Review Body on Doctors' and Dentists' Remuneration 2023 to 2024: Scottish evidence
Written evidence submitted to the Review Body on Doctors’ and Dentists’ Remuneration (DDRB) by the Scottish Government for the 2023 to 2024 pay round.
H. Specific Staff Groups - Pay, Terms and Conditions
1. General Medical Practitioner Contractors (GMPs)
Introduction
242. This section provides information relating to general practice (independent contractor GMPs) and the delivery of contracted services through the NHS Boards. This section provides additional background to developments with the GMS arrangements in Scotland, and the implementation of the new contract in 2018.
Background
243. The majority of GMPs working to provide primary medical services in Scotland are independent contractors, self-employed or partnerships running their own GP practices.
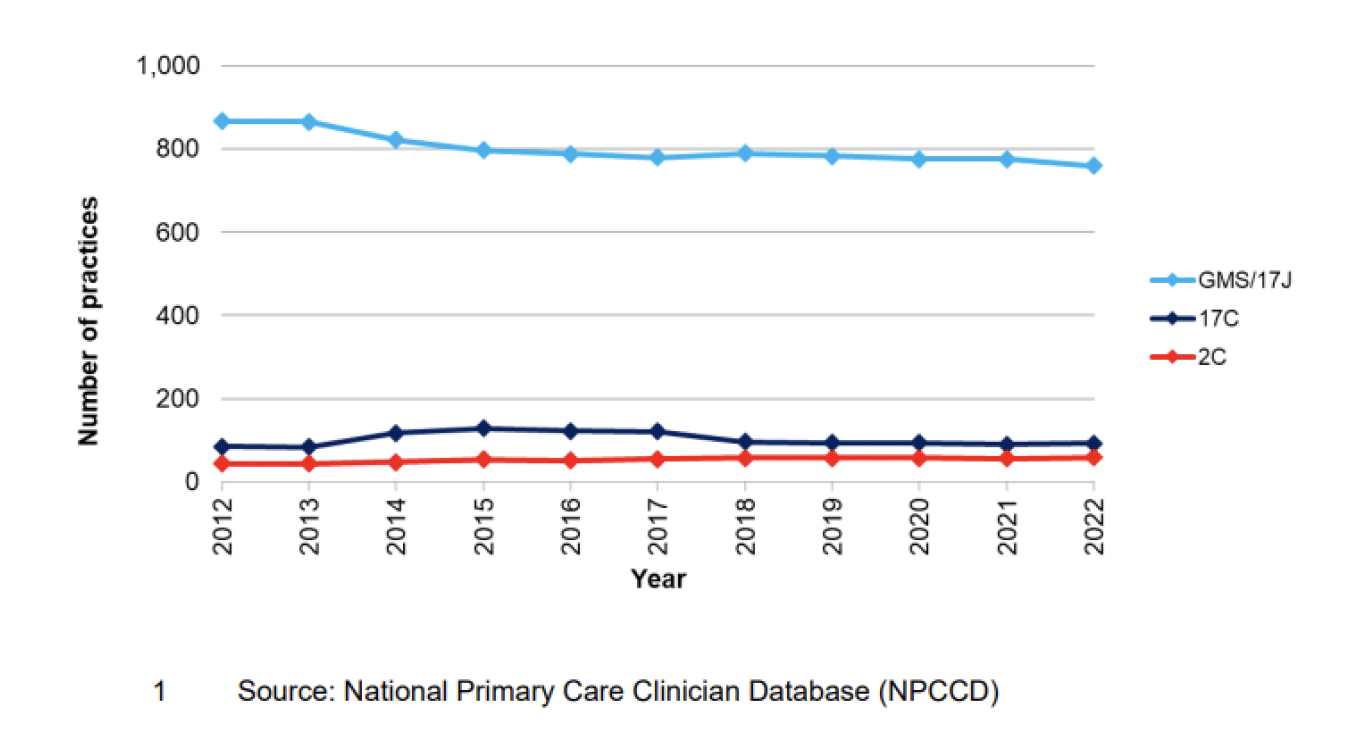
244. The General Practice – GP workforce and practice list sizes was published on 13 December 2022. As of 1 October 2022, there were 911 GP practices[23] in Scotland and 83% were on the national General Medical Services contract. The number of practices in Scotland has decreased by 9% from 997 practices in 2012, reflecting a trend towards larger practices with more GPs serving a larger number of patients. GMPs operating under Section 17C or 2C arrangements provide services based on locally agreed contracts, and any uplift in investment for these arrangements is a local matter for the Health Board.
245. As of 1 October 2022:
- 759 practices operated under the General Medical Services Contract;
- 93 practices operated under the 17C contract; and
- 59 practices operated under the 2C contract[24].
246. The headcount of GPs in Scotland is 5209. This is a slight rise of 32 GPs compared to 2021. Prior to 2018, the headcount of GPs had remained roughly constant at around 4,900 since 2012[25].
247. As of 30 September 2022, 1956 (38%) of the GP workforce were male and 3217 (62%) female[26].
248. The average (or mean) size of a Scottish GP practice in terms of numbers of registered patients was 6470 in 2021[27], however there was considerable variation, ranging from under 200 patients for practices in remote locations or practices which addressed specific health needs of patients (e.g. those with challenging behaviours or homelessness), to practices of over 20,000 patients in densely populated urban areas.
2018 GMS Contract
249. The 2018 Contract came into effect on 1st April 2018. It was agreed through a process of collaborative negotiations between the Scottish Government and the SGPC.
250. The contract includes:
- Improving access for patients;
- Addressing health inequalities and improving population health, including mental health;
- Providing financial stability for GPs;
- Reducing GP workload through the expansion of the primary care multidisciplinary team;
- Increasing support for GPs and GP infrastructure;
- Increasing transparency on general practice funding, activities and workforce to assist strategic planning, commissioning and delivery of primary care services; and
- Making general practice a more attractive profession for existing GPs, junior doctors and undergraduate medical students.
251. One of the core aspects of the new Contract is the new funding model as the Scottish Government recognises that an appropriate and secure level of income is a prerequisite to attracting GPs to the profession and ensuring the future sustainability of general practice.
252. The new contract will be introduced in two phases. Phase One included:
- A new workload formula to better match resource to demand;
- Additional investment of £23 million to allow most practices to gain from the new funding formula, whilst the remaining practices have received an income guarantee to protect their income level to ensure no practice was destabilised; and
- From April 2021, a GP Partner whole-time-equivalent minimum earnings expectation. This means that no GP will receive less than £89,784 NHS income per year (including pension contributions) for a whole-time post. This is due to be uplifted in line with DDRB recommendations.
253. These initial changes will be followed by Phase 2 dependent on a further vote from the profession. Phase 2 will include:
- Introducing an income range for GP Partners that is comparable to consultants; and
- Directly reimbursing practice expenses.
254. These proposals are based on evidence from the 2017 Review of GP Earnings and Expenses[28].
Pay and Contractual Uplift 2022/23
255. For 2022/23 the Scottish Government implemented the DDRB recommendation to uplift GP pay net of expenses by 4.5%[29]. In total the Scottish Government uplifted the GP contract by £44.2 million. This also included a 5% uplift to practice staff expenses, and a 4.5% uplift to wider practice expenses. This also included £6.8 million funding to cover population growth in 2020/21.
256. The contractual uplift was applied consistently across all general practices.
Investment in General Practice
257. Investment figures for 2018/19 were published on 19 September 2019[30]. They show that for the period 2018/19 the total spend on General Practice (including the reimbursement of drugs dispensed) was £992.5 million in Scotland, an increase of 6.53% from 2017/18. Total spend on General Practice 2018/19 (excluding the reimbursement of drugs dispensed) was £967.5 million in Scotland, an increase of 6.81% from 2017/18. From 2020, this series of publication has been discontinued.
Agreement to Publish GP Earnings
258. Following an agreement between Scottish Government and SGPC NHS payments to practices have been published since May 2015 beginning with the publication of 2013/14 data.
259. In 2020/21 the sum of NHS Scotland non-dispensing payments made to 928 General Practices was £950.5 million[31]. Investment had increased by £55.8 million (6.2%) when compared to 2019/20 .
- £800.9 million was paid to General Medical Services (GMS) contracted practices run by GPs[32];
- £111.5 million was paid to locally negotiated contracted practices (17C) run by GPs[33]; and
- £38 million was paid to NHS Board run practices (2C)[34].
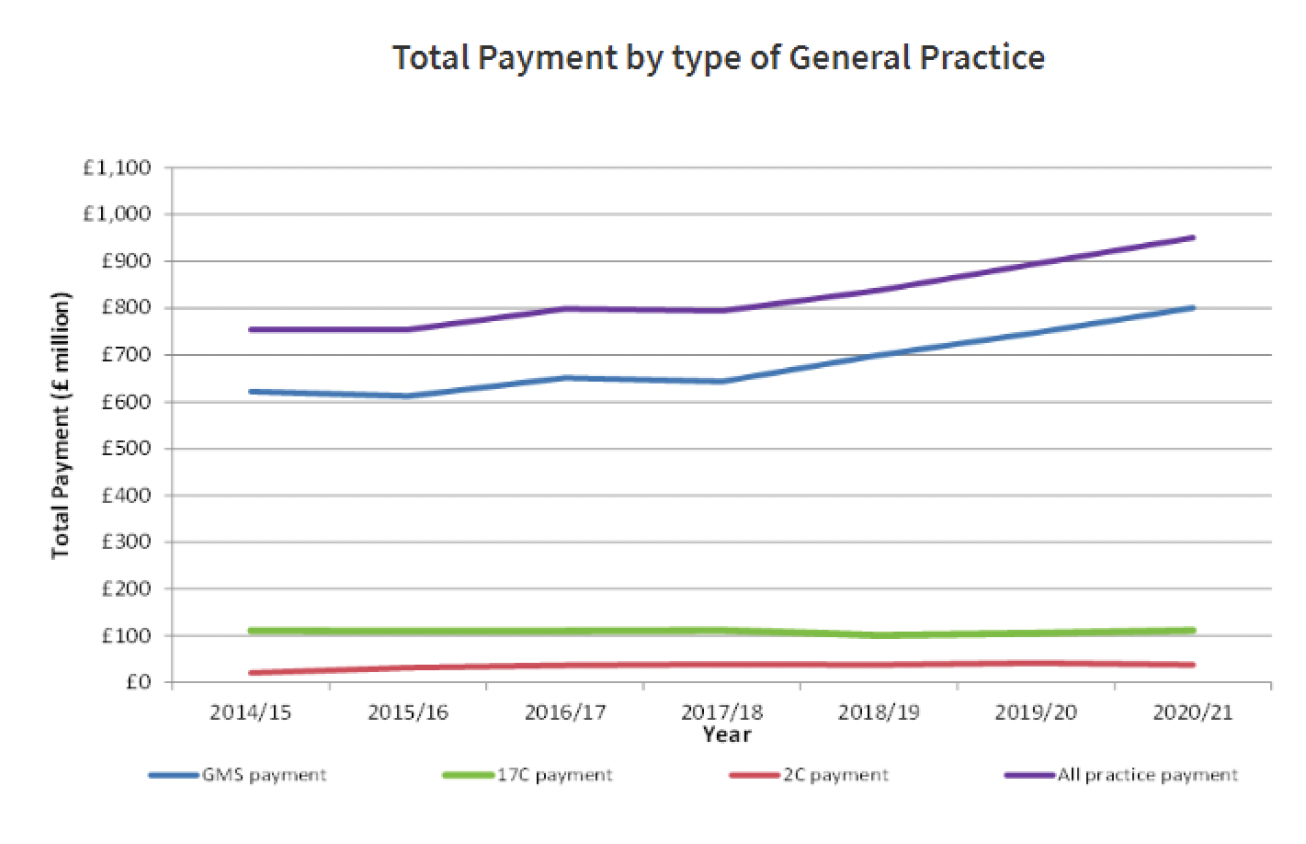
Types of General Practices and their Total Payment[35]
260. Of the £950.5 million paid in 2020/21: The Global Sum was the largest payment amounting to £643.8 million to 928 General Practices[36].
261. In addition to the £950.5 million, £21.9 million was paid to 88 General Practices for dispensing services in 2020/21, a decrease of £1.0 million, paid to 89 General Practices for these services in 2019/20[37].
262. The new contract means an increase of data collection. This will include requiring all practices to provide data on earnings, expenses, hours and sessions. This data will be held confidentially and processed by NHS National Services Scotland Practitioner Services. Only anonymised, non-identifiable data will be provided to the government and NHS Boards for the purpose of analysis.
Patient Experience
263. The Scottish Health and Social Care Experience survey is carried out every two years, the 2021/22 survey was published in May 2022[38],
264. Over 130,000 individuals registered with a GP practice in Scotland responded to the 2021/22 Health and Care Experience Survey. The survey asked respondents to feed back their experiences of their GP practices and other local healthcare services: receiving care, support and help with everyday living; and caring responsibilities.
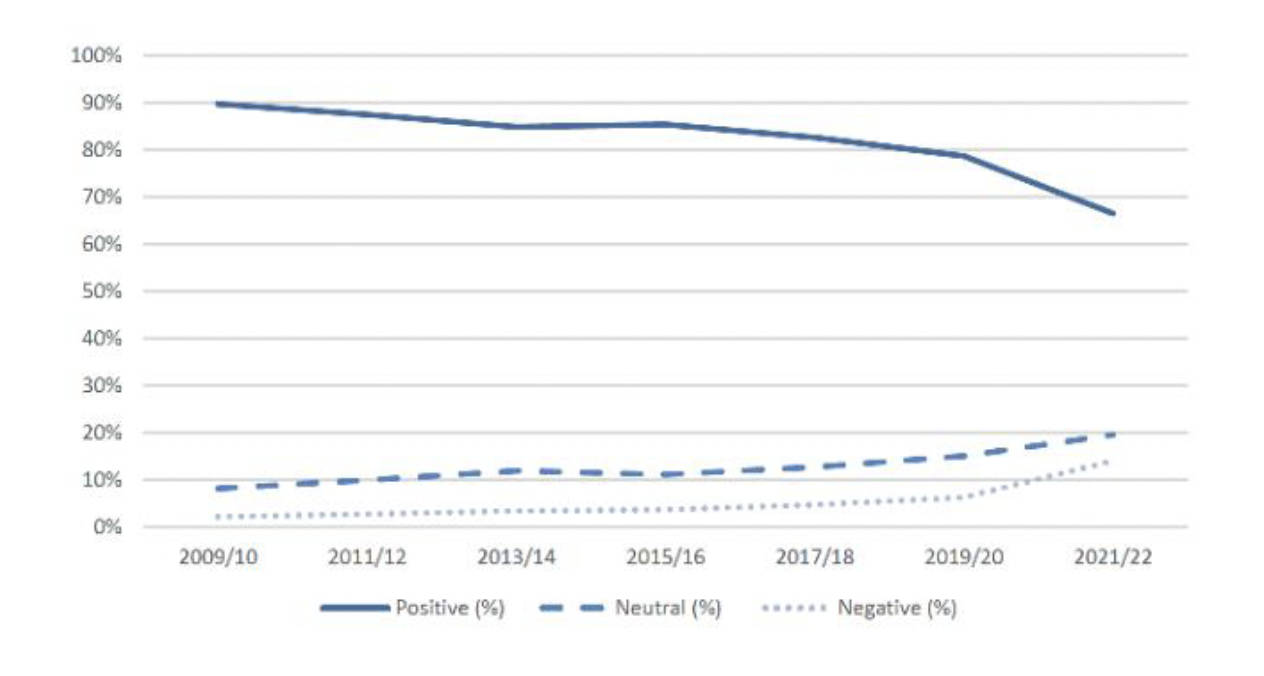
265. 67% of people rated the overall care provided by their GP practice positively, this was down twelve percentage points from the last survey.
266. 75% of people found it easy to contact their GP practice in the way that they want to.
267. 61% rated the arrangements to see a doctor positively compared with 71% seeing a nurse.
268. Of those who had needed to see or speak to a doctor / nurse, 85% were able to do so within two working days. This is similar to 2019/20 (86%).
269. Respondents were asked whether the appointment they got was face to face at the GP practice or via phone or video call or a home visit. The majority (57%) of respondents had a telephone appointment (11% in 2019/20), with just 37% of respondents having a face-to-face appointment (87% in 2019/20). The number receiving home visits or video calls remained low (1% and 2% respectively). Similarly, only 2% of people reported having an email or instant message consultation.
Overall rating of care and treatment provided by GP practice (%)[39]
270. The number of GP consultations estimated to have taken place in Scotland in 2012-13 was 16.2 million[40]. This figure is likely to have risen in subsequent years.
Access
271. Three quarters of respondents (75%) found it easy to contact the GP practice in the way that they want compared to 85% in the 2019/20 survey. Conversely, the proportion of people who found it not easy to contact their GP Practice in the way that they want increased from 15% to 25%,
272. In previous surveys, respondents were asked how easy they found it to get through to their GP practice on the phone specifically and this was also rated very positively, with 82% of people saying they found it easy in both 2015/16 and 2013/14.
273. The survey asked respondents when they had last contacted the GP practice named on the survey letter. Fewer respondents (77%) had contacted the named GP practice in the last twelve months than in 2019/20 (86%).
274. For those who had contacted their GP practice in the last twelve months, fewer patients contacted their GP practice on multiple occasions compared to previous years, with an increase in the percentage of patients contacting their practice on only one occasion, from 17% in 2019/20 to 22% in 2021/20.
275. A review of patient access to GP services across the country in partnership with the British Medical Association (BMA) was included in the GP contract agreement for 2014/15, in order to support practices and NHS Boards to both better understand the challenges and to make any necessary improvements to access. This focus has been maintained in the new contract, which is underpinned by the principle of ensuring patients can see the right person at the right place at the right time.
276. In Scotland we are transforming primary care, including the development of multidisciplinary teams, supported by extra investment through the Primary Care Fund. This will put in place long-term, sustainable change within GP services that can better meet changing needs and demands, to ensure that patients can access the right person at the right time.
277. The Primary Care Fund is also supporting and accelerating the use of digital services by GP practices, such as by funding the development of web GP and online appointment booking to improve patient access.
278. The General Practice Access Group will work to understand the challenges and issues accessing appointments with GPs. It will work to establish principles to support patients' accessing the right care at the right time. The group will establish high level core principles to support and enhance patients' experience of accessing 'The Right Care, Right Time, Right Place'.
Care and Treatment
279. When asked to rate the care provided by their GP practice overall, 67% of people rated it positively. This is a decrease of twelve percentage points compared to the previous survey and a decrease of twenty three percentage points compared to the first Health & Care Experience Survey in 2009/10.
280. The most positively rated statements were 'I understood the information I was given' and 'I was able to ask questions if I wanted to' (91% and 87% positive).
281. The statement with the lowest positive rating was 'I knew the healthcare professional well', with less than a third of people (32%) rating it positively. This statement also has a significantly higher negative rating (41%) than the other statements. However, those who had contacted their GP practice more frequently in the last 12 months were more likely to respond positively to this statement.
Vacancy, Turnover and Attrition Rates
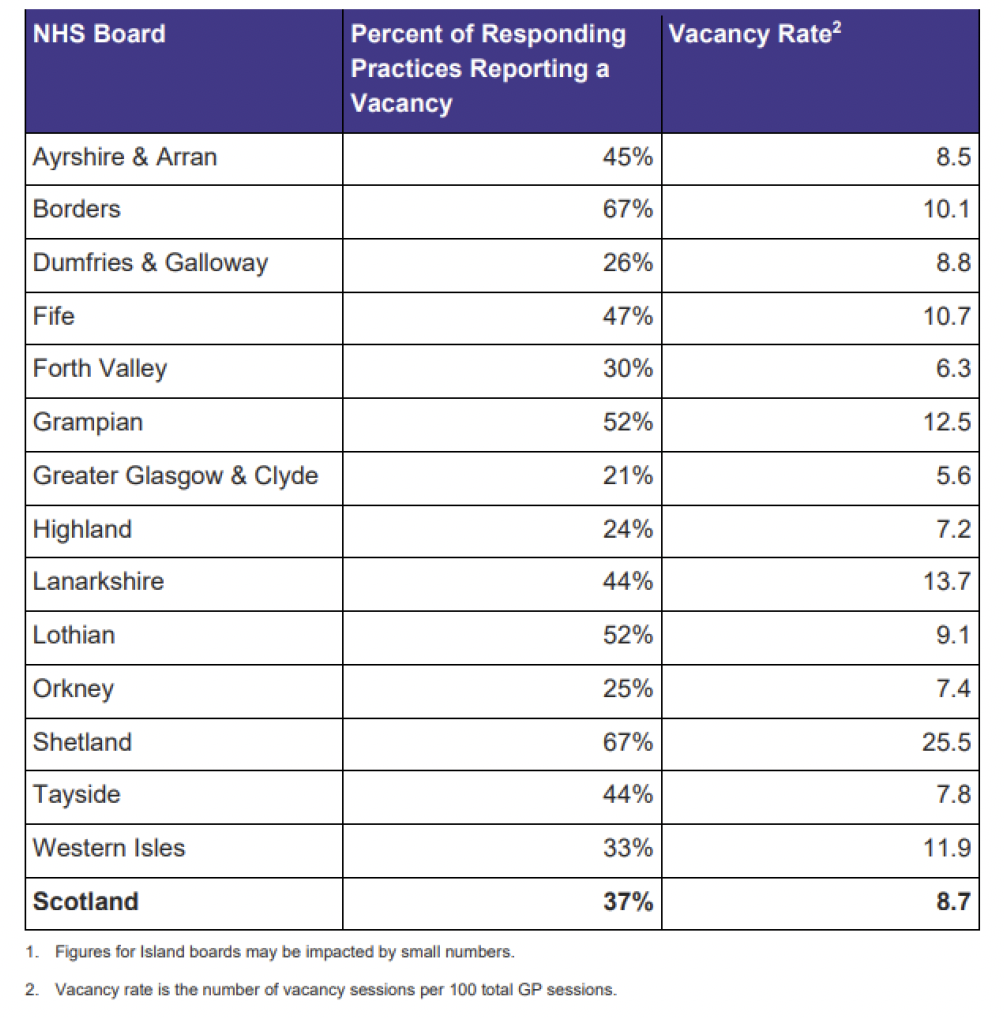
282. According to the Primary Care Workforce Survey Scotland 2022[41] workforce survey, 37% of GP Practices reported that they had vacant GP sessions from 1 April 2021 to 31 March 2022, in comparison with 32% of practices in 2019[42]. The overall vacancy rate was 8.7 vacant GP sessions for every 100 total GP sessions. The vacancy rate varied by NHS Board. Discounting the Island Boards rates which are subject to volatility due to small numbers, the vacancy rate ranged from 5.6 vacancy sessions per 100 GP sessions in Greater Glasgow and Clyde, to 113.7 vacancy sessions per 100 GP session in Lanarkshire.
Vacant GP Sessions(1) and Vacancy Rates(1)(2), by NHS Board; 1 April 2021 to 31 March 2022.
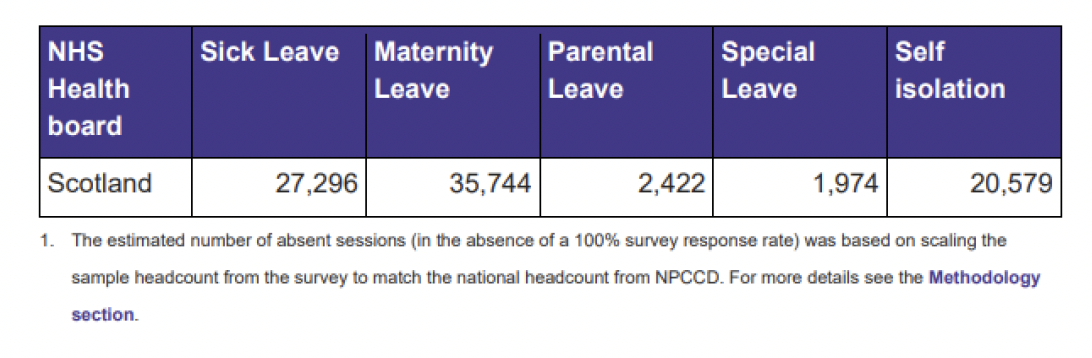
Number of estimated(1) absent GP sessions, by reason for absence; 1 April 2021 to 31 March 2022.
Recruitment and Retention
283. Between 2008 and 2017 the headcount of GPs remained roughly constant at around 4900. In 2017, Scottish Government committed to increasing numbers by at least 800 over the next ten years.
284. In 2022, we remain committed to that target with the number of GPs increasing by 106 over the last two years, to a total of 5209, as at 1 October 2022, which was a record number of GPs working in Scotland
285. As we strive to meet our 2027 recruitment challenge we recognise it will require concerted and sustainable effort over the medium term to achieve significantly improved fill rates. This includes taking forward a number of initiatives to make general practice a more exciting and attractive specialism. This includes:
- Continuing to offer the £20,000 bursaries for GPST posts in "hard to fill areas" in the further 2020 recruitment round.
- Expanding training opportunities within Primary and Community-based practices.
- Enhancing roles of GPs via Fellowships.
- Reviewing the trainee selection criteria to ensure it is fit for purpose.
- Enhancing the GP Returners Programme to encourage those who have left the profession to return.
- Increasing exposure to primary care at undergraduate level
286. The high level of trainee recruitment has been maintained in 2022 with 98% of GP training posts filled and we continue to develop our strategy for both recruitment and retention of our workforce.
287. The NHS Recovery Plan highlights that the recovery of staff is intrinsic to our collective ambitions for renewing our NHS and highlights the £8 million of investment this financial year in measures to support the physical, mental and emotional needs of the workforce, including:
- the National Wellbeing Hub and National Wellbeing Helpline;
- investment of £2 million in targeted support to the primary care and social care workforces;
- the Workforce Specialist Service, which is a confidential multidisciplinary mental health service with expertise in treating regulated health and social services professionals;
- Specific GP Coaching for GPs thinking of leaving the profession
- additional funding to NHS Education for Scotland (NES) for the provision of psychological interventions and therapies to the Health and Social Care workforce;
- guidance to promote effective wellbeing conversations;
- enhancing occupational health provision;
- improving access to quality assured peer support and reflective practice; and
- the launch of a new National Wellbeing Programme with workstreams covering specific areas of work including ICU, nursing, primary care and social care.
288. Seniority Payments for Scottish GPs are set out in chapter 10 of the annual Statement of Financial Entitlements (SFE)[43]. Seniority Payments reward experience, based on years of reckonable service adjusted for superannuable income factors. Seniority Payments are made to the practice for payment to individual GPs.
289. Presently a GP has to work for six years before any seniority payment is made; for 6 years to achieve a payment of £600 per annum, for 21 years to achieve a payment of £5,129 per annum, for 36 years to achieve £10,258 per annum, with the maximum of £13,900 per annum payable being made at the 47 year point[44]. The contractor has to have been in an eligible post for more than 2 years in order to be able to apply.
290. The Scottish Government's annual bill for seniority payments to GPs was £16.9 million in 2020/21[45]. This is a decrease on the £17.3 million in the previous year 2019/20[46].
291. 'Golden Hellos' for Scottish GPs are set out in chapter 11 of the annual Statement of Financial Entitlements (SFE). Golden Hellos are a lump sum payment to doctors who are starting out as GP performers in their first eligible post. Posts are considered to be eligible if they are attracting payments for remoteness, rurality or deprivation. Golden Hellos can also be paid to new GP performers if the local Health Board believes the practice is experiencing significant difficulties around recruitment and retention. These are just for GPs in GMS practices with the exception of Golden Hellos for remoteness and rurality which are for all practices regardless of contractual status.
Table setting out the rate of Golden Hello payments
| Reason | Payment |
|---|---|
| Recruitment Difficulty | £5,000 (minimum) |
| Remoteness or Rurality | £10,000 |
| Deprivation | £7,500 - £12,500 |
292. The rate of payment for part time GPs, with a time commitment fraction of less than 4 sessions per week is 60% of the full payment.
Salaried GPs
293. The Primary Care Workforce Survey Scotland 2022 estimated that 72% of GPs were Independent Contractors[47]. It estimated that there were around 1221 salaried GPs (27%) and 61 GP retainees (1%). .
294. The survey also found that Performer GPs, who had an average of 0.82 WTE per GP. Performer Salaried (0.67 WTE per GP) and Performer Retainer (0.44 WTE per GP) were more likely to work part time.
295. The document sets out a breakdown of the GP workforce by gender, however we do not have current data to indicate whether these GPs were independent contractor or salaried GPs.
GP Expenses
296. Data on GP income and expenses data is provided annually by NHS Digital on behalf of the four countries[48], and which, for the tax year 2020/21, was published on 1 September 2022. We invite DDRB to consider this report in its entirety, but for the purposes of independent contractor GPs in Scotland the report showed that:
297. The average taxable income for contractor GPs in General Medical Services in the UK was £142,000 in 2020/21. In Scotland the average taxable income for contractor GPs was £115,400.
| Contract Type | Year | Report Population | Gross Earnings | Total Expenses | Income Before Tax | Expenses to Earnings Ratio |
|---|---|---|---|---|---|---|
| GPMS | 2019/20 | 3,300 | £241,100 | £135,000 | £106,100 | 56.0% |
| 2020/21 | 3,250 | £255,600 | £140,200 | £115,400 | 54.9% | |
| Change | -50 | +6.0% | +3.9% | +8.8% | -1.1 Percentage Points | |
| GMS | 2019/20 | 2,900 | £237,400 | £131,600 | £105,800 | 55.4% |
| 2020/21 | 2,900 | £251,400 | £136,600 | £114,800 | 54.3% | |
| Change | 0 | +5.9% | +3.7% | +8.6% | -1.1 Percentage Points | |
| PMS | 2019/20 | 400 | £269,600 | £160,800 | £108,800 | 59.6% |
| 2020/21 | 350 | £290,400 | £170,100 | £120,300 | 58.6% | |
| Change | -50 | +7.7% | +5.8% | +10.5% | -1.0 Percentage Points |
GPMS Contactor GPs – mean earnings and expenses by contract type, Scotland, 2019/20 and 2020/21[49]
298. During 2017 the Scottish Government commissioned Deloitte to undertake a Review of GP Earnings and Expenses[50]. It found that 70% of practice costs (on average) were staffing costs, followed by premises which accounted for 16% of practice costs.
299. There was some evidence indicating that partners in urban practices earned on average more than partners in remote practices. No correlation between average net income and deprivation was found. There was also some limited evidence that larger practices had a higher net income per partner GP than smaller practices.
Workforce Data for Scotland
300. The Primary Care Workforce Planning Survey Scotland 2019 captures aggregate workforce information from Scottish general practices and each of the NHS Board-run GP Out of Hours services. It provides the most comprehensive information available on the staffing cohort of general practice, both in hours and out of hours, but does not provide the cost. The costs of running a practice are a matter for the GP partners, including what pay they award employees. The 2019 survey was published in October 2021[51].
301. The 2019 results for Scottish general practices are based on survey data received from 830 responding practices. Of these, 76 did not fully complete the survey, 311 did not provide suitable unique identifiers (National Insurance Numbers) for their staff, and 40 practices submitted no GP data. The results include information on:-
- Estimated WTE numbers of GPs in post in Scottish general practices, along with information on patterns of sessional commitment by age and gender (a GP's week is typically defined in terms of sessions rather than hours, with a working day generally being comprised of two or sometimes three sessions).
- Estimated headcount and WTE numbers of nurse practitioners and other registered nurses employed by Scottish general practices, along with information on the age profile of these staff.
- Use of locum GP time and extra nurse time by Scottish general practices.
- Known vacancies for these professional groups in general practices from 1 April 2018 to 31 March 2019.
302. The Primary Care Out of Hours workforce survey was published in 2019 and the main points from that survey were:
- The number (headcount) of GPs working for Primary Care Out of Hours (OoH) services in Scotland in the year ending 15th November 2019 was 1,879, equating to an estimated Whole Time Equivalent of 329.6.
- Within Primary Care OoH services, 9% of the GPs worked 1,000 hours or more over the year and their total annual hours accounted for nearly half (45%) of the total GP hours worked.
- Eight NHS Boards had to take additional action at least weekly to ensure shifts are filled, either by extending shifts, having nurses cover GP shifts or vice versa, or by offering additional financial incentives.
- As observed in previous surveys, GPs aged over 55 years worked a higher average number of hours per week in Primary Care OoH services than younger GPs.
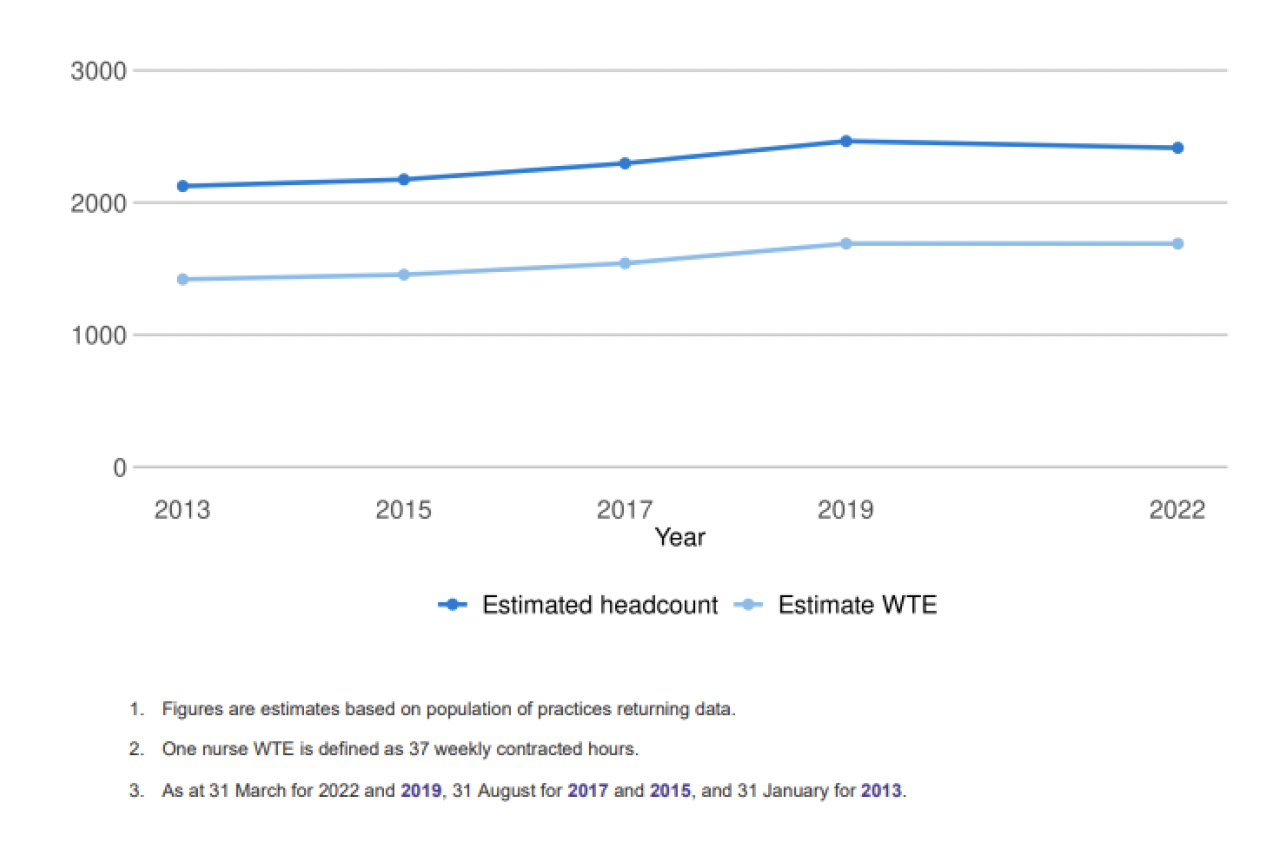
303. The estimated number (headcount) of registered nurses working in GP practices in Scotland in 2022 was 2414, a decrease of 51 from the 2019 survey. The estimated WTE for all nurses was 1,690 (based on 37 hours or more per week being full time), representing the same estimated WTE as the 2019 survey.
304. The largest group of nurses working at General Practices were General Practice Nurses, accounting for 63% of the estimated Nurse headcount and 60% of the estimated Nurse WTE. The next largest group are Advanced Nurse Practitioners (ANPs) and Nurse Specialists, accounting for 27% of the estimated Nurse headcount and 31% of the estimated Nurse WTE.
305. The figures from this survey do not represent the entire registered nurse workforce working in Scottish general practices. They exclude nurses who are employed by NHS Boards but who work in independent contractor practices.
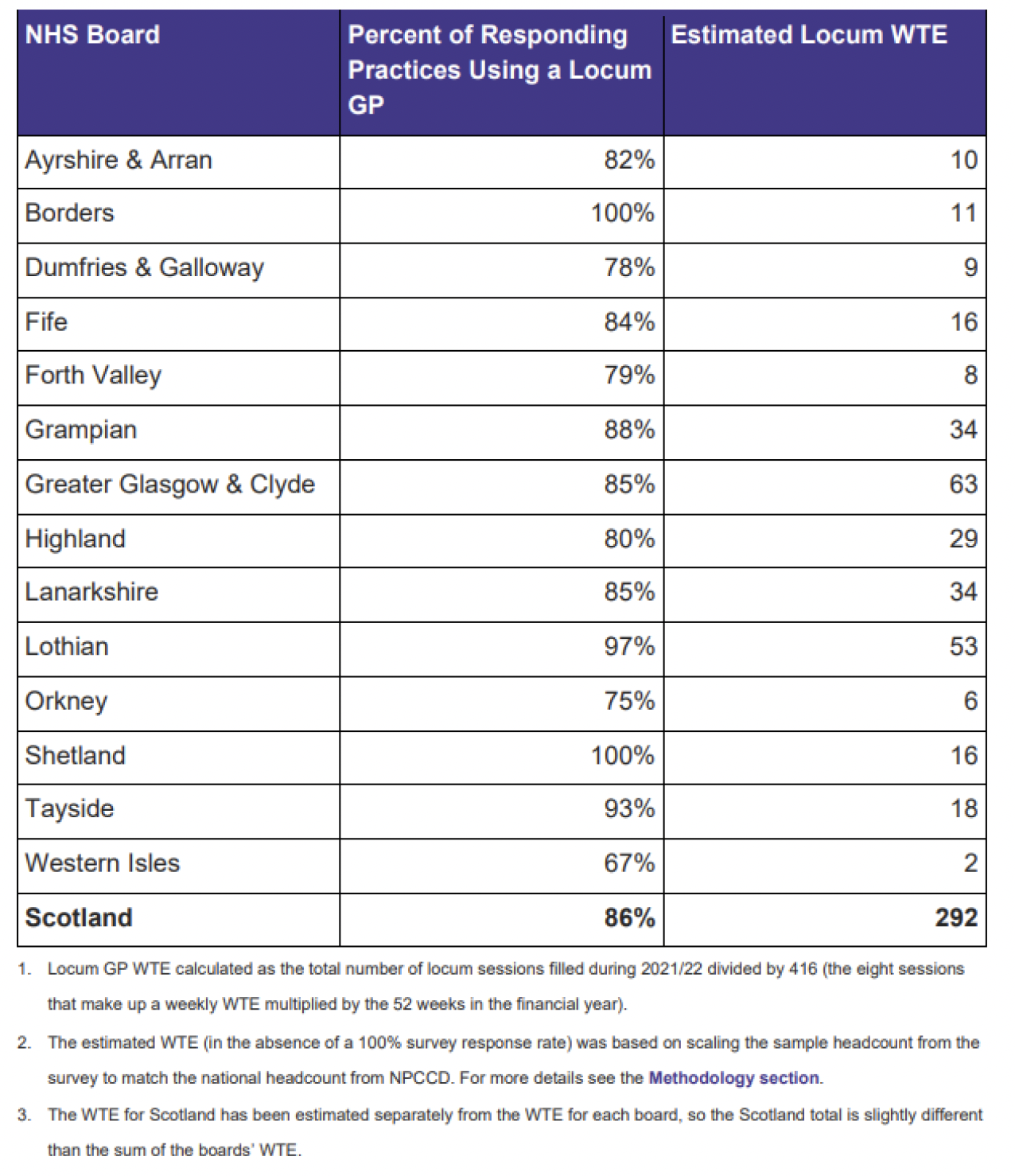
306. Overall, 86% of all responding practices reported the use of a locum GP during 2021/22, with the estimated use of 292 Locum GP WTEs. This is higher than the 273 WTE estimated from the 2019 survey.
Number of internal locum sessions required over 12 months, Scotland; 2013 - 2017[52]
307. There were an estimated 479 Health Care Assistants with an estimated WTE of 317 working in Scottish general practice in 2022 (as at March 31). This shows a 24% decrease in headcount (estimated 627 in 2019) and a 23% decrease in estimated WTE (410 in 2019) compared with the previous survey. For phlebotomists, there were an estimated 103 working at General Practices in Scotland in 2022 with an estimated WTE of 59.6. This shows a similar estimated headcount as in 2019 (104), but with a 5% higher estimated WTE (54 in 2019) compared with the previous survey.
308. The 2018 GP Contract mandates the provision of workforce data to be made mandatory. This will facilitate workforce planning in the future.
Working Hours
309. The Primary Care Out of Hours Workforce Survey Scotland 2019[53] gathered information on GPs working in GP Out of Hours services.
310. Results from the 2019 survey showed that younger GPs were more likely to input fewer hours with the average for under 35s being 3 hours and for 35 to 44 year olds, 6 hours per week on average. This contrasts to those aged 45 to 54, contributing 8 hours, 55 to 59 year olds contributing 9 hours, 60 to 64 year olds contributing 11 hours and those aged 65 years and over contributing 11 hours per week on average.
311. GPs aged under 35 years made up 20% of the OoH workforce, but their combined hours accounted for just 10% of the total hours. Likewise, for GPs aged 35 to 44 years, while they made up 37% of the workforce, their combined hours accounted for only 31% of the total GP hours worked in Primary Care OoH services. GPs aged 45 years and over made up 43% of the OoH workforce, but their reported combined hours accounted for 58% of the total GP hours worked in Primary Care OoH services.
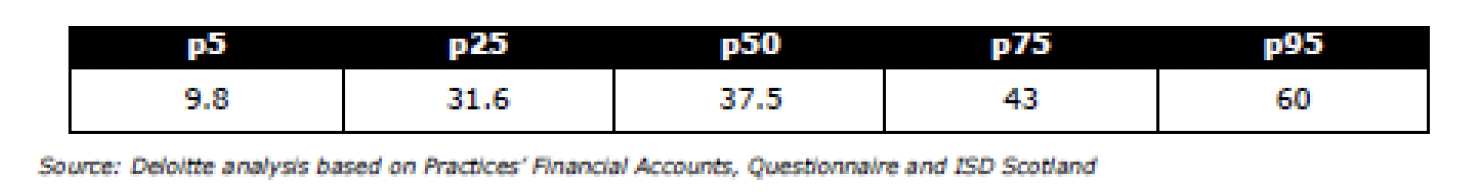
312. During 2017 the Scottish Government commissioned Deloitte to undertake a Review of GP Earnings and Expenses[54]. Like the workforce survey this was also based on a sample of GP practices, and found that GP commitment ranged from under 10 hours per week to over 60 hours per week.
Average weekly working hours by Partner GPs[55]
2. General Dental Practitioners (GDPs)
Introduction
313. This evidence refers to independent contractor General Dental Practitioners (GDPs) that provide General Dental Services (GDS).
314. GDPs are independent contractors who have undertaken to provide NHS dental services on behalf of NHS Boards. They can be either GDPs who are owners, directors or partners of a dental practice (principals) or self-employed GDPs who enter into arrangements with principal GDPs – which is neither partnership nor employment (associates). Independent contractors may engage assistant dentists, including vocational dental practitioners, to assist with the provision of GDS.
315. The evidence provided in this submission reflects the period through the Covid-19 pandemic, considering its impacts on the sector over the course of a prolonged period of recovery of NHS dental services. Reflecting too on the removal of emergency financial support measures since April and significant improvement in NHS dental activity after then through a reanimation of payment linked to activity through Item of Service (IoS) and 'multiplier/ bridging' payments that have been in place during the 2022/23 financial year.
316. At present the sector is delivering levels of care and treatment that are analogous to the pre-pandemic position and Scottish Government intends to build on this success by bringing forward necessary reforms to the payment system, including a focus on preventive and anticipatory care during 2023/24.
Background
317. The impact of the pandemic on the NHS dental service has been prolonged and significant, beginning with the full cessation of High Street dental services and introduction of emergency financial support arrangements from 23 March 2020. The recovery of services during 2020 was greatly influenced within the cautious approach taken by Scottish Government that culminated in the re-instatement of the full NHS treatment list from 1 November 2020. Throughout 2020 to early 2022 there were also significant clinical and public health constraints placed on the sector, in particular around the use of Aerosol Generating Procedures (AGPs).
Financial Support arrangements
318. The financial support arrangements that have been in place through the pandemic were successful in supporting the sector through the financial challenges that the sector faced as part of the wider effort to combat Covid-19. There have been three main stages:
a. Stage 1: March to October 2020: Financial support focused on two main areas – 80% gross IoS and also an uplift of 30% General Dental Practice Allowances (GDPA). This phase supported the generally cautious approach that Scottish Government followed at this stage of the pandemic.
b. Stage 2: November 2020 to March 2022: Financial support was the same approach as Stage 1, however, gross IoS payments were increased to 85% to further support contractors providing care to patients. Over the course of this part of the pandemic the overall level of activity levelled out at around 40 to 45% of pre-pandemic levels, highlighting that there was a reduced level of patient access to NHS dental services. Scottish Government took an active supporting role with Health Boards to support practices with very low levels of activity to enable improvements. By the end of the 2021/22 financial year Scottish Government were clear that activity and patient access to care needed to be increased.
c. Stage 3: April 2022 to current: In a letter on 21 October 2021, the Cabinet Secretary issued the sector with a letter, noting "that sustaining the pre-pandemic blended payments system is the only practical way to recover the sector and clear the patient care backlog". This letter also signalled some initial changes to fees from 1 February 2022, alongside the withdrawal of the emergency financial support. Letter from the Cabinet Secretary to NHS dental teams | Scottish Dental
319. In addition, to the activity and patient access to NHS dental services by early Autumn 2021, it was clear that the wider position across specific sectoral emergency financial support arrangements was generally coming to an end. The IPC public health protocols provided an additional complexity, as while these measures supported control of the spread of Covid-19, when combined with the financial support measures in place it is likely to resulted in a more general reduction in levels of activity.
February 2022 (improved payment incentivisation)
320. The first step that was taken was in February 2022 to deliver significant changes to a small number of fees – focusing on examination appointments, preventive provision for children and diagnostic. In particular, the introduction of the enhanced examination appointment, which included the addition of children in the exam fee for the first time provided contractors with an improved incentive to bring patients into their practices. This was delivered in advance of the withdrawal of the financial support measures to support the sector tackle the backlog in care that was present at that point.
Withdrawal of financial support measures / 'multiplier' arrangements
321. In the Autumn / Winter 2021/22 it was clear that there were significant concerns within the sector about the withdrawal of the financial support measures, in one step at the end of March 2022, noting the potential for a cliff-edge. Scottish Government actively and robustly responded to these concerns through the development and introduction of a 'multiplier' arrangement.
322. While there was a clear need for the Scottish Government to secure more activity and deliver improved patient access to care there was also significant IPC controls in place, that provided a limiting factor on the provision of care. Scottish Government was clear that while it was essential to withdraw the financial support arrangements it was equally clear of the need to sustain and maintain NHS dental service provision.
323. As stated by the Cabinet Secretary in the October letter Scottish Government were clear that the blended payment system (allowances, cap & con and IoS) is essential to the delivery of NHS care and treatment. In an overall context that had also to reflect the main concerns around cliff-edge, mitigation of IPC conditions suppressing activity and value for money. In close discussion with BDA there was a period of significant engagement and an outcome that was not formally agreed to introduce the temporary 'multiplier' from 1 April 2022. The arrangement supported the delivery of patient care and treatment through IoS activity.
324. The temporary 'multiplier' was introduced with a quarterly review point, whereby, the rules that were applied to IPC conditions, levels of activity, value for money were considered. The temporary 'multiplier' was initially set at 70%, which meant that for every £1 earned through IoS a further £0.70p was added to the total income. The introduction of this arrangement coincided with a significant reduction in IPC conditions and this reduction, allied to increased incentivisation provided the sector with the opportunity to significantly improve levels of activity.
325. This meant that the review for quarter two indicated that the temporary 'multiplier' arrangement could be safely reduced from 70% to 30%. Over the course of this period it has become clear that the sector overall is broadly and consistently operating close to pre-pandemic levels of activity and that IoS earnings are comparable.
Bridging Payment
326. Scottish Government welcomes the increased in levels of activity and patient access to NHS dental services. Across the sector, the focus on reform is a vital next step to deliver sustainable NHS dental services. In this connection, the temporary 'multiplier' was modified to reflect the present situation that IPC mitigation was less necessary, while the wider situation around 'cost of living' being a key driver for the change. This modification of the 'multiplier' to a temporary 'bridging' payment supports Scottish Government ambitions to deliver a more sustainable payment. The temporary 'bridging' payment has been confirmed to the sector at 20% in Q3 and 10% in Q4.
327. The monthly statistics from Public Health Scotland continue to show that considerable progress has been made in ensuring access to NHS dental services and oral health improvements: NHS Dental Treatment Statistics - Month ending 30 September 2022 - NHS Dental Treatment Statistics - Publications - Public Health Scotland. There have been over 1.3 million NHS examination appointments have been completed, since April to September this year.
328. Across key treatment items NHS dental services is at comparable levels of activity to levels last seen before pandemic restrictions were introduced. Since April 2022, the sector is presently averaging over 300,000 courses of NHS dental treatment per month and are on course for over 3.5 million contacts in the 2022/23 financial year.
Overview of pandemic related financial support
329. During the pandemic financial support arrangements were in place to support dental incomes because the payment system provides patient care and treatment largely through IoS payments. Low levels of activity in the sector under these arrangements meant that the sector would have been unviable without financial support arrangements. From March 2020 to April 2022 Scottish Government has spent an additional c. £150m supporting the NHS dental sector to maintain capability to deliver NHS services. Noting that IoS income levels across the sector are broadly, with some variation between practices but overall levels arein line with pre-pandemic levels and have been enhanced further by 'multiplier' and 'bridging' payments.
Pay Award for 2021/22
330. Scottish Government accepted the pay increase recommendation of 3% for GDPs. As in previous years, the increase was applied to gross item of services fees, and capitation and continuing care payments. As NHS dental contractors were continuing to receive emergency support payments the Scottish Government also applied a 3% increase to the value of the financial support payments. The 3 per cent increase was calculated based on the uprated 100% value of the financial support payment in the November paid December 2021 schedules.
Pay Award for 2022/23
331. Scottish Government accepted the pay award of 4.5% for GDPs and this was implemented from 1 November 2022. As in previous years, it will apply to gross item of services fees, and capitation and continuing care payments. NHS dental contractors have been in receipt of both multiplier payments and bridging payments during the 2022/23 financial year, the 4.5% pay award will be applied to both of these payments.
332. Both 2021/22 and 2022/23 pay awards contained a backdated element.
Pay Award for 2023/24
333. The Cabinet Secretary for Health has set out to the profession that 'bridging' payments will be made in respect of IoS until the end of the current financial year, with the intention to focus delivery of payment system reform from April 2023. The intention would be to apply a pay award for 2023/24 within the reformed payment system structures to ensure consistency of IoS payment values and surety for contractors delivering care and treatment to NHS patients.
334. The trend since April 2022 is that NHS dental activity has increased significantly, as the re-introduction of performance related pay through IoS (allied to multiplier and bridging payments) and reduction in IPC constraints has enabled sector earnings on average return to pre-pandemic levels. The increase in patient access to care is a relative success in the wider health context, however, it is a potentially fragile situation overall that will require significant reform of the payment system to deliver longer term stability.
Reform
335. Through the course of the pandemic Scottish Government has sought to ensure that the NHS dental sector is provided with a stable financial environment – as seen through the emergency payments / 'multiplier' and 'bridging' payments. It is the intention that the current focus on payment system reform builds on this to ensure business continuity over the longer term.
336. Scottish Government has been carefully developing significant payment system reform, including wide engagement with the sector through a survey and more detailed discussions with an Advisory Group about the clinical requirements necessary to deliver NHS dental care through a reduced list of fee codes. Work is developing around a structure that includes around the 35 to 40 code range against the current 700 codes, which is intended to support clinicians provide improved person centred care.
337. Scottish Government is clear that the current blended payment model provides the most effective use of public spending on NHS dental services, driving treatment through IoS while at the same time supporting practices through Cap&Con and allowances payments (such as GDPA and rent). The focus of the payment system reform is to deliver key aspects of the 2018 Oral Health Improvement Plan (OHIP) around preventive care and improve periodontal provisions, alongside enabling clinical discretion for contractors to deliver patient focussed care – based on the individual patient needs.
338. The dental sector has undergone a long period of recovery through the pandemic and the significant improvement in levels of activity seen since April 2022 are indicative of the sector generally being in a position to operate at a high level. As part of the longer term planning to deliver sustainable NHS dental services the focus at present is to build on pre-pandemic OHIP to deliver a reduced number of fee codes that can more easily reflect activity.
339. The reform work is being developed through the Advisory Group forum and this is developing a clear picture of the clinical aspects required for NHS dental services and the papers from these meetings are provided: Updated 1/12 – CDO Advisory Group – Meeting Papers | Scottish Dental. There will be a further process to determine fees and pricing in the New Year.
340. The Cabinet Secretary wrote to the sector on 23 September 2022 about the 'bridging' payment, reform plans and also Scottish Government intention to undertake an 'open books' expenses exercise. In particular, he signalled that officials will write to practices who are mainly NHS and ask them to share their accounts. This will allow Scottish Government to understand the impact of business costs on NHS practice and help inform future pay awards: Letter to NHS dental teams from the Cabinet Secretary for Health and Social Care | Scottish Dental
Links to relevant information:
- NHS dental contractor workforce information is available through a recent NSS report: 06 December 2022 CAMHS | Turas Data Intelligence (nhs.scot)
3. Consultants including Improving the working lives of Consultants
341. A tripartite forum with MSG (NHS Scotland employers/Scottish Government) and BMA Scotland meets regularly to discuss matters of common concern and, where appropriate, produce joint guidance on these areas.
342. A consistent issue that has been raised in this space by BMA is the impact Pension Taxation charges are having on the consultant workforce with claims many senior clinicians either reducing their commitment to NHS Scotland or retiring from the service altogether.
343. Whilst the Scottish Government has extremely limited powers in relation to Pension Taxation we have listened to the BMA's concerns and have delegated the powers to NHS Boards to offer Pension Recycling. NHS employers worked with BMA Scotland to develop a scheme which is now in operation.
344. Under the scheme, staff impacted by annual allowance charges can withdraw from the pension scheme and receive the contributions their employer normally makes to their pension as a 12.4% addition to their salary. Arrangements were officially signed off in early December.
345. We are however cognisant of the need to maintain the overall NHS Pension Scheme and recognise that offering Pension Recycling in the long term is not a sustainable solution. Whilst the UK Government's recent commitment to correct the NHS Pension Scheme rules to mitigate the impact of inflation on pension tax calculations is welcomed and we are consulting on making similar amendments to the Scheme in Scotland, it does not fix the substantive issue of pension tax rules impacting on the choices senior clinicians are making to reduce their commitments or retire early. We believe that a permanent solution is required to this issue and only the UK Government can deliver this.
4. Distinction Awards and Discretionary Points for Consultants
346. Since 2010, no new Distinction Awards have been made. The Consultants still receiving these are those who were successful prior to the freeze being imposed. We have been clear that that existing arrangements for DAs and DPs would remain in place and our position, since 2010 has been that to increase or restore DADPs would go against progressive pay principles.
347. The Scottish Government values the enormous contribution NHS Scotland staff makes to our health service. It is right that our aim is to attract and retain highly skilled and much sought-after staff. There is no evidence to suggest that an adverse impact has resulted from the freezing of the value of DADPs.
348. Although DAs are frozen to new consultants, the availability of new DPs increases in line with the number of consultants in post. Scotland continues to offer an attractive pay package for Consultants along with the continued guarantee of No Compulsory Redundancy.
349. We are therefore not seeking any recommendations from DDRB on distinction awards and discretionary points.
5. Junior Doctors including Improving the working lives of Junior Doctors
350. Work to implement the recommendations of the Expert Working Group report on a maximum 48 hour working week for junior doctors with no averaging, has started. In partnership with the BMA and employers, we continue to work to identify specific areas where actual operational improvements can be made to working lives of Junior doctors.
351. In June 2022 we issued guidance to NHS Boards restricting the consecutive days of long shifts (greater than 10 hours) to a limit of 4 in any seven days. This was both an Expert Working Group recommendation and key priority within the BMA Wellbeing report. The goal is to achieve full compliance, which on target to be achieved by February 2023.
352. We have started work with the BMA and employers to facilitate broader improvements to rota design and to improve earlier sight of rotas for Junior Doctors, and will soon be establishing a forum to look at improvements to New Deal Monitoring reporting and rest periods (breaks). In addition we are undertaking a test of change in relation to sleep pods to help reduce tiredness and fatigue in the workforce.
353. In respect of pay, the Scottish Government was approached in the third quarter of 2022 by the BMA Scottish Junior Doctor Committee (BMA SJDC) regarding the 2022/23 pay award. The BMA SJDC requested an additional increase to the 22/23 pay award which would have breached RPI, and a commitment to Pay Restoration of 23.5% over a five year period. To implement such a request would mean reprioritising health and other public sector spend which would negatively impact already pressurised services and we believe this request to be simply unaffordable in the current climate.
354. We do however recognise the current cost of living pressures and the impact they are having on many workforces, and Junior Doctors report they are no exception, comparing t their level of earnings with Agenda for Change rather than senior medical staff. We recognise the specific challenges faced by junior doctors, and that their earnings are more comparable in the training period to AfC. In addition, the transient nature of the workforce means that the unprecedented inflationary pressure being faced across the economy can impact more greatly on Junior Doctors as they rotate within the service.
355. With this in mind and taking into account current and projected inflationary levels during 2023, we would ask that you consider making a separate and specific recommendation for Junior Doctors for the 2023-24 DDRB pay review round.
6. Specialty Doctors and Associate Specialists (SAS) including Improving the working lives of SAS Doctors
356. The Scottish Government declined to join contract discussions with the rest of the UK on SAS doctors. Instead, it was agreed we would seek a Scottish solution to reform the Speciality Doctor contract, including the potential development of a Senior Speciality Doctor grade.
357. In the autumn of 2022, after many months of negotiation, the Scottish Government came to an agreement with employers and the BMA on the creation of a new contract for both the Speciality and Associate Specialist Doctors and Dentists in NHS Scotland.
358. These new contracts were accepted by BMA members at ballot, and the contracts were implemented on 1 December 2022.
359. The contract brings forward improved pay and contractual arrangements for Specialty Doctors, and introduces a new medical grade to NHS Scotland, the Specialist Doctor which is fully welcomed by both employers and BMA.
360. Current Specialty Doctors will have the opportunity to move to the Specialty Doctor arrangements or chose to stay on their current terms and conditions.
361. The new grade is an addition to our Senior Medical staffing cohort and is able to act as an autonomous senior decision maker. This will provide an alternative career opportunity for many doctors in NHS Scotland.
362. As we are the middle of the implementation phase, the Scottish Government will continue to monitor the uptake and progress of the new contract and the creation of the new role.
7. Locums
2022/23
363. The annual spend on agency medical locums in secondary care in NHS Scotland increased by 16.9% from £87.6M to £102.4M from 2020/21 to 2021/22.
364. Total agency spend on all staff remains a tiny fraction of the NHS Scotland £9 billion staffing budget, and we continue to explore ways in which we can drive down the use and cost of agency staff.
365. We have in place a framework preferred supply arrangement who provide staff on NHS rates of pay. In addition we have well developed HNS Staff Bank arrangements, with enhanced rates for medical staff.
366. The Chief Nursing Officer has established a Task and Finish Group to explore all options to reduce the use and cost of agency staff.
367. We should however recognise that in order to ensure service continuity during times of planned and unplanned absences, an organisation as large and complex as NHS Scotland will always require a degree of temporary staff from both internal and external sources. Our actions are designed to ensure that agency staff are used as a very last resort.
Contact
There is a problem
Thanks for your feedback