Type 2 Diabetes - framework for prevention, early detection and intervention: evaluation
Findings of a qualitative process evaluation of the implementation of the framework for the Prevention, Early Detection and Intervention of Type 2 Diabetes in three early adopter areas.
1. Introduction and context
This report presents the findings from a qualitative process evaluation of the implementation of the framework for the prevention, early detection, and early intervention of type 2 diabetes in three early adopter areas.
1.1 Introduction
The Scottish Diabetes Survey[4] 2020, shows that, in Scotland, 317,128 people diagnosed with diabetes were recorded on local diabetes registers at the end of 2020. This represents 5.8% of the population. When considering the type of diabetes:
- 10.7% (34,087) of all registered people were recorded as having type 1 diabetes
- 87.7% (278,239) of all people registered with diabetes were recorded as having type 2 diabetes
- 1.5% (4,802) of all people registered with diabetes were recorded as having other types of diabetes, for example pre-diabetes, gestational diabetes.
The incidence and prevalence of all types of diabetes has been steadily growing in Scotland, as in many other countries, in part due to better care and better detection. For type 2 diabetes, this has also been in part due to unhealthy diet, low levels of physical activity and an increase in levels of obesity. Excess weight is a modifiable risk factor for type 2 diabetes.
The evidence about preventing or delaying the diagnosis of type 2 diabetes (or promoting remission) through targeted weight management interventions,[5] and the cost to the NHS budget for the treatment of people with type 2 diabetes, helped to inform the decision and policy to address the avoidable risks associated with weight and type 2 diabetes.
1.2 A Healthier Future – Framework for the Prevention, Early Detection and Early Intervention of type 2 diabetes
A Healthier Future: type 2 Diabetes prevention, early detection and intervention: framework - gov.scot (www.gov.scot) (known throughout this report as the "Framework") was produced in collaboration with specialists in diabetes, dietetics, maternal health, public health, primary care and obesity. It builds on the prevention work within the Diabetes Improvement Plan[6] (DIP) and is designed to provide guidance to Integration Joint Boards (IJBs), NHS boards and Community Planning Partners (CPPs), and other delivery partners on the implementation of a specific weight management pathway for those at risk or those diagnosed with type 2 diabetes.
The Framework sets out the pathway, which sits within wider national policy, 'A Healthier Future – Scotland's Diet and Healthy Weight Delivery Plan (2018)' aimed at tackling high levels of overweight and obesity. The Framework details:
- the approach to prevention, early detection, and early intervention for type 2 diabetes (action to reduce health inequalities, collective leadership and partnership, co-production, person-centred approach and value-based care and being sensitive to stigma and discrimination)
- the actions that would be taken at a national level in terms of the awareness campaign, targeted core messages, and the resources that would be developed to ensure consistency in weight management and lifestyle interventions
- the actions at a local level to promote understanding of the risk levels amongst individuals, the development of pathways of care, psychological support, and a comprehensive tiered approach to weight management programmes.
Implementation of the Framework
For the first year of implementation, three early adopter areas were approached and supported by a professional advisor - registered dietitians seconded to Scottish Government to support NHS boards and lead the implementation of the Framework. This included building the necessary strategic and operational partnerships and service re-design. Given the ambitious overhaul of services recommended by the Framework, a co-production approach to implementation was taken in the first year, creating opportunities for early adopter health boards to identify and tackle practical and systemic barriers.The intention was that the learning from the early adopter areas during their first year of implementation would be shared with the remaining IJBs and NHS boards throughout the year to help inform the wider roll-out.
The roll-out to other areas was to be staggered over five years in order to facilitate effective implementation and create opportunities for improvement.
Early adopter areas
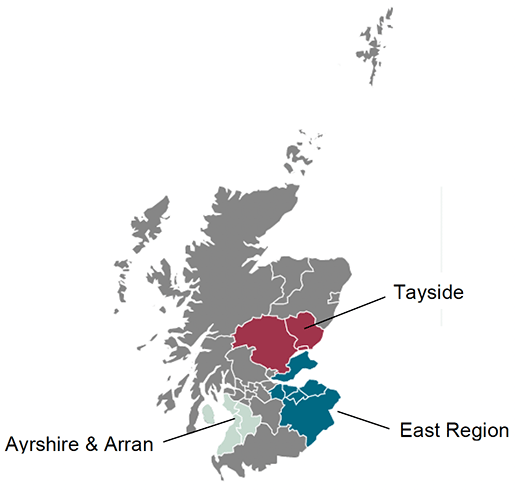
The three early adopter areas were NHS Ayrshire & Arran, NHS Tayside, and the East Region (a partnership between NHS Lothian, NHS Fife and NHS Borders). They agreed, with additional support from Scottish Government funding and the professional advisors, to begin work to redesign and deliver services in line with the Framework. The early adopters were selected according to their readiness to re-design and deliver services in line with the national guidance and to represent a broad selection of population demographics and geography. More detail on early adopter sites is presented in Chapter 3.
Monitoring the Framework
An Evaluation Advisory Group (EAG) was convened to co-produce a monitoring and evaluation framework in collaboration with the early adopter areas. Short, medium and long-term outcomes within a logic model were agreed to help understand the impact of the implementation of the Framework. These helped to identify a series of measurable indicators of success and appropriate data sources. As part of the workshops, the EAG also identified a set of research questions, detailed in appendix 1.
The evaluation was to take place in two stages. As part of the first stage, a qualitative process evaluation was to be carried out after the first 12 months post-implementation (Sep 2018 to Sep 2019). This aimed to identify barriers and enablers in the implementation of the Framework in early adopter areas. It was to run in parallel with, and complement, the development of national monitoring of patient outcomes, the core dataset.
The second stage will be a light-touch outcome evaluation to be carried out over a five-year period, post-implementation, in order to establish whether the Framework is achieving its aim of improving population health by reducing the incidence of type 2 diabetes associated with overweight and obesity.
1.3 Purpose of this report
In November 2019, the Scottish Government commissioned Blake Stevenson to carry out an independent qualitative process evaluation of the adoption and implementation of the type 2 diabetes prevention framework in the three early adopter areas. This was to contribute to the first part of the evaluation work alongside the national monitoring of patient outcomes through the core dataset.
Delays associated with the requirement for Public Benefit and Privacy Panel (PBPP) approval and the COVID-19 pandemic meant that information gathering started in January 2021, more than a year after the evaluation was commissioned. During this time the Framework has been rolled out to more areas. This report has been written in year four (2021/22) and to date 14 territorial NHS boards and one special NHS board have implemented the Framework. Although delayed, learning presented within this report provides valuable insights for those areas in the process of implementing the Framework, and more broadly for the roll out of other healthcare frameworks or policy that need to be implemented at a health board or partnership level.
Contact
There is a problem
Thanks for your feedback