Primary care improvement plans - implementation progress summary: March 2023
This publication provides a summary of the current progress towards implementation of the Memorandum of Understanding (MoU) between the Scottish Government, the SGPC, Integration Authorities and NHS Boards.
Primary Care Improvement Plans : Summary of Implementation Progress at March 2023
1. Introduction
This management information publication provides a national summary of the progress towards implementation of the Memorandum of Understanding ("MoU": see section 3 for more information about what this is). It covers the period up to the end of March 2023 and is based on data provided by Integration Authorities (IAs) in May 2023. It updates the information published in June 2022. The data at IA/NHS Board level is available in the spreadsheet accompanying this publication.
2. Data quality
The data included in this report is provided by IAs. Information on workforce numbers is sourced from local systems which are dynamic and primarily used for operational purposes. The data can therefore change over time and the figures presented here are the best available estimates. The Scottish Government is working with IAs to improve data quality and previously published information may change from one publication to the next to reflect these refinements.
In order to improve our understanding of the wider workforce providing services, for this period, we collected information for both staff funded by Primary Care Improvement Fund and other sources for the first time. This means figures may differ from the previously published information, and that some staff previously noted as being PCIF funded may now be included in other funding, due to this being explicitly collected.
In previous years, we had collected data on whether areas had full or partial access to services. This year, in order to ease burden and reduce discrepancy between areas, we simply asked if areas have access to a service. These figures therefore include access levels from minimal access to full access and should be interpreted as such. We continue to work with areas on granular detail and collecting information on activity and capacity levels.
Additionally, where we have access details for multiple subservices within a MOU priority area, we have collected the number of practices which have access to none of those sub services. This means practices with access to at least one of the services will be the same or larger than those of the individual subservices.
3. Background
The 2018 GP Contract Offer ("the Contract Offer") and its associated Memorandum of Understanding ("MoU") between the Scottish Government (SG), the Scottish General Practitioners Committee of the British Medical Association (SGPC), Integration Authorities (IAs) and NHS Boards was a landmark in the reform of primary care in Scotland. The Contract Offer refocused the General Practitioner (GP) role as expert medical generalists to enable GPs to do the job they train to do and deliver better care for patients. It committed to a vision of general practice being at the heart of the healthcare system where multidisciplinary teams (MDT) come together to inform, empower and deliver services in communities for those people in need of care. It recognised the statutory role of IAs in commissioning primary care services and service redesign to support the role of the GP as an expert medical generalist. It also recognised the role of NHS Boards in service delivery and as NHS staff employers, and parties to General Medical Services (GMS) contract.
In 2021 the MoU was refreshed (the MoU2) to cover the period 2021-2023 between the same Parties. The key aim remains expanding and enhancing multidisciplinary teams working to help support the role of GPs as expert medical generalists, to improve patient outcomes. The MoU Parties recognised a great deal has been achieved however there is still a way to go to fully deliver the GP Contract Offer commitments originally intended to be delivered by April 2021.
The original MoU sets out the six priority service areas where it has been agreed that IAs, in partnership with Health Boards and GPs, will focus:
- Vaccination Transformation Programme (VTP);
- Pharmacotherapy;
- Community Treatment and Care Services (CTAC);
- Urgent Care;
- Additional Professional Roles;
- Community Links Workers (CLW).
All of these services are currently available to patients, however in most cases these had historically been provided by individual GP practices. Following the joint SG/SGPC letter of December 2020, the focus for 2021-22 was on Pharmacotherapy, CTAC and VTP services. More information about what these services include and the anticipated new models of delivery are provided in Section 6.
Funding to support the implementation of the MoU has been allocated to IAs through the Primary Care Improvement Fund (PCIF), and locally agreed Primary Care Improvement Plans (PCIPs) covering all 31 IA areas of Scotland were developed by the end of July 2018. The PCIPs set out in more detail how implementation of the six priority service areas will be achieved. IAs are required to provide updates on their PCIPs on an annual basis, and data including workforce numbers and spread of services every six months through an agreed standard tracker template. The trackers also include space for free text comments to provide context to the data provided.
The delivery of primary care transformation is occurring within a complex local landscape. IAs must work closely with local communities and other stakeholders to ensure that PCIPs address specific local challenges and population need. They must also agree where the local priorities lie for the services being reformed. As a result of this, there is geographical variation in service design and delivery models. Service design and implementation progress has also been affected by a number of external factors in recent years, including the legacy impacts of the pandemic as well as, more recently, the cost of living crisis.
4. Workforce numbers
Table 1 shows the number of whole time equivalent (WTE) staff working to support implementation of the six priority services agreed in the MOU.
The data returned shows 4,730.9 WTE staff working in the MOU services in March 2023, with 3,233.2 funded through the Primary Care Improvement Fund and 1,497.7 funded through other sources.
There was an increase of 518.0 WTE staff between March 2022 and March 2023, with an increase of 286.7 funded through the Primary Care Improvement Fund.
While increases in workforce may be indicative of progress towards delivery of the MoU, there is in general no expectation of specific workforce levels which are required across Scotland.
It should be recognised that there may be variation in appropriate staffing numbers depending on the clinical model developed, the skills mix of the workforce and local population needs.
| PCIF funded | Other funded | Total | PCIF funded | Other funded | Total | ||
|---|---|---|---|---|---|---|---|
| Mar-22 | Mar-22 | Mar-22 | Mar-23 | Mar-23 | Mar-23 | ||
| Pharmaco-therapy | Pharmacist | 552.8 | 79.6 | 632.5 | 560.1 | 97.7 | 657.9 |
| Pharmacy Technician | 366.4 | 21.7 | 388.1 | 393.9 | 34.7 | 428.6 | |
| Assistant/Other Pharmacy Support Staff | 45.9 | 4.2 | 50.1 | 116.5 | 9.3 | 125.7 | |
| Vaccinations | Nursing | 240.0 | 287.2 | 527.2 | 216.3 | 300.9 | 517.2 |
| Healthcare Assistants | 79.7 | 330.9 | 410.5 | 68.3 | 361.0 | 429.3 | |
| Other | 49.8 | 169.4 | 219.1 | 63.0 | 140.0 | 203.0 | |
| CTAC | Nursing | 323.4 | 92.6 | 416.0 | 369.3 | 150.6 | 519.9 |
| Healthcare Assistants | 384.2 | 53.0 | 437.2 | 444.8 | 91.3 | 536.1 | |
| Other | 79.2 | 3.7 | 82.9 | 85.9 | 8.4 | 94.4 | |
| Urgent Care | Advanced Nurse Practitioners | 182.0 | 12.7 | 194.7 | 206.6 | 13.3 | 219.9 |
| Advanced Paramedics | 8.0 | 1.0 | 9.0 | 9.8 | 1.0 | 10.8 | |
| Other | 28.4 | 11.0 | 39.4 | 22.5 | 20.8 | 43.3 | |
| Additional professional roles | Mental Health workers | 154.5 | 137.0 | 291.5 | 186.4 | 188.6 | 375.0 |
| MSK Physios | 173.0 | 11.5 | 184.5 | 206.0 | 19.3 | 225.3 | |
| Other | 36.8 | 3.0 | 39.8 | 30.4 | 6.0 | 36.4 | |
| Community Links Workers | 242.5 | 47.9 | 290.4 | 253.5 | 54.8 | 308.2 | |
| Total | 2946.5 | 1266.3 | 4212.8 | 3233.2 | 1497.7 | 4730.9 | |
5. NHS Board provided services
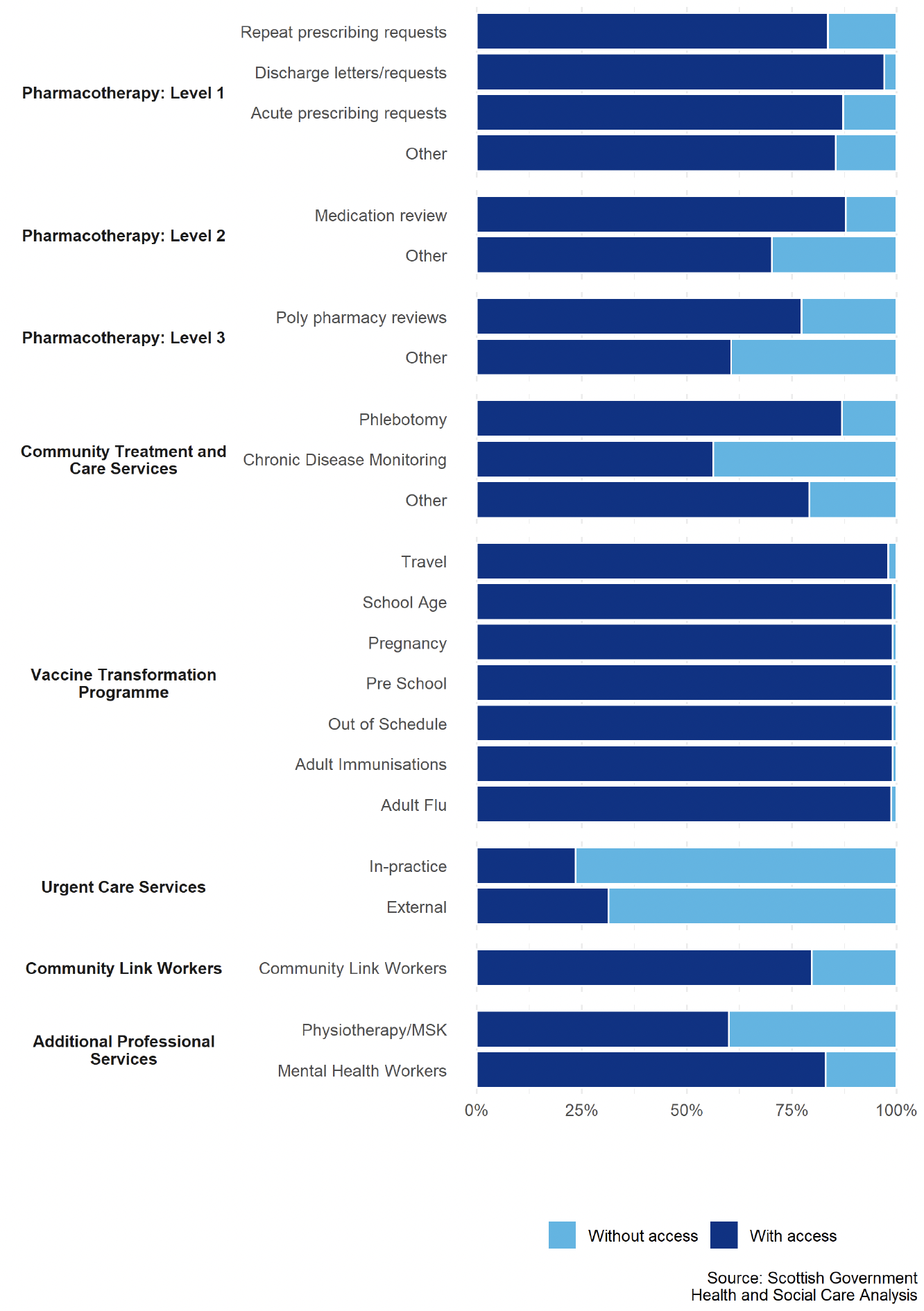
The additional staff described in section 4 above enable NHS Boards to provide an increased range of services, in accordance with the MoU. All of these services are currently available to patients, however in most cases these had historically been provided by individual GP practices. Chart 1 illustrates the percentage of GP practices whose patients can now access these services directly from their NHS Board. The data relating to this chart can be found in the spreadsheet which accompanies this publication.
It is not expected that all GP practices in Scotland will take up these NHS Board provided services. Because service delivery models are designed specifically according to local population needs, there are variations in approach across the country. For example, there may be some GP Practices where there is no defined need for a particular professional role. These services may therefore never reach 100 per cent coverage. There may also be local circumstances where local Primary Care Improvement Programme Boards determine it is necessary for one or more local GP practices to continue delivering one or more services intended to transfer to board-employed MDT under the MoU.
Almost all practices have access to at least one of the pharmacotherapy services provided by NHS Boards. At an IA level, between 84 per cent and 97 per cent of practices have access to different level 1 subservices as at March 2023. Around 70 to 88 per cent of practices have access to level 2 subservices, and between 61 and 77 per cent of practices have access to level 3 subservices.
In total 91 per cent of practices have access to at least one of the NHS Board provided CTAC services. As at March 2023, 87 per cent of practices have access to Phlebotomy, 56 per cent of practices have access to Chronic Disease Monitoring, and 79 per cent of practices had access to Other CTAC services.
The roll out of the Vaccination Transformation Programme is well advanced. As at March 2023, all practices have access to at least one of the NHS Board provided VTP services. More than 99 per cent of practices have access to school age, pregnancy, pre school, out of schedule, and adult immunisations vaccinations. Just under 99 per cent of practices have access to adult flu vaccinations, and travel vaccinations are accessed by 98 per cent of practices. Many areas are operating a blended model of GP and NHS Board delivery, with community nurses, pharmacies, schools and maternity wards all playing an important role.
NHS Board-provided urgent care services are accessed by 42 per cent of practices. Here 24 per cent of practices have access to in-practice services and 31 per cent of practices have access to external services.
Eighty per cent of practices have access to a community links worker, whose services were not intended to be universal but allocated on the basis of need. Additional professional services include physiotherapy and mental health workers. Sixty per cent of practices have access to a musculoskeletal physiotherapist, and 83 per cent of practices have access to a mental health worker.
6. Background notes: Definitions
The services included in the MoU are defined as follows. As indicated above, there may be geographical and other limitations to the extent of any service redesign and local needs which need to be determined as part of the PCIP.
Vaccination Transformation Programme - The Vaccination Transformation Programme was announced in March 2017 to review and transform vaccine delivery in light of the increasing complexity of vaccination programmes in recent years, and to reflect the changing roles of those historically tasked with delivering vaccinations.
IAs have delivered phased service change based on locally agreed plans as part of the PCIP to meet a number of nationally determined outcomes including shifting of work to other appropriate professionals and away from GPs. In October 2021, regulation change removed vaccinations from the GMS contract, supplemented by legal directions which were issued in August 2022, providing a framework to conclude the role of most GP practices in providing vaccinations. PCA(M)(2022)13 provides the current position on the programme.
Pharmacotherapy - These services are in three tiers divided into core and additional activities, to be implemented in a phased approach.
Phase one included activities at a general level of pharmacy practice including acute and repeat prescribing and medication management activities. This is to be followed by phases two (advanced) and three (specialist) which are additional services and describe a progressively advanced specialist clinical pharmacist role.
Regulations have been amended by Scottish Government so that NHS Boards are responsible for providing a pharmacotherapy service to patients and practices. The use of medicines to treat and care for patients will remain an important part of GP work. The delivery of electronic prescribing is an essential requirement for all involved in prescribing, which will be prioritised by the ePharmacy Programme Board, supported by National Services Scotland and the NHS Education for Scotland Digital Service.
Community Treatment and Care Services - These services include, but are not limited to, basic disease data collection and biometrics (such as blood pressure), chronic disease monitoring, the management of minor injuries and dressings, phlebotomy, ear care, suture removal, and some types of minor surgery as locally determined as being appropriate.
Scottish Government have amended regulations for the delivery of CTAC Services so that Boards are responsible for providing a Community Treatment and Care service. These services will be designed locally, taking into account local population health needs, existing community services as well as what brings the most benefit to practices and patients.
Urgent Care - These services provide support for urgent unscheduled care within primary care, such as providing advance practitioner resource (a nurse or paramedic) for GP clusters and practices as first response for home visits, and responding to urgent call outs for patients, working with practices to provide appropriate care to patients, allowing GPs to better manage and free up their time for more complex cases.
Additional Professional Roles - Additional professional roles provide services for groups of patients with specific needs that can be delivered by other professionals as first point of contact in the practice and/or community setting (as part of the wider MDT). These roles could include, but are not limited to:
- Musculoskeletal focused physiotherapy services
- Community clinical mental health professionals (e.g. nurses, occupational therapists) based in general practice.
Specialist professionals will work within the local MDT to see patients at the first point of contact, as well as assessing, diagnosing and delivering treatment, as agreed with GPs and within an agreed model or system of care. Service configuration may vary dependent upon local geography, demographics and demand.
MoU Parties will consider how best to develop the additional professional roles element of the MoU. In particular with Mental Health, there is a need to consider how PCIF funded posts interface with posts funded through other streams (such as Action 15).
Scottish Government continues to work with local areas on how we best align funding and reporting arrangements across different mental health funding streams in order to support greater understanding of the totality of service delivery, minimise administrative duplication and allow for more effective targeting of funding in local areas.
Community Links Worker is a generalist practitioner based in or aligned to a GP practice or Cluster who works directly with patients to help them navigate and engage with wider services, often serving a socio-economically deprived community or assisting patients who need support because of (for example) the complexity of their conditions or rurality. The roles of the CLWs should be consistent with assessed local need and priorities and function as part of the local models/systems of care and support.
Spread of Services have been categorised by IAs as: GP practices having any access to services, previously this was reported as full access; partial access; or no access. These figures therefore include access levels from minimal access to full access and should be interpreted as such.
7. Contact
For more information or queries on the information presented here please contact the Primary Care Policy Team at PCImplementation@gov.scot
Contact
Email: PCImplementation@gov.scot
There is a problem
Thanks for your feedback