsible use of services. We advise that best practice should be used to achieve that including learning experience, taking into account international best practice.
- We have particularly looked at how to bolster self care and have recommended promoting person-centred care through better self-management and health literacy.
- We call for greater public involvement in health service developments - those who receive services are entitled to shape them.
What about those who provide the services?
- We have indicated that staff providing services need to be valued more, which is why we say person-centred should refer to both those who receive care and those who deliver it.
- We have made a large number of recommendations about workforce issues and have examined the future roles of GPs, advanced nurse practitioners, district nurses, pharmacists, paramedics, AHPs, physician associates and social care practitioners.
- We have called for urgent primary care workforce planning to be developed at national and local levels - this must be done without delay to rapidly enlarge and enhance capacity.
- We have asked for new one year posts to be created for GPs after completion of three year training and for four year training to be better configured for urgent GP care. We want young GPs to be supported and GPs at all career stages to be encouraged and enabled to work in OOH services.
- We commend the Chief Nursing Officer's Reviews of Advanced Nurse Practitioners (ANPs), creating sufficient capacity and uniform standards and also her District Nursing Review - many district nurses will be retiring shortly so this a pressing matter.
- We have already indicated that community pharmacies should play a greater role for urgent care. Clinical pharmacists will contribute more to both daytime and OOH services. Like ANPs we would expect many more pharmacists to be independent prescribers.
- Paramedical practitioners (paramedics) will play greater roles in delivering care to the community - they are already doing it and like NHS 24 have recently supported some GP practices with staffing difficulties, in daytime hours. Ambulances could be regarded in the future as mobile Urgent Care Centres - that may be more important for remote and rural areas.
- AHPs too will have more prominent roles in OOH services, primarily supporting community rehabilitation and fall pathways, which we have recommended should be accelerated and more uniform throughout Scotland.
- Physician Associates (PAs) have been working in the USA for many years and play important roles working with and for doctors. They should be considered for augmenting the Scottish primary care workforce.
- The roles of social services workers continues to grow - the importance of working closely with clinical colleagues should be fostered by the new model we propose. Again awareness of their roles could be improved as they contribute much to the care of society in the OOH period - including the community alarm system and assistance and preventing falls.
- We also indicate how critical OOH support workers are - they should be appreciated and valued.
How will this happen?
- We have made a number of recommendations about improving quality and safety.
- We have asked for a service specification for OOH services to be developed.
- We would like to support services to promote quality improvement and have asked how that can best be achieved.
- We have made a number of recommendations about securing best use of electronic records and consistent data sharing.
- We have yet to truly unleash the potential of information technology for better and safer patient care and we must strive to achieve that.
- We have called for rapid development of comprehensive primary care workforce plans at national and local levels
- We have suggested that undergraduate schools for health and social care professionals should look at the balance and emphasis of their training - as the changing needs of society and workforce capacity/capability, should be closely aligned
Who will support and ensure these recommendations happen?
- We have spoken to and made recommendations about the third sector, the independent sector, Special Health Boards, Health Bodies and other agencies.
- Throughout the Review we heard about the future importance of Health and Social Care Partnerships and Integrated Joint Boards - that is reflected in our recommendations.
- We commissioned academic research to inform our deliberations and uncovered a lack of good evidence and evaluation of OOH Services We offer some priority areas for future research and have recommended that new models of care, such as proposed by the Review are properly piloted and rigorously evaluated.
- We are conscious of how ambitious some of our recommendations are and also their limitations - while some may be delivered in the short term others will take much longer.
- We would expect these recommendations to be considered carefully but also critically - the canvas is wide, but we need to prioritise and in some cases discard for good or unforeseen reasons.
- We have suggested guiding principles for new services should be:
- Person-centred - for those who receive and those who deliver services
- Intelligence-led - making the most of what we know about our people and their needs
- Asset-optimised - making the most of all available assets and resources
- Outcomes-focused - making the best decisions for safe and high quality patient care and wellbeing
In addition to these guiding principles, such services should be: - Desirable - high quality, safe and effective
- Sustainable - resilient on a continuous basis
- Equitable -fair and accessible to all
- Affordable - making best use of public funds
- We have recommended robust planning to be developed at national and local levels to do determine what are likely to be quick wins and what are not. We thought about prioritising our recommendations, but felt that more detailed deliberations would be required, which would fall outwith our allotted timescale for conducting the Review. The recommendations need wider scrutiny and that is our intention, taking into account stringent resource constraints. However, because of current difficulties and serious challenges ahead, we cannot tarry and need to press on with resolve.
- We need to ensure best use of resources and have offered some proposals regarding financial planning for some of the strategic developments recommended.

Nursing staff, part of a multidisciplinary team at NHS 24, Norseman House
Contact
Email: Diane Campion
There is a problem
Thanks for your feedback