The Scottish Health Survey 2022 – volume 1: main report
This report presents results for the Scottish Health Survey 2022, providing information on the health and factors relating to health of people living in Scotland.
This document is part of a collection
3 Respiratory
Prevalence of doctor-diagnosed asthma has ranged from 13% to 17% since 2003, and has remained between 16% and 17% since 2017.
- 2003: 13%
- 2008: 13%
- 2010: 14%
- 2012: 16%
- 2013: 16%
- 2014: 17%
- 2015: 17%
- 2016: 15%
- 2017: 16%
- 2018: 17%
- 2019: 16%
- 2021: 16%
- 2022: 17%
A higher prevalence of doctor-diagnosed asthma was recorded among children aged 8-15 compared with those aged 0-7:
- 0-7 years: 6%
- 8-15 years: 13%
Among those aged 25-34, just over a fifth of women reported having wheezed in the last 12 months, a higher proportion than among men in the same age group.
- Women 25-34: 22%
- Men 25-34: 11%
In 2022, the proportion of adults who reported having wheezed in the last 12 months decreased from
- Most deprived: 23%
- 2th: 20%
- 3rd: 16%
- 4nd: 14%
- Least deprived: 12%
Adults who smoked 20 or more cigarettes a day were more likely to report having wheezed in the past 12 months than non/occasional smokers.
- Smokers: 40%
- Non-smokers: 12%
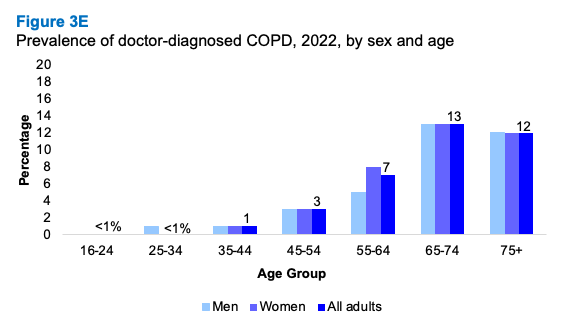
Prevalence of doctor-diagnosed Chronic Obstructive Pulmonary Disease (COPD) increased with age, from:
- <1% of those aged 16-44 years
- 12-13% of those aged >65 years
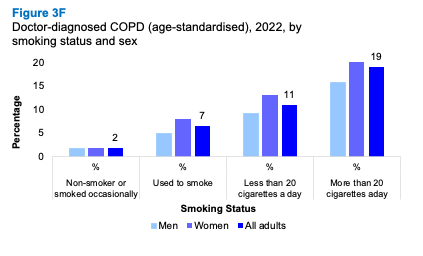
In 2022, prevalence of doctor-diagnosed COPD varied as follows:
- 2% of adults who had never smoked or had smoked occasionally
- 7% of adults who had smoked previously
- 11% of current smokers (<20 cigarettes per day)
- 19% current smokers of 20 or more cigarettes per day
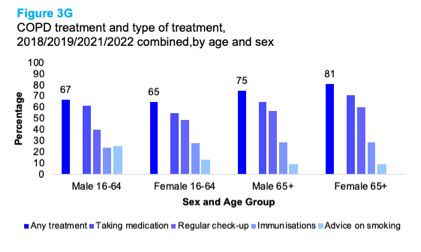
In 2018/19/21/22 combined, the most common forms of treatment received by all adults for a COPD were:
- Medication: 64%
- Regular check-ups: 53%
- Immunisations: 28%
In 2022, 13% of adults reported that they ever had long COVID[68], while prevalence among children was 4%. Those aged 45-54 were most likely to report having ever had long COVID (19%).
- 0-15: 4%
- 16-24: 9%
- 25-34: 10%
- 35-44: 14%
- 45-54: 19%
- 55-64: 16%
- 65-74: 10%
- 75+: 7%
Elena Maiolani
3.1 Introduction
Infectious respiratory disorders and long-term respiratory conditions, such as asthma and chronic obstructive pulmonary disease (COPD), are a considerable challenge for the individuals that live with them and for health services in Scotland, particularly in light of an ageing population and the ongoing impact of the Covid-19 pandemic on healthcare services [66]. These respiratory conditions are currently incurable, however, treatment can help to improve symptoms and quality of life[67].
The UK has one of the highest rates of asthma in the world[68], with an estimated £500 million spent by the NHS in Scotland each year on this and other respiratory diseases[69]. This long-term condition is characterised by variable and recurring symptoms of breathlessness, wheezing, coughing and chest tightness. The reasons for the high prevalence of asthma in the UK are not certain; however, risk factors include infections/viruses, hormones, environmental, lifestyle (inc. diet and obesity), occupational and genetic disposition[70],[71],[72].
COPD continues to be the third leading cause of mortality worldwide[73]. The ageing population, along with the additional complication of older COPD patients being more likely to have other long-term conditions, presents a further challenge in managing COPD in Scotland[74]. The associations of long-term conditions like COPD with deprivation, lifestyle risk factors and wider social health determinants persist in Scotland[75]. Smoking is the main cause of COPD with an estimated 8 in 10 of those with the condition in the UK having either smoked or continuing to smoke[76]. Exposure to smoke is associated with a higher risk for women compared to men[77].
Long COVID, or post-COVID-19 syndrome, refers to symptoms that develop during or after a COVID-19 infection that continue for 4 weeks or more and are not attributed to another condition/diagnosis. The overlapping long COVID symptoms that are sometimes experienced can affect body systems including the respiratory system[78]. Recent evidence suggests that a sizeable proportion of people who report to have long COVID have long-term rehabilitation and support needs[66].
3.1.1 Policy background
The Respiratory care – action plan: 2021 to 2026[79] sets out the vision for improvement in the prevention, diagnosis, care, treatment and support of people living with respiratory conditions in Scotland. This is supported by other key policy initiatives including the Special Delivery Group within the Centre for Sustainable Delivery[80], which aims to improve patient journeys through sustainable changes that facilitate person-centred care and the Framework for supporting people through Recovery and Rehabilitation during and after the COVID-19 Pandemic[81].
One of the Scottish Government’s National Performance Framework National Outcomes[82] is for people in Scotland to ‘live longer, healthier lives’, which includes a National Performance Indicator to ‘reduce premature mortality’ (deaths from all causes in those aged under 75). Within the Scottish Government National Indicators, health risk behaviours linked to respiratory disease, including smoking, harmful drinking, low physical activity and obesity, are monitored against an outcome of reducing the percentage of adults exhibiting two or more of these behaviours[83].
In September 2021, the Scottish Government published Scotland’s Long COVID-19 Service[84] paper. The paper sets out four key elements that underpin the approach to care and support for people with long COVID: supported self-management, primary and community-based support, rehabilitation support and secondary care investigation and support.
The Scottish Government has established a £10 million long COVID Support Fund to support NHS Boards and partners increase the capacity of existing services providing support to people with long COVID, develop these into more clearly defined pathways and to provide a more co-ordinated experience for those accessing support[85].
In addition, a long COVID Strategic Network has been established and brings together clinical experts, NHS Boards, third sector organisations and those with lived experience to guide, plan and design the ongoing care for people living with long COVID[86].
3.1.2 Reporting on respiratory conditions including COVID-19 in the Scottish Health Survey
This chapter updates trend data on self-reported doctor-diagnosed asthma respiratory symptoms (wheezing) for adults and children, as well as data for 2022 for adults by area deprivation and by smoking status. COPD prevalence, including by smoking status, is reported for 2022, as is combined 2018/2019/2021/2022 data for COPD treatment. Data on long COVID prevalence, symptoms and impact on daily life are also reported for 2022 for adults and children. The question in 2022 was amended so that respondents were not asked explicitly if they would describe themselves as having long COVID. Instead, those respondents who had ever had COVID and who had experienced any of a range of symptoms that could not be explained by ‘something else’ for 4-12 weeks, or for 12 weeks or longer, were included in the totals who had long COVID.
The area deprivation data are presented in Scottish Index of Multiple Deprivation (SIMD) quintiles. To ensure that the comparisons presented are not confounded by the different age profiles of the quintiles, the data have been age-standardised, as is the data analysed by smoking status. For a detailed description of both SIMD and age-standardisation as well as definitions of other terminology used in this chapter and for details on the data collection methods for respiratory conditions and long COVID, please refer to Chapter 2 of the Scottish Health Survey 2022 - volume 2: technical report.
Supplementary tables on respiratory conditions including COVID-19 are also published on the Scottish Government website: Scottish Health Survey.
3.2 Respiratory
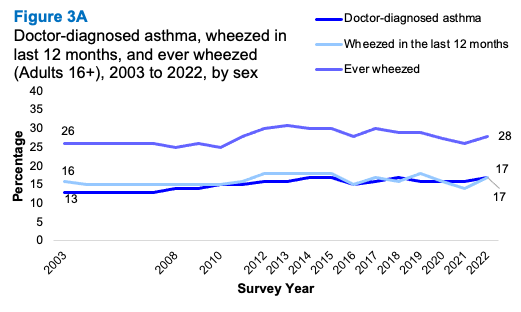
3.2.1 Doctor-diagnosed asthma, wheezed in last 12 months, and ever wheezed, 2003 to 2022, by sex
Adults
In 2022, 17% of adults reported having doctor-diagnosed asthma. Prevalence has ranged from 13% to 17% since 2003, and has remained between 16% and 17% since 2017.
The proportion of adults who had wheezed in the last 12 months was 17%, up from 14% in 2021, but within the range that has prevailed since 2003 (14-18%). Trends for females and males have been similar, with prevalence a few percentage points higher for females since 2019. In 2022, prevalence was 18% for females and 15% for males.
In 2022, the proportion of adults who had ever wheezed was 28% (females 30%; males 27%). This proportion has fluctuated between 25% and 31% since the start of the timeseries in 2003.
Children
For children aged under 16, 10% reported having doctor-diagnosed asthma in 2022. This figure is in line with those seen over the past seven years (8-10% since 2015), and is substantially lower than 2003 (16%).
In 2022, 13% of children reported having wheezed in the last 12 months. This was within the 10-14% range that has prevailed since 2003. About one-fifth (21%) of children in 2022 reported ever having wheezed (boys 22%; girls 19%), which was at the lower end of the range between 19-25% that has prevailed since 2003.
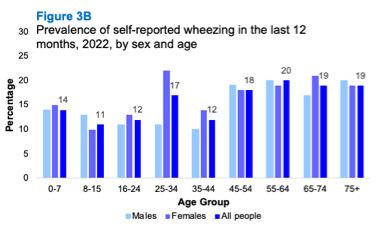
3.2.2 Doctor-diagnosed asthma, wheezed in last 12 months, and ever wheezed, 2022, by age and sex
Adults
There was a significant difference in the prevalence of asthma diagnoses by sex with 19% of women having been diagnosed with asthma by a doctor compared with 14% of men.
There were no significant variations recorded by sex for ever wheezed or having wheezed in the last 12 months and no clear pattern was evident by age among all adults.
Significant variations were evident, however, among those aged 25-34 in 2022. Just over a fifth of women aged 25-34 reported having wheezed in the last 12 months (22%) compared with 11% of men within the same age group. This pattern was also reflected for doctor-diagnosed asthma, with women aged 25-34 significantly more likely than men aged 25-34 to have been diagnosed with asthma (29% compared to 13%).
Children
In 2022, 10% of children aged 0-15 reported having doctor-diagnosed asthma. Slightly more (13%) had wheezed in the last 12 months, and 21% had wheezed at some point in their life. Boys were more likely than girls to have doctor-diagnosed asthma in 2022 (11% compared with 8%) however this difference was not significant. A significantly higher prevalence of doctor-diagnosed asthma was recorded among children aged 8-15 (13%) compared with those aged 0-7 (6%).
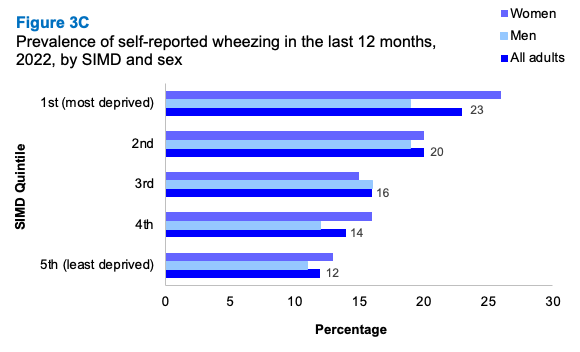
3.2.3 Doctor-diagnosed asthma, wheezed in last 12 months, and ever wheezed (age-standardised), 2022, by area deprivation and sex
The proportion of adults in 2022 who reported ever having wheezed varied by deprivation, with 36% of those living in the most deprived areas having ever wheezed compared with 23% of adults living in the least deprived areas.
A similar pattern was evident for having wheezed in the last 12 months which decreased from 23% of adults living in the most deprived areas to 12% of those living in the least deprived areas.
There were no significant variations in the prevalence of doctor-diagnosed asthma by area deprivation in 2022. The proportions of doctor-diagnosed asthma ranged between 15% and 19% in each of the deprivation quintiles.
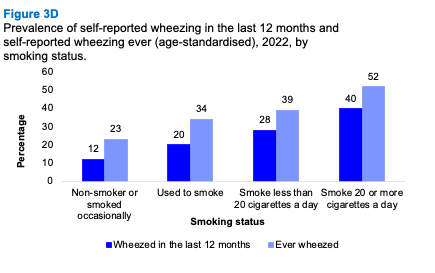
3.2.4 Doctor-diagnosed asthma, wheezed in last 12 months, and ever wheezed (age-standardised), 2022, by smoking status and sex
The proportion of adults who had ever wheezed was significantly higher among those who smoked 20 or more cigarettes a day than for those who smoked less than 20 cigarettes per day or not at all. More than half of adults smoking 20 or more cigarettes a day reported having ever wheezed (52%) compared with 23% of non- or occasional smokers. This pattern was also reflected in the proportion of adults who had wheezed in the last 12 months, which was higher among those who smoked 20 or more cigarettes a day compared with non- or occasional smokers (40% and 12% respectively).
The proportion of adults with doctor diagnosed asthma was higher for those who used to smoke than for non- and occasional smokers (21% compared to 15%), however the percentage point difference is outside of the threshold for statistical significance.
3.2.5 Doctor-diagnosed COPD, 2022, by age and sex
The proportion of adults with doctor-diagnosed COPD was 5% in 2022. While there was no significant variation by sex, the prevalence of doctor-diagnosed COPD increased with age, from <1% among adults aged 16-34 to 12-13% among those aged 65 and over.
3.2.6 Doctor-diagnosed COPD (age-standardised), 2022, by smoking status and sex
Doctor-diagnosed COPD varied by smoking status. Whereas 2% of adults who had never smoked or had smoked occasionally, had been diagnosed with COPD, this increased to 7% of those who had smoked previously, to 11% of current smokers of less than 20 cigarettes per day, and to 19% of those who currently smoked more than 20 cigarettes per day. While women more likely than men to have been diagnosed with COPD, regardless of smoking status, these variations were not statistically significant.
3.2.7 COPD treatment and type of treatment, 2018/2019/2021/2022 combined, by age and sex
Based on data from 2018/2019/2021/2022 combined, the most common forms of treatment received by people for COPD were medication (including tablets and the use of inhalers) (64%), regular check-ups with a GP, hospital or clinic (53%), and immunisations against flu/pneumococcus (28%). Less common types of treatment included advice or treatment to stop smoking (13%), and exercise or physical activity (7%).
Almost three-quarters (73%) of adults were currently receiving treatment for COPD, while 27% were not receiving any treatment. Patterns of treatment received varied by age and sex. Women in the 16-64 year age category were more likely (49%) than men (40%) to have regular check-ups. Conversely, men in this age group were more likely than women to be taking medication, including tablets and the use of inhalers (62% and 55% respectively).
3.2.8 Whether has ever had self-reported long COVID and whether limiting ability to carry out day-to-day activities due to long COVID, 2022, by age and sex
In 2022, 13% of adults reported that they had ever had long COVID, while the prevalence among children was 4%. The largest proportion of adults that reported ever having long COVID was recorded among those aged 45-54 (19%) while the smallest proportion was recorded for those aged 75 or over (7%).
A significant difference in ever having long COVID was recorded between men and women aged 35-44 in 2022. A higher proportion of women aged 35-44 reported ever having long COVID (21%, compared with 8% of men in the same age group).
Just over one in twenty adults reported that long COVID limited their ability to carry out day-to-day activities a lot (6%), and 5% reported that long COVID limited their activities a little.
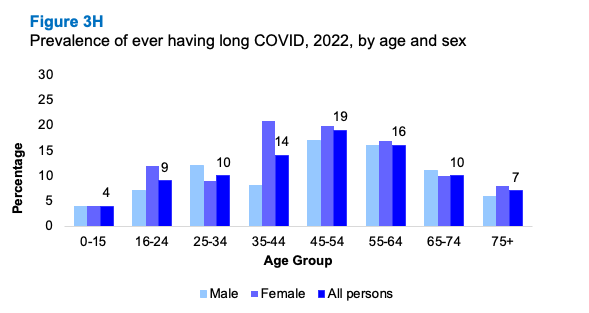
Table List
Table 3.1 Doctor-diagnosed asthma, wheezed in last 12 months, and ever wheezed, 2003 to 2022, by sex
Table 3.2 Doctor-diagnosed asthma, wheezed in last 12 months, and ever wheezed, 2022, by age and sex
Table 3.3 Doctor-diagnosed asthma, wheezed in last 12 months, and ever wheezed (age-standardised), 2022, by area deprivation and sex
Table 3.4 Doctor-diagnosed asthma, wheezed in last 12 months, and ever wheezed (age-standardised), 2022, by smoking status and sex
Table 3.5 Doctor-diagnosed COPD, 2022, by age and sex
Table 3.6 Doctor-diagnosed COPD (age-standardised), 2022, by smoking status and sex
Table 3.7 COPD treatment and type of treatment, 2018/2019/2021/2022 combined, by age and sex
Table 3.8 Whether has self-reported long COVID and whether limiting ability to carry out day-to-day activities due to long COVID, 2022, by age and sex
Contact
There is a problem
Thanks for your feedback