Telemedicine early medical abortion at home: evaluation
We commissioned this evaluation of early medical abortion at home (EMAH) in Scotland in 2021. The evaluation sought to determine the safety and efficacy of the current arrangements and help inform Ministers about the future of EMAH.
Findings
Work Package 1: Patient Safety
Public Health Scotland data showed that there were 4223 EMAH procedures carried out in Scotland during the six month pre COVID-19 period (October 2019-March 2020) and 11041 EMAH procedures in the 12 months following this (April 2020-March 2021).
In the pre-COVID-19 period, EMAH was used up to 10 weeks’ gestation. In the subsequent period EMAH was available until 12 weeks’ gestation. Only 3% of EMAH procedures in the period from April 2020-March 2021 were between 10 and 12 weeks’ gestation.
Public Health Scotland data showed that the total number of EMAH procedures conducted at the eight participating boards equated to 2374 EMAH procedures in the six-month period pre-COVID-19 (October 2019-March 2020), and 9031 abortions carried out over the 12-month period between April 2020-March 2021. Therefore the data reviewed covered the majority of EMAHs in Scotland during those time periods.
The effectiveness of EMAH was defined as complete abortion rate (i.e. excludes ongoing pregnancies and cases of incomplete abortion requiring surgical intervention). The complete abortion rate was high and was not significantly different between the two time periods; 98.5% pre COVID-19 and 98.8% in the subsequent period; P=0.34 (Table 1).
The rates of ongoing pregnancy, incomplete abortion requiring surgical evacuation, and retained products of conception with medical management were also low with no indication of potential differences between the time periods.
| Pre-COVID (Oct 2019-Mar 2020) (< 10 wks) |
Post-COVID Apr 2020-Mar 2021 (<12 wks) |
|
| Complete abortion |
98.5% |
98.8% |
| Ongoing pregnancy |
0.5% |
0.75% |
| Incomplete abortion |
1% |
0.5% |
| Retained products of conception managed with additional mifepristone and/or misoprostol |
0.5% |
0.5% |
As noted previously, the sample sizes make it difficult to draw firm conclusions in relation to any of the rare forms of complication considered. However, there was a low rate of haemorrhage in both time periods. There were no cases of severe infection requiring treatment with intravenous antibiotics in either time period (Table 2).
| Pre-COVID EMAH (< 10 wks) |
Post-COVID EMAH (<12 wks) |
|
| Haemorrhage of > 1 litre or requiring a blood transfusion |
0.3% |
0.2% |
| Severe infection requiring intravenous antibiotics |
0 |
0 |
The adverse outcomes of particular interest in this evaluation, were ectopic pregnancy diagnosed after treatment had been commenced and inadvertent treatment at a gestation above the Scottish clinical guidelines for EMAH at that time period. This is because in the pre-COVID-19 period, all patients had a routine ultrasound, but, in the subsequent 12 month period, ultrasound was used selectively in most Health Boards where clinically indicated, such as for those at high risk of ectopic pregnancy, or with pain, bleeding, or other significant risk factors. It continued to be used routinely only by a small number of Health Boards.
In the six month pre-COVID period there were no cases of inadvertent treatment above 10 weeks of pregnancy. In the longer 12 month post-COVID-19 period, there were a very small number of cases where EMAH medication was taken by someone at or above 12 weeks gestation but under 20 weeks (Table 3).
Ectopic pregnancies were rare both before and after the changes in practice. Even though numbers were insufficient to test difference, there were no marked observable changes that suggest a concern about any change in risk. Ectopic pregnancies occurred even when ultrasound was routine in all cases[17]. In addition, some of the cases of pregnancy of unknown location or ectopic pregnancy diagnosed following the changes in practice did have an ultrasound before receiving abortion medication, but the ultrasound did not detect the ectopic pregnancy.
| Pre-COVID EMAH (< 10 wks) |
Post-COVID EMAH (<12 wks) |
|
| Ectopic pregnancy diagnosed after starting treatment |
0.04% |
0.1% |
| Inadvertent treatment at higher gestation* |
0 |
0.03% |
*inadvertent treatment >10 weeks if pre-COVID-19, or >12 weeks in subsequent period.
Health Boards also reported on admissions to hospital for pain, admissions for other concerns related to abortion within 24 hours and from 24 hours to six weeks. The rates of admission for any cause were low in both time periods (Table 4).
| Pre-Covid EMAH (< 10 wks) |
Post-Covid EMAH (<12 wks) |
|
| Admission/attendance within 24 hours of misoprostol |
0.2% |
0.2% |
| Admission/hospital attendance within 24 hours to 6 weeks after EMAH |
1.7% |
1.4% |
| Admission for pain management |
0.1% |
0.1% |
| Total |
2.0% |
1.6% |
Work Package 2: Mapping clinical abortion care pathways
The finalised maps were produced to contextualise the data collected in other work packages within this report. It was not possible to gather sufficient information from NHS Highland to include details on their EMAH pathway in this report. Patients from NHS Western Isles and NHS Shetland receive abortion care from larger neighbouring Health Boards (NHS Greater Glasgow and Clyde, NHS Grampian, and NHS Highland) and so some of the processes outlined below are carried out by these other Health Boards.
Referral processes
All Health Boards gave patients the option of self-referring to abortion services. These referrals were processed by administrative staff in the majority of Health Boards and by nursing staff in the remaining boards.
Advance provision of information
All but one of the Health Boards made information about abortion available in advance of the pre-abortion consultation. Most commonly, this was by directing patients to the clinic website for information. Some Health Boards also sent text messages or emails with links to further information.
Clinic timings
Two thirds of Health Boards had abortion clinics running on four days per week or more. Nine Health Boards had clinics at variable times during the day, with one health board offering evening appointments.
Types of consultations offered
All Health Boards except one offered consultation by telephone with some boards offering a choice of telephone or in-person appointments. No Health Boards routinely offered video consultation, although some stated that they could offer this if requested by a patient.
Safeguarding processes
All Health Boards had safeguarding processes embedded into abortion services that included routine questions on safeguarding at the pre-abortion consultation, whether that was in-person or remote consultations. All Health Boards offered staff training to identify safeguarding issues. Some Health Boards used tools to aid assessment of safeguarding issues, for example the ‘West of Scotland Child Sexual Exploitation Screening Tool’, structured questions as part of routine enquiry, or a ‘safe word’ to alert clinicians to arrange an in-person appointment if used during a consultation.
Systems used for delivering care
There was variation across boards in the use of IT (Information Technology) systems for delivering abortion care. Most Health Boards used more than one IT system along with paper records and paper prescriptions.
Pre-abortion investigations
Two Health Boards performed pre-abortion ultrasound scans on all patients to confirm the stage of pregnancy. The remaining Health Boards conducted ultrasound selectively and on clinical indications according to clinical guidelines. The leads of abortion services in the Health Boards performing selective ultrasound estimated that a pre-abortion ultrasound was conducted in between one-third to two-thirds of patients. In addition, all Health Boards carried out other investigations based on clinical need rather than routinely. In most boards, testing for blood-borne viruses and sexually transmitted infections were conducted following risk assessment.
Types of abortion provided
All Health Boards provided the option of EMAH. All Health Boards except for one also provided the option of medical abortion in hospital. Ten Health Boards provided surgical abortion. One Health Board reported willingness to provide surgical abortion, but indicated that since COVID-19, they no longer had access to theatre space to perform these.
Gestations for abortion care
All but four Health Boards provided EMAH up to 12 weeks, as recommended by national guidelines. Most Health Boards had a maximum gestation for providing abortion of 19 weeks and 6 days. Two Health Boards provided abortions to higher gestations (21 weeks and 21 weeks and 6 days). Two Health Boards (small island boards) provided to an earlier gestation.
Access to abortion medications
All Health Boards offered collection of medications for EMAH from a healthcare facility (clinic or hospital). One Health Board offered collection from a designated community pharmacy. Five Health Boards used the option of posting medications, four of which indicated that most patients preferred to collect medications rather than receive them by post.
Location of mifepristone administration
All but one Health Board gave patients the option of choosing to administer mifepristone at home or in the clinic and said that most patients selected the home option. One Health Board indicated that most patients took mifepristone in clinic and another board indicated that around one half of patients took it in the clinic. These were both smaller Health Boards.
Following abortion
All but one Health Board provided patients with a recommended urine pregnancy test to confirm the success of EMAH. All Health Boards had a follow-up route for patients to access aftercare where required. Just over half of Health Boards stated that they conducted routine audit of abortion outcomes in their service.
Contraception
Most Health Boards included the offer of supplies of contraception in the medication packs for patients having EMAH. This was usually the progestogen-only pill; however some boards offered combined hormonal contraception and one board included supplies of the self-injectable contraceptive in this pack, where patients requested this method. All but one Health Board offered rapid access to a clinic for insertion of subdermal implants or intrauterine devices.
Examples of good practice for EMAH
Whilst most Health Boards provided EMAH (Table 5), the large, predominantly urban boards were able to provide consultations on most weekdays and offered EMAH up 12 weeks of pregnancy in line with what is permitted under national guidelines. Other examples of innovative practice were from Health Boards who offered a postal service for abortion medications to those living in remote and rural areas and outside their own board areas (NHS Greater Glasgow and Clyde, Tayside and Grampian).
| Health Board |
Self Referral |
Advance Information |
Telemedicine available |
Safeguarding processes |
Ultrasound |
|
| Clinical reason |
All |
|||||
| A & A |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
| Borders |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
| D & G |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
| Fife |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
| Forth Valley |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
| GG & C |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
| Grampian |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
| Lanarkshire |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
| Lothian |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
| Orkney |
Yes |
No |
No |
Yes |
No |
Yes |
| Shetland |
Yes |
Yes |
Yes |
Yes |
No |
Yes |
| Tayside |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
| Western Isles |
Yes |
Care delivered by other Health Boards |
||||
A&A = Ayrshire and Arran; D&G = Dumfries and Galloway; GG&C = Greater Glasgow and Clyde
Work Package 3: Patient experiences of abortion care
A total of 327 questionnaires were completed and analysed. Although patients had the option of completing the questionnaire via telephone rather than online, no one chose the telephone option, and all completed the questionnaire electronically.
Demographics
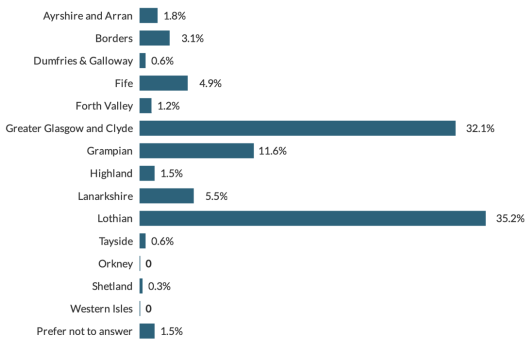
Over two thirds of respondents were from the largest Health Board areas of NHS Greater Glasgow and Clyde and NHS Lothian. No survey responses were obtained from Orkney or Western Isles. (Figure 1)
Respondents were all 16 years or older and the most common age category was 25-29 years (28% of responses). One half of all respondents had been educated to university level. Almost all (99%) identified as female and as women. In terms of ethnicity, 89% identified as White/White Scottish/White British ethnicity. This was followed by 4% as Black/African/Caribbean/Black Scottish/Black British. The next most common category (3%) Asian/Scottish Asian or British Asian. The remainder were of mixed ethnicity, or other ethnic groups. Ten respondents (3%) indicated that they had a disability and these were all in the mental health category.
154 respondents provided partial postcode information, which allowed the postcode sector to be determined. We calculated the proportion of postcodes in these sectors that belonged to the 20% most deprived postcodes (also known as Scottish Index of Multiple Deprivation, SIMD, quintile 1, see Scottish Index of Multiple Deprivation 2020).
44% lived in an area where none of the postcodes were in SIMD quintile 1, 11% lived in an area where more than half of the postcodes were in SIMD quintile 1 and the remaining 45% lived in an area where less than half of the postcodes were in SIMD quintile 1.
Pre-abortion consultation
A total of 284 respondents (87%) stated that they had all or some of the pre-abortion consultation by telephone with the remaining 13% having exclusively in-person consultations at a clinic. In 30% of cases involving a telephone consultation, the respondent had an initial phone call, but then also needed to make an in-person visit. No respondents had their consultation via video call.
Of those who had some or all of the consultation by telephone, 93% felt that they could talk privately without risk of being overhead and 5% indicated that they could not. The remainder either felt they could not talk privately but that privacy was not important to them, or chose not to answer this question.
Respondents were asked to rate how satisfied they were with having their consultation in this way (telephone or in-person, or a mix of both); on a five point scale from ‘very satisfied’ to ‘very dissatisfied’. The most common response was ‘very satisfied’ (79%), followed by ‘fairly satisfied’ (13%), ‘neutral’ (5%) and ‘slightly dissatisfied’ (3%). Only 0.3% were ‘very dissatisfied’.
94% of respondents agreed that they were given enough information (online, written and/or verbal) about the abortion and any potential side-effects. Over three quarters of respondents (78%) felt they had enough time and opportunities during the consultation to discuss any uncertainty or how they were feeling about having an abortion, but 5% felt they did not have enough time. A further 15% indicated that whilst they did not have time/opportunities to discuss this, they did not feel they needed to discuss this.
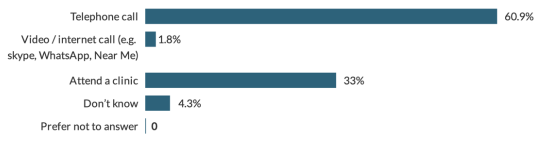
When asked which type of consultation they would have chosen if given the choice, the most common response (over 60% of respondents) was ‘telephone consultation’ (Figure 2).
Pre-abortion ultrasound scan
Just over half (56%) of all respondents had a pre-abortion ultrasound. Of this group, two thirds agreed that they were fine about having an ultrasound before they could start treatment, but 19 respondents (11%) stated that they would have preferred not to have ultrasound.
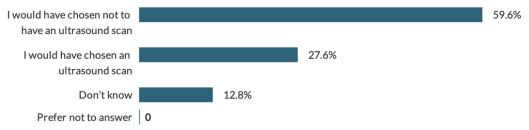
Of the 156 who did not have ultrasound, 60% stated that if given the choice, they would have chosen not to have ultrasound and 28% would choose an ultrasound (Figure 3).
Medical abortion pills at home
85% of respondents took both mifepristone and misoprostol at home. The remainder took mifepristone in a clinical setting followed by misoprostol at home.
94% of respondents collected the medications from a clinic, others had them delivered by courier (4%), and the remainder by delivered by post or collected from a pharmacy. When medications were delivered by courier they arrived same day or next day.
Wider sexual and reproductive healthcare
98% of respondents indicated that at the pre-abortion consultation they were offered a discussion on contraception and 84% were also offered supplies of contraception in their medication pack.
In 70% of cases, respondents recalled that they were offered a test for sexually transmitted infections such as a swab to take home or a test at a clinic. A further 21% indicated that they did not want testing for sexual infections. 6% stated that they were not offered testing, but would have liked to have been offered.
71% of all respondents stated that they had been questioned about gender-based violence at the pre-abortion consultation, 20% had not and 9% were unsure.
Continuation of current arrangements for medical abortion at home
When asked ‘Do you think that patients should continue to be offered the option of having a telephone/video/internet consultation for abortion?’ 92% were in favour, 4% were not in favour and 5% answered ‘don’t know’.
97% responded ‘Yes’ to the question: ‘Do you think women who are eligible for an abortion at home should continue to be offered the option of taking both pills for medical abortion (mifepristone and misoprostol) at home?’ 2% stated ‘don’t know’ and 1% stated ‘no’.
87% of respondents supported continuation of the option to deliver or post abortion medications. 92% also supported continuation of the option to collect abortion medications from a community pharmacy. 5% were not supportive and 3% indicated ‘don’t know’.
Patients were also asked about their overall satisfaction with their abortion care. In response to the question ‘Overall, how satisfied were you with the care you received from the clinic before, during and after the abortion?’, most (92%) indicated satisfaction. Specifically, 83% were very satisfied, 9% slightly satisfied, 5.5.% neutral, 2.4% slightly dissatisfied and 0.3% very dissatisfied.
Free text comments
A total of 155 respondents made free text comments. Some made more than one point, giving a total of 206 discrete comments. These 206 comments were categorised by the research team as positive (68%) or negative (32%) and were grouped into themes. Many of these comments were general comments about the abortion service and so not directly relevant to the questions covered by this evaluation, but they still provided useful feedback. The most common theme, which is relevant to this evaluation, was ‘praise for aspects of the EMAH service’ (38%). Many of these comments indicated support for continuation of the current models of service delivery, noting a range of benefits including convenience, privacy, comfort and flexibility. The second most common theme - also from within the ‘positive’ category - was ‘expressions of thanks to staff’ for care received at abortion services (30%). In these comments, respondents reported gratitude towards staff for their kindness, non-judgmental and caring approach.
Negative comments were less common. 12% of comments were critical of aspects of the service including: the appropriateness of the procedure within the home setting, the location of clinics (and their being insufficiently close to home), and perceived negative attitudes of staff. Another 10% of respondents commented on the procedure and noted that their experience of bleeding and/or pain was worse than they had expected. 6% of comments indicated a preference for more follow up to be available following abortion. 3% commented that intimidation by anti-abortion protestors/vigils outside the clinic had negatively impacted their experience of accessing abortion. One comment (0.5%) cited limited availability of contraception.
Work Package 4: Staff perspectives on provision of abortion care
Findings from the ENHANCES study will be reported and published in peer-reviewed journals in due course. The main findings related to the research questions for this evaluation are outlined below.
Key benefits of changes to provision of EMAH
A key benefit of the ‘new’ model of EMAH articulated by staff was that it enabled treatment and care to be provided ‘at the right time, in the right place’. Staff noted this was critical during the COVID-19 pandemic when access to clinics and hospitals was limited. However, enduring benefits of the EMAH model for patients accessing abortion were also highlighted, including:
- enabling timely access to abortion care
- overcoming geographic barriers to (timely) care
- reducing the need for travel
- reducing need for multiple appointments and associated time and travel costs
- enhancing patients’ control and autonomy over the abortion process
- These dimensions of the new model were understood by participants to enhance patient-centred care.
Telemedicine for EMAH was described as particularly important in rural and remote areas (“a lifeline for rural services”) because it enabled staff to provide high-quality care via phone/video, even when in a different geographic location. For patients living in remote island communities, telemedicine also helped address issues around privacy and ‘visibility’ for those who did not want to disclose their abortion.
“[in rural and remote locations] the chances of you coming across a relative or somebody that you know are huge – it’s high, very high. And the confidentiality of this process…or even early pregnancy process in itself, trying to keep a pregnancy within cover, you know, to allow the woman the privilege to release that information to people that she wants to know.”
(P10, Nurse)
Telemedicine provision of abortion care was valued by staff because it has enabled timely provision of care in the context of ongoing workforce pressures across NHS Health Board areas. From a practical perspective, it was noted that it offered increased flexibility in managing staffing within services. For example, telemedicine consultations offer flexibility when managing staff absence (within and across Health Boards) by enabling staff to contact patients in various geographic locations.
“COVID has really shown up how fragile various parts of healthcare systems can be. And we’ve ended up with situations where suddenly staff haven’t been able to work because they were shielding for long periods of time or because they were self-isolating. Being able to provide telemedicine has been really helpful from that point of view.”
(P2, Consultant)
Telemedicine consultations also enable services to manage ‘demand’ for consultations by, where possible, scheduling additional ‘telephone clinics’. Although the widespread adoption of EMAH provision via telemedicine was seen as broadly positive, staff noted that EMAH should not be understood as ‘optimal care’ for all patients, especially where home circumstances may not be conducive to EMAH. In such cases, staff voiced a commitment to supporting patients to access the form of abortion care best suited to their needs.
“[the service aims to] make it easy for people to access us and also that there’s some choice in that. So if somebody does want to come in and see us face-to-face, or after a chat on the phone says no, I’d rather just come in and see somebody, that we’ve got that ability to do that and it’s not just one pathway or one size fits all.”
(P13, Consultant)
There was widespread agreement across staff from all professional groups that reverting to former (pre-COVID-19) models of care (in-person consultation, ultrasound for all and administration of mifepristone on clinical premises) would reduce flexibility in service delivery and increase waiting times and delays to treatment and care.
“I think it would just be disastrous, to be honest, if we were to go back [to previous models of EMAH]. Because along with COVID, access to contraception just fell. So abortion rates have gone up a little bit but the access to contraception’s gone down. I don’t know we would manage our capacity […] I think people would be having to wait longer, abortions would be happening at a later gestation, they wouldn’t be happening earlier.”
(P9, Consultant)
This would be likely to lead to more abortions at later gestations, increased demand for medical and surgical abortion in hospital settings and greater costs to NHS services. Staff also expressed concern that for patients, reverting to former models of care would also mean more appointments, more time for appointments (away from work, challenges in managing childcare, etc.), increased requirement to travel (with time and cost implications) all of which reduce access and convenience of care for patients.
Variations among and within boards in telemedicine EMAH service delivery
The COVID-19 pandemic required rapid changes to abortion processes and models of care including:
- remote consultations
- abortion medications being delivered at home
- ultrasound scanning only where clinically indicatedimplementation of revised protocols and screening processes
The mapping and analysis of clinical abortion care pathways (WP2) identified variations in elements of telemedicine services across NHS Health Board areas. This was reflected in staff interview accounts. Staff at senior levels acknowledged variations in the implementation and provision of care across Scotland linked to several issues, including:
- challenges around workforce
- service demand and capacity
- funding
- location of the service (geography, community or hospital-based) and
- effects of non-participation in abortion care by some staff (in some cases described as ‘conscientious obstruction’)
For example, staff reported that many NHS abortion services have, and continue to, experience intense workforce pressures related to issues such as the ongoing effects of the COVID-19 pandemic; staff sickness and ‘burnout’; and staff leaving NHS. Increased demand for abortion care, without a concomitant increase in workforce and other resources, was also reported.
Staff commented on the ways in which the location of services could pose specific challenges. One way in which this manifest was through competing priorities and demands across services. For example, within abortion services located in community sexual and reproductive health settings, there are demands for provision of other clinics beyond abortion, such as access to effective contraception, testing for sexually transmitted infections (STI) and other specialist services. In hospital-based services, staff described a necessary focus on obstetric and gynaecological emergencies, and competing demands for surgical beds for cancer treatment.
Changes to EMAH service provision were described as easier for services with strong medical leadership, and for larger Health Boards that were (and are) better resourced in terms of staffing. In large, research-active abortion services, implementation was supported by experience from ongoing research, and some staff noted that this made it easier for these services to rapidly pivot to new model(s) of care.
Some smaller board areas, including those where services are predominantly nurse-led, experienced challenges due to lack of strong medical back-up and ‘championing’ of abortion care. Some staff noted challenges for services where there has historically been a lack of visible (senior) support for abortion care, and in areas where there are high levels of staff non-participation in abortion care. Nevertheless, ‘smaller’ boards adopted innovative, collaborative approaches to enable the continued delivery of abortion care. For example, staff described strong inter-organisational working and relationships between NHS Health Boards and key individuals, including support from clinical leaders in larger boards and the sharing of protocols and examples of best practice.
“…we’ve adapted a lot of [name of large Health Board service] information. They kindly shared their resources and things with us. So, we’ve been able to sort of model a lot of our paperwork and things for governance on them. I think the fact that these places have been up and running and it’s been successful has allayed some of the fears.”
(P12, Specialist Trainee)
Although evidence for the safety and effectiveness of telemedicine delivery of abortion care (delivered in line with clinical guidelines) was acknowledged, some participants noted that concerns circulating among staff about adverse outcomes, such as late diagnosis of an ectopic pregnancy or inadvertent treatment at a later gestation, served as a barrier to consistent implementation of telemedicine care, in particular the use of selective, rather than routine use of ultrasound. This most obviously manifested in differential ‘appetites for risk’ in relation to selective rather than routine use of ultrasound.
Although staff reported the rigorous application of clinical guidance when assessing the need for ultrasound scanning, and as part of safeguarding assessments (see process maps developed as part of WP2 for overview of safeguarding processes and pre-abortion clinical investigations undertaken in different Health Board areas), they noted that concerns and anxieties amongst staff, particularly during the transition to ‘new’ models of care (at the start of the COVID-19 pandemic), posed challenges to the implementation of telemedicine care.
In line with previous research in Scotland, staff reported that as telemedicine provision became an established way of working, confidence in clinical protocols (to minimise risks) increased and they became less anxious about selective use of ultrasound. Staff accounts suggested that this worked most effectively in services where there were clear pathways in place for seeking medical support and advice from senior leadership (nursing and medical).
Similarly, staff reported that any initial concerns they had about their (and colleagues’) ability to identify safeguarding issues, including coercive control and domestic violence, because of the absence of visual cues during telemedicine consultations, diminished over time and that assessment tools for identifying safeguarding issues had been refined over time. Furthermore, staff described that as new EMAH models became established, confidence in their ability to pick up non-verbal cues developed, enhancing their ability to identify safeguarding issues.
“…all of our staff are well trained at picking up the sort of, I suppose, non-verbal cues […] There are lots of things that you can pick up without actually seeing, and I think we’ve probably all learned that from all our different types of consultations.
(P14, Consultant)
Staff also emphasised that provision of ‘safe abortion care’ extends beyond evidence-based clinical care (and mitigation of risks) and encompasses issues such as: addressing abortion stigma at multiple levels, enhancing opportunities for training and shared learning, and extending research, audit and evaluation. It also requires continued commitment to maintaining, and extending, access to legal abortion and addressing barriers to access including the implementation of buffer zones. Staff described such endeavours as contributing to safe abortion care by reducing barriers to access, enhancing patient-centred care and improving patient experience, all of which were understood to improved the quality and safety of abortion care.
Leadership and ‘abortion care champions’
The importance of medical leadership was consistently highlighted by abortion care providers. Support from medical leaders enhanced staff confidence in protocols to ensure safety, and helped increase staff confidence in following key clinical guidance and conducting assessments (including selective ultrasound and safeguarding) during telephone consultations.
Strong clinical leadership (including abortion care champions) and support was understood by staff as critical for sustainable provision of high-quality, equitable care across Scotland. The importance of ongoing training and support for future generations of abortion care providers (across all professional groups - doctors, nurses, and midwives) was highlighted by staff across professional groups.
Staff identified the value of ‘champions’ of abortion care. ‘Champions’ were described as key staff who advance and support abortion services at both ‘strategic’ and ‘local’ levels. Examples of leadership and ‘championing’ of abortion care were cited across professional groups, not only at consultant or service lead level. For example, staff described the importance of consultants and service leads who visibly advocate for resources to support high-quality service provision at a ‘local’ level (within Health Boards), and improvements to equitable provision of care at a strategic level. Examples were also highlighted of nurses and midwives ‘championing’ local service improvements, such as increased availbility of community ultrasound scanning (where required).
Enhancing support and training, and nurturing future abortion care champions, across professional groups was described as important in enabling innovation in future abortion care provision.
Sharing lessons learned and future opportunities
Staff highlighted that lessons have been learned and expertise shared between NHS abortion services, such as sharing of telemedicine and safeguarding protocols. Services that have limited capacity for research have benefited from the expertise of research-active services in other Health Boards, through enhanced refinement of protocols over time.
The Scottish Abortion Care Providers (SACP) Network was described as an important mechanism for advancing high-quality abortion care in Scotland through the development of guidelines, opportunities for collaborative research, and peer support. Staff highlighted the importance of bi-directional learning between services providing care in urban and rural areas, and opportunities to strengthen and advance learning across varied service contexts. For example, staff described the value of training visits to other services to learn from good practice.
“Us going to see how their service runs […] I’ve already worked in [name of large abortion services] see what their setup is like, because when you’re setting up a service you think, I wonder if I’ve got this right, what else could I do […] Because you do feel vulnerable if you’re just doing it on your own, but you need these people to support you.”
(P10, Nurse)
Some nursing and midwifery staff voiced a desire for increased opportunities for inter-board/service learning and peer support, especially where there is limited intra-board/service support. For example, staff articulated the value of sharing learning at the (formerly) annual SACP Network Conference and intra-board training events. Such learning was emphasised as being important in managing experiences of professional stigmatisation linked to involvement in the delivery of abortion care.
The value of drawing on patient experience to inform service delivery and improvement was emphasised by staff across professional groups. Staff highlighted both formal (research and evaluation, patient engagement and involvement) and informal (‘in the moment’ patient feedback) mechanisms to support service improvement and redesign.
“I think we’ve got to listen to the service users […] our job is to work, you know, within evidence-based practice and within the guidelines. Over and above that, we should listen to the service users as much as possible about how they think we could make this not really difficult for them”.
(P1, Nurse)
Contact
Email: abortionteam@gov.scot
There is a problem
Thanks for your feedback