Long Term Conditions Collaborative: Improving Care Pathways
A resource to improve care pathways for those with long term conditions.
1. APPLY GENERIC AND INTEGRATED APPROACHES
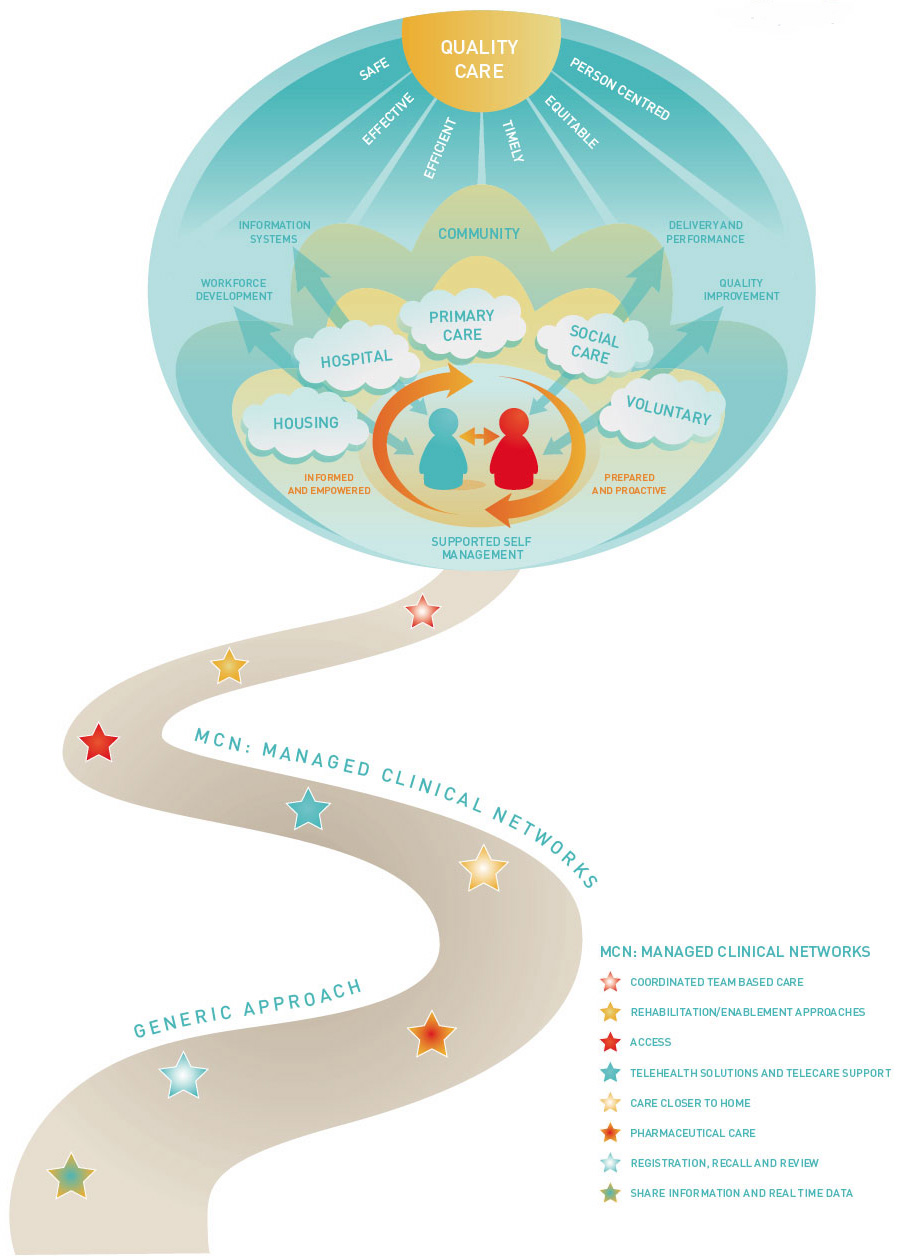
Figure 1
Improvement Actions:
- Include generic approaches in condition specific CPD programmes
- Develop integrated patient pathways for long term conditions
- Embed evidence-based guidelines in integrated care pathways
BACKGROUND
Many people live with more than one long term condition. A holistic approach to care frames evidence-based practice for each condition in the context of the individual's life circumstances. It also balances condition specific approaches with generic principles that apply to the management of all long term conditions. These principles include provision of information, advice and support to make appropriate lifestyle choices and changes; to adjust to the loss of mobility or manage chronic pain; to maintain psychological and emotional wellbeing; and to deal with employability and financial health issues. Underpinning these principles is the need for good quality information and clear signposting to care pathways so that the person and their carer can access the appropriate service at the right time and in the most appropriate setting, irrespective of their specific condition(s).
Most people self manage their long term conditions with help from family, community and voluntary sector and with some support from health and community care services. Community Health Partnerships ( CHPs) and MCNs need to fully involve service users and their carers if they are to promote a culture change that empowers supported self management and access to community-led health.
Formal care and support, when required, is largely delivered at home through services provided by primary care teams together with social care and housing partners as well as independent contractors such as community pharmacists. The capability and potential of community-based services is maximised through an effective extended primary and community team that in turn collaborates well with more specialist services. This extended community team and its specialist support has a key contribution to the delivery of care in community hospitals and in care homes.
This model requires an integrated approach to skills mapping, workforce development and support for ongoing education and development of the multi-professional team. It also requires defined pathways that support effective care, avoid needless delays, duplication and waste, reduce inappropriate variance in practice and improve access, coordination and continuity of care across teams, agencies and settings.
Pathways need to be viewed as a continuum and considered from the point of view of the person not the condition. They need to be well signposted so that they are easy to navigate for patients, their families and for staff providing care.
Good quality pathways ensure a timely, smooth and coordinated journey across the whole system and a better experience for all. They support care that is safer, more efficient and effective by making it easier for us all to do the right thing.
A Tiered Model for Care Pathways
The tiered model developed as part of the Forth Valley Integrated Healthcare Strategy offers a useful integrated framework to support you to take a generic approach to pathways for long term conditions. It illustrates how services and support can be tailored as needs change over time. It is a mechanism to design services that enable people to access the most appropriate care and support in the right setting.
The overarching principles of the model are to support people to be involved in care planning; enable them to be as independent as possible and to shift the balance of care though care and support provided by the most appropriate person and in the least intensive setting.
This is in line with the principles of person centred care and with our model for long term conditions management in Scotland. It should lead to a rational, coordinated approach to the design of care pathways, and help inform decisions about the most appropriate location of care, the type of health and social care inputs required and the desired outcomes.
The framework segments the local population into six tiers. Each tier represents a different set of circumstances and describes the appropriate service response for that situation.
Tier 0: Well
Describes services provided at home and in community settings with and for people who are well. Services aim to inform and educate the general public about lifestyle choices and self management, raising awareness of how to access services if needed. They may include targeted health improvement for those with risk factors for long term conditions as well as population wide prevention and health improvement.
Tier 1: Development of symptoms
Identifies those first level services provided to help people who are now developing symptoms of ill health. The purpose is to enable speedy access to an informed first point of contact, usually in primary care but including access out of hours. The aim is to facilitate accurate early diagnosis and appropriate management and to inform and support people to manage their condition with help from family, community and voluntary sector partners.
Tier 2: Established long term conditions with needs met fully in the community
This applies to the majority (70-80%) of people with long term conditions. The aim of Primary Care services, with community and voluntary sector partners, is to support people to manage their conditions and maintain their health and wellbeing. Maximising quality of life and independence at home may require additional support from outreach rehabilitation, diagnostic, social care and housing services.
Tier 3: Long term conditions mainly managed in the community but requiring specialist input
This reflects the needs of people supported by the primary care team but who require additional, usually intermittent, specialist support delivered mainly in the community or in Community Hospitals. There is a greater need for effective coordination across teams with multi-disciplinary and multi-agency working. It may be appropriate to consider introducing Anticipatory Care Planning and to explore carer support needs.
Tier 4: Frequent exacerbations and people with more complex care needs
This applies to people with serious acute conditions and/or exacerbations of long term conditions. Services need to be well coordinated with timely access to a range of professionals across care settings and agencies. As well as increased involvement of acute hospital services there is a need to deliver effective packages of care and equipment that proactively and continually support people with complex needs. This requires an integrated approach to planning, workforce development and care delivery as well as an effective use of telehealth and systems for information sharing.
Tier 5: End of life care
Coordinated multi-professional and multi-agency care that supports informed choice for the individual and those close to them. It is generally more appropriately delivered in community or hospice settings as opposed to an acute hospital.
An example of an integrated care pathway from NHS Lanarkshire
NHS Lanarkshire
Inequalities Targeted Case Finding
Through systematic targeted approaches to case finding, people who have long term conditions not yet identified on GP disease registers, or other related systems, can be identified and more effectively managed. This may include secondary prevention, pharmaceutical care, lifestyle advice and signposting to local supports for self management. At the same time those who do not yet have a long term condition but are at risk of developing one can benefit from primary prevention activity, lifestyle advice and supports for health behaviour change.
Ambulatory Care Sensitive Conditions
Ambulatory care sensitive conditions are illnesses, mainly long term conditions, for which hospitalisation is thought to be avoidable and where adequate care can safely be provided in primary care. This requires careful assessment and decision-making, supported by alternatives to bed based acute care for people whose illness severity does not or no longer requires an acute hospital bed. The NHS Institute for Innovation and Improvement developed a Directory of Ambulatory Care for Adults that identifies conditions that may be amenable to primary care provision and where efficiency and productivity gains and improved experience are possible through service redesign. There are essentially four groups to be considered:
1. Diagnosis exclusion - referral for the purpose of exclusion of a specific diagnosis. Individuals can be discharged with a zero length of stay.
2. Low-risk - people with conditions for which senior review with 'risk stratification' can enable early discharge.
3. Specific procedure - people who require a specific procedure or treatment.
4. Infrastructure required - people who can be managed as an outpatient with the appropriate infrastructure.
Long term conditions where effective ambulatory care can prevent flare-ups include asthma, COPD, diabetes and heart failure. These are the principle conditions that make up the current HEAT Target T6:
To achieve agreed reductions in the rate of hospital admissions and bed days of patients with a primary diagnosis of COPD, asthma, diabetes or CHD from 2006/07 baseline to 2010/2011.
Complexity through Multiple Morbidity or Inequalities
Where possible, we should design services that can support the needs of people with multiple morbidities. Many people will have additional social, psychological and economic factors that increase the complexity of their needs. This requires a fully integrated response across health, social care, housing, employment, benefits and voluntary sector partners. Health inequality remains one of our biggest challenges in Scotland. People living in the more deprived communities are likely to have greater complexity of needs and are more likely to be high users of health and social care services at a younger age. Poverty is also a risk factor for late presentation with long term conditions. Those most disadvantaged are least likely to be able to make best use of available health services and support for self management.
There is a problem
Thanks for your feedback