Coronavirus (COVID-19): Scotland's Strategic Framework update - February 2022
This update of the Strategic Framework assesses where we are in the pandemic and sets out Scotland’s approach to managing COVID-19 and its associated harms effectively for the long term as we prepare for a calmer phase of the pandemic.
This document is part of a collection
Delivering our approach
Vaccination
Progress
Vaccination remains a critical component in our response to COVID-19. From the outset the primary objective of the vaccination programme has been to prevent severe illness and death associated with the virus. Our vaccination programme has delivered on this, with the WHO reporting that up to November 2021, vaccination in Scotland was likely to have prevented over 27,000 deaths from COVID-19. Recent evidence has also highlighted the important role boosters can play as part of our ongoing response, especially to emerging variants such as Omicron.
Scotland's autumn/winter Flu and COVID-19 Booster Programme which began on 6 September 2021, has now surpassed 6.7 million doses and builds on the 7.8 million COVID-19 vaccinations delivered during the first phase of the Programme (between December 2020 and September 2021). As of 21 February 2022, there had been over 11.9 million COVID-19 vaccine doses administered in Scotland, and over 2.7 million flu doses.
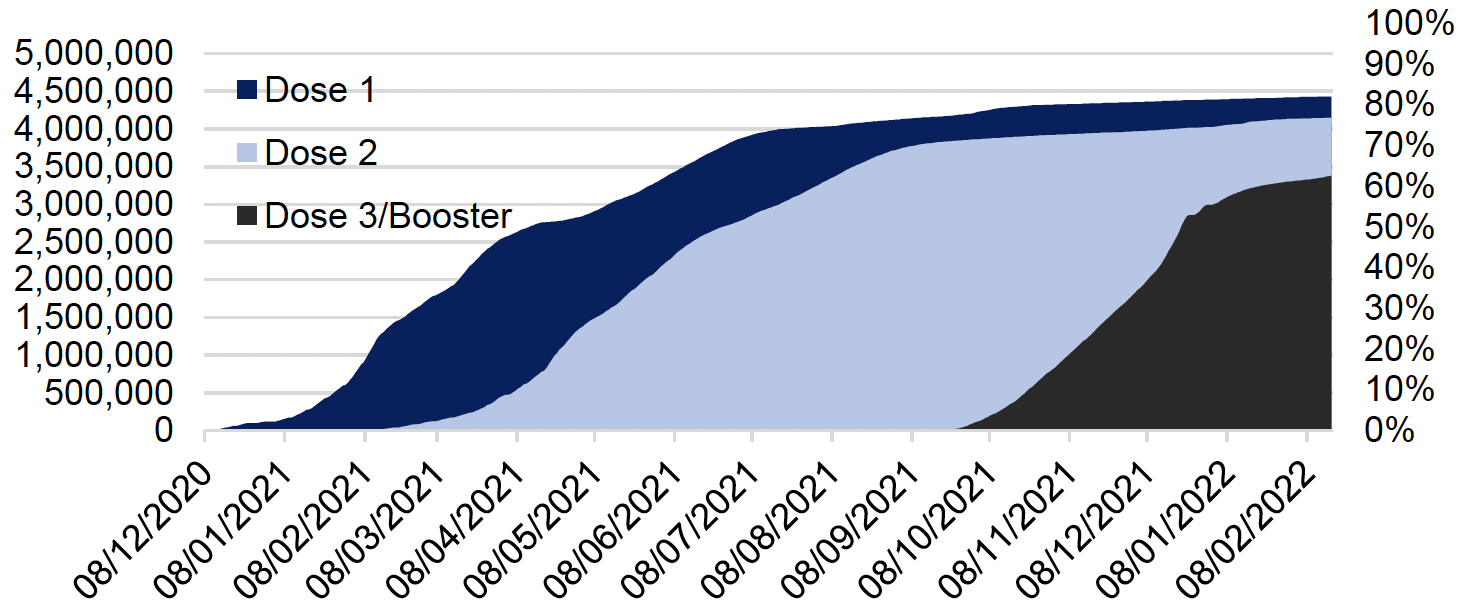
In order to protect more people in Scotland, and in line with the independent and expert advice received from the Joint Committee on Vaccination and Immunisation (JCVI), we have expanded our COVID-19 vaccination eligibility criteria. More individuals under the age of 18 are now eligible for first and second doses, with some also eligible for boosters. All adults (16 and over) are eligible for a booster vaccination and, third primary doses are now being provided for all those aged 5 years and over, who at the time of their first or second dose are identified as being severely immunosuppressed. Following receipt of JCVI advice, we are also starting to offer vaccines to all 5 to 11 year olds recognising that this will offer protection from serious illness and hospitalisation in a future outbreak.
As of 18 February 2022, 92% of those aged 12 years and over have had a first vaccine dose and 87% have had a second dose. In addition, 84% of 16 to 17-year-olds had received a first dose of the vaccine with 58% also receiving their second dose. Currently over 3.3 million booster/third doses have been delivered which equates to around 71% of the eligible 12 and over population.
Next Steps
We are now working on the delivery plan to offer vaccination to all 5 to 11 year olds, following recent advice from the JCVI and will be shortly offering an additional booster to all adults over 75 years old, care home residents and everyone over 12 who is immunosuppressed.
We also have a planning assumption that there will be a continued need for vaccinations in response to COVID-19 in 2022/23 and beyond. We are, therefore, preparing for a continued need for some level of ongoing booster vaccination activity, particularly for those at highest risk.
We are also ensuring that people who may experience barriers, or feel less confident, are able to come forward for vaccination. We are increasing our efforts to ensure the vaccination programme reaches everyone and is fully inclusive with a range of outreach activities and partnerships with community and third sector organisations to engage with under-represented groups. This will include the continued use of research and focus groups to understand the reasons and potential barriers to individuals who may be vaccine hesitant. Building on our approach used for under-represented groups, this will inform our communications and engagement activity, and also our deployment model.
Current evidence provides confidence that the booster vaccination programme has greatly strengthened population immunity against severe illness. However, we also know that evidence is still emerging on waning vaccine protection, and there is a risk of future Variants of Concern developing - against which protection afforded by vaccines may differ.
On that basis, we are planning for a number of different scenarios including an annual booster programme, for those who are at risk and possibly more frequently for the most clinically vulnerable. These planning assumptions will be refined once we receive further JCVI advice on this issue. We are aware of the need to deliver rapidly in response to either a new variant and/or the emergence of a more variant-specific vaccine. Work is in hand to develop surge plans that could be rapidly deployed, if required, building on the lessons learnt from our response to Omicron in November and December 2021.
A core element of activity and planning is to ensure that there is a sustainable model for the delivery of COVID-19 vaccines alongside existing vaccination and immunisation programmes in Scotland. COVID-19 learning and infrastructure provides us with an opportunity to consider the full range of immunisation activity to achieve a positive and lasting legacy from the pandemic. We are therefore taking into consideration the Scottish Vaccination and Immunisation Programme (SVIP) aspirations and ensuring that existing vaccination programmes are maintained as part of our overall public health objectives.
Testing and Surveillance
Progress
The Test and Protect programme has continued to play a key role in our response to COVID-19 by providing testing, contact tracing and supporting self-isolation, all essential in reducing the health and broader harms caused by COVID-19.
The advent of Omicron tested the system to its maximum levels, with record-breaking levels of PCR testing conducted, LFDs distributed and results reported by the public. Winter saw the highest ever levels of PCR testing for COVID-19 since the pandemic began. The period of significant testing demand meant that the volumes of PCR test results being reported in the first week in January 2022 (452,000 tests) was double the level that was reported in the first week in November 2021 (226,000 tests).
In response to the unprecedented increase in demand, in December sampling capacity was maximised by increasing booking capacity by 50% at test sites, along with increased laboratory, PCR home test and online LFD ordering capacity. When the testing system demand reached 85% capacity levels (on 29 December) we started prioritising access to PCR test sites for essential workers, highest risk groups and those eligible for new COVID-19 treatments.
Since the festive period, and changes to testing policy to remove confirmatory PCR tests, we have seen a significant decrease in the levels of daily PCR testing, now settling at around 8,000-12,000 tests per day.
The high number of cases driven by Omicron, and our guidance and intensive media and marketing activity to encourage people to use LFD tests before mixing with others over the festive period, also saw exceptional demand for LFDs over December and early January. Demand reached as high as 8-10 million tests each week, compared to the 10 million LFD tests distributed per month in the autumn. The increase in demand for tests also led to a significant increase in the number of LFD results being reported, with the numbers of tests per week being recorded increasing by 135% between the end of November and the end of December. Record numbers of individuals also entered the contact tracing system over this period, with over 130,000 unique positive cases being created in the contact tracing system within one week at the turn of the year - compared with around 20,000 index cases per week in late November 2021. The number of LFD results reported has been decreasing in the early weeks of 2022 but the levels of LFD test result recorded in the week ending 13 February 2022 remained over 94% higher than at the end of November 2021.[21]
In response to the emergence of the Omicron variant, public health advice on self-isolation changed in December to reflect the early evidence on transmissibility and the lack of data, at that point in time, on the potential severity of Omicron and consequent population health risks. As evidence accumulated, and the vaccination booster programme rolled out, from January 2022, further policy changes included:
- reducing the isolation period for index cases from 10 to 7 days to improve workforce and system resilience across key sectors of the economy;
- removing the requirement for a confirmatory PCR after a positive LFD;
- replacing negative PCR with negative LFD to release from isolation; and
- removing the close contact isolation requirement for triple-vaccinated adults/under 18s with negative PCR/LFD.
Next Steps
Our approach to testing – and to tracing and isolation – has continually adapted as pandemic conditions have changed; as our understanding of the virus and disease has grown; as new technologies have become available and their reliability has been demonstrated; and as the public have adopted new behaviours and understanding of testing as a means of reducing risk. This adaptation will continue, and the scale and place of Test and Protect in our range of interventions will adapt to be proportionate to the requirements of future phases and in alignment with our updated strategic intent.
As part of a careful and phased transition – the detail of which we will set out in March - our Test and Protect approach will focus on the following key priorities:
- to protect the most vulnerable and those at highest clinical risk (a core priority throughout the pandemic);
- to support patient care;
- to monitor disease prevalence;
- to respond to outbreaks; and
- to scale as required for future health threats.
As we move through the spring and into the summer, our priorities will move away from the current routine asymptomatic programmes of testing towards ensuring continuing and sufficiently rapid access to:
- testing for those who require clinical care or would benefit from new and emerging treatments;
- a continued focus on protecting those at highest clinical risk;
- maintaining sufficiently robust surveillance (including genomic sequencing) to detect emerging issues early enough for effective response;
- continuing to support local responses in communities where there is enduring transmission; and
- supporting outbreak management and mitigation in particularly high-risk settings – with the ability to scale our response as required to address threat levels in the future.
In order to move to this new Test and Protect approach we are developing a managed transition plan which will ensure that Scotland continues to have a proportionate and effective testing response and effective domestic and international surveillance infrastructure.
We will publish a detailed transition plan in March setting out updated plans for Test and Protect for the endemic phase, and how we will manage the transition from the current position to that end steady state. This will confirm the duration of the transition beyond the end of March. It will also include detail on surveillance capabilities that will remain long term; contingency infrastructure scalable if required in the event of a future variant; and continuing provision of testing to protect those most vulnerable, support clinical care, enable prompt treatment for COVID-19 patients where required, and build a legacy for wider population health benefit.
In the meantime, we will continue to support access to PCR and Lateral Flow Testing on the same basis for the general population as now, subject to the changes in advice on frequency of lateral flow testing set out below.
In line with our progress though the Omicron wave, we are evolving our population level asymptomatic testing approach from the current advice to test on every occasion before mixing with others, back to advice to test at least twice weekly and in particular before mixing in crowded places or with anyone who is clinically vulnerable through age or other health conditions.
We are also reviewing the frequency of asymptomatic testing taking place within our health and social care workforces and may revert in the period ahead from daily to twice weekly testing. However we will only do this in line with the latest clinical advice and risk assessments.
We have also asked the educational advisory subgroup for advice on lateral flow testing for schools and will update our approach when this is available.
We still advise those with symptoms to book a PCR test.
And we continue to advise anyone who tests positive – either through a PCR or a Lateral Flow Test – to stay at home for the recommended period of isolation to reduce the risk of infecting others, including those who may be clinically vulnerable. We will keep the recommended period of isolation for positive cases under review. Contact tracing and advice to contacts also continues at this point, as does support for those advised to isolate.
At the conclusion of the transition period, contact tracing and isolation are likely to focus more on those settings that are highest risk, with local Health Protection teams empowered to make local public health decisions on how to reduce risks to people who are clinically vulnerable. Subject to ongoing evidence of vaccine efficacy, population wide isolation guidance will focus on encouraging people with symptoms of respiratory illness to remain at home whilst unwell.
Our detailed transition plan will be published in March setting out updated plans for Test and Protect for the endemic phase, and how we will manage the transition from the current position to that end steady state. This will include detail on surveillance capabilities that will remain long term; contingency infrastructure scalable if required in the event of a future variant; and continuing provision of testing to protect those most vulnerable, support clinical care, enable prompt treatment for COVID-19 patients where required, and build a legacy for wider population health benefit.
COVID-19 Surveillance
Alongside the test and protect system, the Scottish Government has worked with PHS and the UK Health Security Agency (UKHSA) to undertake a number of enhanced public health surveillance programmes that provide deeper insight into the impact of COVID-19 on people living in Scotland and on NHS services in Scotland. These programmes provide statistically and clinically robust information on transmission, on immunity and on the effectiveness of clinical and public health countermeasures, which has supported public health decision making.
In addition, since September 2020, people living in Scotland have participated in the UK-wide ONS COVID-19 Infection Survey, which is partly funded by the Scottish Government by forgoing Barnett consequentials. This survey provides vital data that inform weekly estimates of the number of people living in Scotland who are positive with COVID-19, and fortnightly estimates of the number of people testing positive for antibodies from a blood sample. This method has allowed a stable platform for assessment of incidence and prevalence unaffected by changing population use of PCR or LFDs, which has been problematic for other surveillance components.
Through a collaborative programme of work with the Scottish Environment Protection Agency (SEPA), Scottish Water and bioinformaticians, we are collecting data through wastewater surveillance to inform weekly modelling the epidemic reports.
The continuing pandemic, and the potential for the resurgence and atypical circulation of other respiratory pathogens, underlines the need to enhance existing epidemiological surveillance systems in order that we respond early, proportionately and precisely. Over the next year, we will continue to work with stakeholders to ensure an appropriate surveillance system is in place to monitor, track and respond to future changes in the pandemic and the effectiveness of our interventions.
This system will include developing an enhanced community surveillance in primary and secondary care, early detection of new variants through Whole Genomic Sequencing (WGS) in collaboration with UKHSA and international partners, understanding the opportunities presented through waste water surveillance and exploring future joint opportunities with other UK nations. Details of the surveillance programme will be included in the updated Test and Protect plan.
Self-isolation support
While self-isolation advice remains a population-wide intervention, support for people self-isolating will continue including the Self-Isolation Support Grant. As isolation guidance evolves, we will continue to consider where targeted isolation support, including financial support, is required to support communities experiencing enduring transmission and COVID-19 related health inequalities.
Data and Analysis
Scottish Government decision-making throughout the pandemic has been based on a range of evidence including scientific and clinical studies, modelling, behavioural research, statistics and analysis. Much of this has necessarily been new and we worked with partners, including PHS and UKHSA, to rapidly develop new data collections and reporting over the course of the pandemic.
This has included rapid data and intelligence to support and inform decision-making such as case numbers, hospital and ICU occupancy, deaths, vaccinations, and other COVID-related data covering schools, care homes and NHS absences. Key published data series have included reporting of headline daily data on the Scottish Government Coronavirus web pages, a weekly State of the Epidemic paper and the latest ONS COVID-19 Infection Survey results. PHS have also developed significant new and interactive reporting on the PHS COVID-19 Daily Dashboard and Education Surveillance Dashboard and continued to develop the content of its PHS weekly COVID-19 statistical report that is published every Wednesday.
We now need to consider what evidence, data and analysis will be required going forward. Work is now under way with PHS and our partners to review the content and frequency of all of our current reporting to identify what is required to support resilience and recovery in the future. This will involve prioritising the modelling, data and analysis that is essential to support the future monitoring and surveillance of COVID-19. We are now identifying the key public reporting that needs to be retained and the frequency of publication. We will publish a data and reporting strategy in spring 2022 to support implementation of the Strategic Framework. We will ensure that users and the public are consulted on any planned changes to public reporting.
Treatment
Thanks to advances in health research, treatments are becoming an increasingly important part of our overall approach to managing COVID-19 for the long term. This section sets out both what we are doing to ensure that people are able to receive effective treatment for COVID-19, drawing on advances in technology and practice, and our activity to support people affected by the long-term effects of COVID-19.
COVID-19
Progress
A range of new therapeutics is now well established in the management of patients who have been admitted to hospital with COVID-19. Treatments including dexamethasone, neutralising monoclonal antibodies, remdesivir, tocilizumab and sarilumab can reduce serious illness and deaths.
We are now also offering new therapeutics which have been authorised by the Medicines and Healthcare products Regulatory Agency (MHRA) for use in non-hospitalised patients at higher risk of admission from COVID-19.
Since 22 December 2021, adults and children (aged 12 years and above) are eligible to be assessed for their suitability for new COVID-19 treatments if they meet certain eligibility criteria. The list of clinical conditions prioritised for treatment was developed by an independent UK expert working group based on detailed clinical evidence and is designed to support targeting those higher-risk patients who have the potential to both be at highest risk of disease progression, hospitalisation and death and be least likely to generate a material immune response to vaccine. More information on the eligibility criteria and access arrangements can be found on NHS Inform (https://www.nhsinform.scot/covid19treatments).
In addition to the direct access arrangements described, oral antiviral treatments for COVID-19 are being evaluated through a UK-wide study called PANORAMIC, run by the University of Oxford. This is open to people living anywhere in the UK who meet all three of the following criteria:
1. a positive PCR test result for coronavirus;
2. feel unwell with symptoms of coronavirus that started in the last five days; and
3. are aged 50 or over or aged 18 to 49 with an underlying medical condition (full details at https://www.panoramictrial.org/) that can increase the chance of having severe coronavirus symptoms.
Next Steps
The national study will lead to the collection of additional data to enable the NHS to fully understand how best to make use of these antiviral treatments in the future.
Long-term effects of COVID-19 (Long COVID)
Progress
NHS Scotland continues to deliver a range of services to support the individual needs of people affected by the long-term effects of COVID-19.
We are implementing the 16 commitments to improve care and support for people with long COVID-19 contained in our approach paper Scotland's Long COVID Service, which are backed by a £10 million Long COVID Support Fund. Our approach is based on maximising and improving co-ordination of the broad range of existing services across our health and social care system and third sector that are relevant to the spectrum of symptoms that people are experiencing.
In addition, we have developed a long COVID information platform on NHS inform to help people manage their symptoms and access further support where required.
This initiative was supported by a targeted marketing campaign which ran through October and November 2021 with information displayed in GP surgeries and community pharmacies. A campaign toolkit was also sent to 250 direct partner contacts with additional distribution to approximately 3,000 contacts.
Next Steps
We will continue to support the implementation of the UK-wide clinical guideline on the long-term effects of COVID-19, developed by the Scottish Intercollegiate Guidelines Network (SIGN), the National Institute for Health and Care Excellence (NICE) and the Royal College of General Practitioners (RCGP), through which clinicians can access evidence-based information and advice to inform assessments, investigations and referrals for their patients.
NHS National Services Division is establishing a Strategic Network bringing together clinical experts, NHS Boards and lived experience to support the ongoing development, resourcing and implementation of services for people with long COVID in Scotland.
Deploying Protective Measures When Necessary
As the updated strategic intent makes clear, in the future we expect health measures and adaptations to be our primary means of managing COVID-19 effectively, enabling a sustainable return to much more normality.
However, there remains a need for protective measures as a contingency that can be deployed if and when the virus again threatens us with excessive harm, which we hope will rarely be the case. By 'protective measures' we mean legal requirements (regulations) and targeted guidance over and above more general positive behaviours, adaptations and good practice measures to curb the virus.
Protective measures would be used temporarily to respond effectively to increased threat from the virus, for example, if a more harmful variant was identified. We want to provide as much clarity around this as we can, notwithstanding the uncertainty inherent in the virus, to help people and organisations plan for the future.
Current measures
Thanks to the collective efforts of the people of Scotland and the success of the booster rollout, we currently have relatively few protective measures in place to help manage COVID-19. Nevertheless, the virus continues to cause significant harm to our health, essential services, economy and society. Many of those who are at higher clinical risk are still wary of undertaking normal everyday activities and we are seeing the ongoing impacts of long COVID on previously healthy individuals. Our NHS and social care services continue to face a challenging period ahead as they deal with the backlog of patients as well as ongoing COVID-19 hospitalisations.
So we must all continue to exercise caution and be vigilant. We continue to encourage everyone to:
- Increase ventilation by opening a window, or going outdoors.
- Wash your hands and cover your nose and mouth if coughing or sneezing.
- Where appropriate, do a mixture of home and office ('hybrid') working.
- Get your vaccine or booster when you are eligible.
- Use the Protect Scotland and Check-in Scotland apps.
- Take a Lateral Flow Device (LFD) twice weekly, in particular before mixing in crowded places or with anyone who is clinically vulnerable;
- Take a PCR test if you develop COVID-19 symptoms or if Test and Protect ask you to.
- Self-isolate for the recommended period if you test positive or are asked to do so by Test and Protect.
While most of the regulations regarding protective measures have now been lifted there are still four baseline measures that continue to be required by law (at the time of the publication of this document):
- You must wear a face-covering in most indoor public spaces and on public transport (unless an exemption applies).
- Hospitality businesses are required to collect and share customer information to support Test and Protect contact tracing.
- Businesses, service providers and places of worship are required to have regard to guidance about reducing risk of exposure to COVID-19 on their premises and take reasonably practicable measures to reduce incidence and spread of COVID-19 on their premises.
- Large events and late night venues must operate the COVID-19 certification scheme. [See below for plans to adjust this measure.]
In time we plan to convert these legal measures to guidance, and often it will make sense for individuals and organisations to continue to adopt them, where appropriate, in order to help maintain effective control of the virus. It will remain important to consider how the decisions we all make can affect others, particularly those who may be at higher clinical risk from COVID-19.
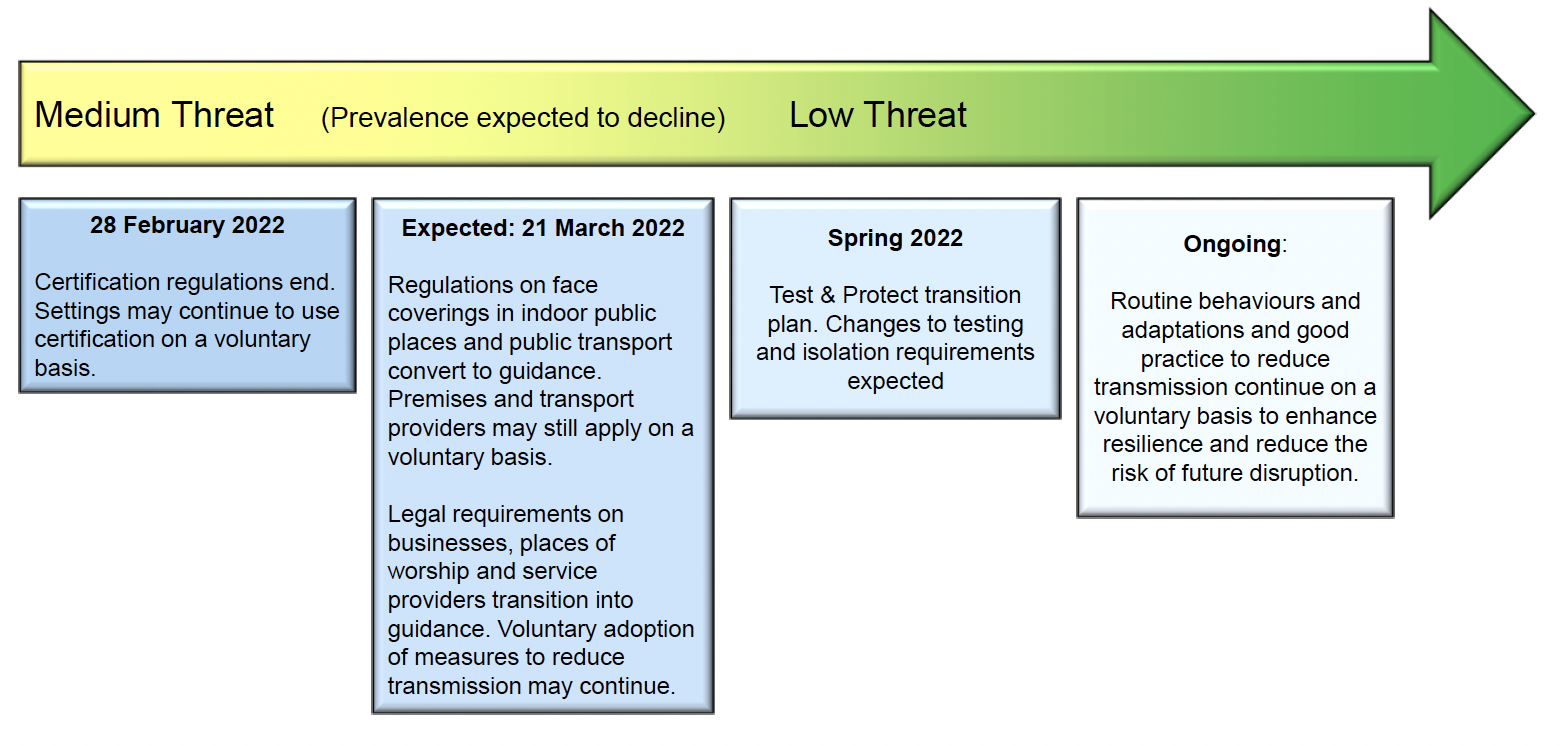
Figure 10 sets out our plans for moving the remaining protective measures from regulation to guidance and good practice.
On 28 February, the legal requirement for COVID-19 certification in certain settings will end. Some premises may, however, wish to continue to require such certification, to make their customers and staff feel safer.
On 21 March (indicative date, to be confirmed at preceding review), we plan to remove the legal requirement for face-coverings in indoor public places and on public transport. Again, some settings and service providers may wish to maintain face-covering policies to help to protect their customers and staff. Other remaining legal requirements will convert to guidance and good practice as appropriate.
Following this, we plan to move to a more sustainable approach to testing, self-isolation and contact tracing, as we progress through our Test and Protect transition plan. We will provide more information about the future requirements closer to the time.
We anticipate moving to a position where, as with other infectious diseases, we advise people generally to stay at home if they are unwell until their symptoms resolve and they feel better. This will continue to help protect others, and will be of particular benefit to those who may be at higher clinical risk. Testing is likely to remain an element of our management of the virus in particular settings, for example to help protect those at higher clinical risk, and to maintain surveillance of the virus and its variants.
Once legal requirements are lifted, we expect that people and organisations will continue as a routine to adapt their behaviours and settings in ways that reduce the spread of the virus. This will help us all to enjoy as much normality as possible and provide resilience to future threats from the virus, potentially reducing the need for increasing protective measures again.
Responding to future threats
Despite this planned shift away from legal requirements, we will still need to manage COVID-19 effectively because the virus remains a threat. We are likely to continue to see outbreaks in Scotland over the coming years, and can expect new variants to appear globally. We should expect a degree of ongoing uncertainty about the threat posed by the virus. If infections rose too high or the impact of the disease became too grave, then the harm in terms of mortality and morbidity, including long COVID, would be excessive and our NHS would again be at risk of being overwhelmed. It may therefore prove necessary to take steps to protect people from serious illness and death. This might involve implementing temporary and targeted protective measures, either within individual settings, in certain localities or nationally.
Local Outbreak Management
Working collaboratively with public health and local government partners, we are developing and will publish a COVID-19 Outbreak Management Plan. This will set out a set of short and medium-term measures that can mitigate impact in specific localities. It will include processes to commission and use research, to assess the risk posed by a variant, determine possible response objectives and options and continually assess the operational success through intervention.
The guidance on the Management of Public Health Incidents sets out the strategic approach to managing public health incidents (including outbreaks of infectious diseases) and provides support to NHS Boards in preparing for and responding to incidents, allowing flexibility to respond as appropriate in collaboration with partners.
We will use the collective learning of the last two years to consider with PHS, Directors of Public Health and partners from local government and other agencies any changes that may be required to the guidance on the Management of Public Health Incidents.
Managing future threats at the national level
Through adaptations to our behaviours and physical environments to reduce the spread of COVID, and through effective vaccination and treatment, we can reduce the risk that we will need to escalate protective measures in the future. The better we collectively do at protecting ourselves through making these measures routine, the less the future need for additional measures in the event that a more harmful variant arises as it should cause less harm.[22] This is because adaptations help to reduce infection risk, treatments help to reduce disease impact, and vaccinations help to reduce both.
Though these routine efforts will reduce the impact of a more harmful variant, there remains the risk that a new variant will arrive in Scotland that is sufficiently harmful, in terms of transmissibility or severity (or both), that it requires additional protective measures, for a temporary period.
We will remain vigilant for this risk, through ongoing surveillance of the evolution and spread of variants. Vigilance and preparedness are important because there are times when responding quickly can mitigate harm and potentially avoid the need for more stringent and harmful interventions later. In particular, we want to have as early an indication as possible when such variants appear in Scotland or elsewhere in the UK, and the ability to develop a rapid understanding of how fast they are spreading.
We will be looking out for variants that are significantly more transmissible or better at bypassing immunity than the existing dominant strain in Scotland – because of the risk that they will lead to an overwhelming volume of cases such that, even if the variant is no more severe in terms of individual disease, it risks a high population volume of disease and hence overwhelming the NHS.
We will also be looking out for variants, which have seeded in Scotland or elsewhere in the UK, that may be significantly more severe than the current dominant strain and so likely to cause greater morbidity and mortality if able to spread in an unmitigated manner.
As well as monitoring developments internationally, including through WHO and UKHSA designations of variants, indicators that we would be particularly watching include:
- numbers of cases of the variant in Scotland and elsewhere in the UK;
- COVID-19 hospital and ICU admissions;
- numbers of COVID-19 deaths and the infection fatality ratio; and
- vaccine efficacy.
Both overall numbers and breakdowns by age group will be important for such indicators to gain a better understanding of expected harm.
We would also monitor epidemiological intelligence from areas or countries that already have experience of relevant variants (e.g. for early indications of severity of disease or increased transmissibility) as they may provide valuable early insights.
Our assessment of the necessary and proportionate response to a new variant will take account of what the available evidence tells us about its transmissibility and severity. If one or other of these were assessed to have significantly increased, then that would likely increase the assessed threat. Our assessment would also take account of factors such as our broader resilience to a more harmful variant (e.g. current NHS capacity, the likelihood of concurrent risks, such as flu, the adequacy of adaptations, and waning immunity). Careful, rounded judgement will need to be applied to take account of these various factors.
As Figure 11 illustrates, our assessment of COVID-19 threat will combine an assessment of potential disease impact and risk of infection. Assessment of disease impact (severity) will consider current and expected infection fatality rates as well as indicators of morbidity, such as Long COVID. Assessment of infection risk will consider current and expected prevalence rates and virus transmissibility. The application of judgement taking all relevant information into account will be key in making these threat assessments, and the UK Alert Levels, and any changes to them, can help to inform this judgement.
At the time of publishing this Framework (late February 2022) we judge that Scotland is currently around the top right of this matrix, which is a 'medium' threat level. This reflects a variant in Omicron that is highly transmissible (with the infection level still high) but of lower severity. Assuming that the level of infection falls - or at least stabilises in the weeks ahead - it is likely that our 'threat' level will move down to "low" as we head into the spring and summer.
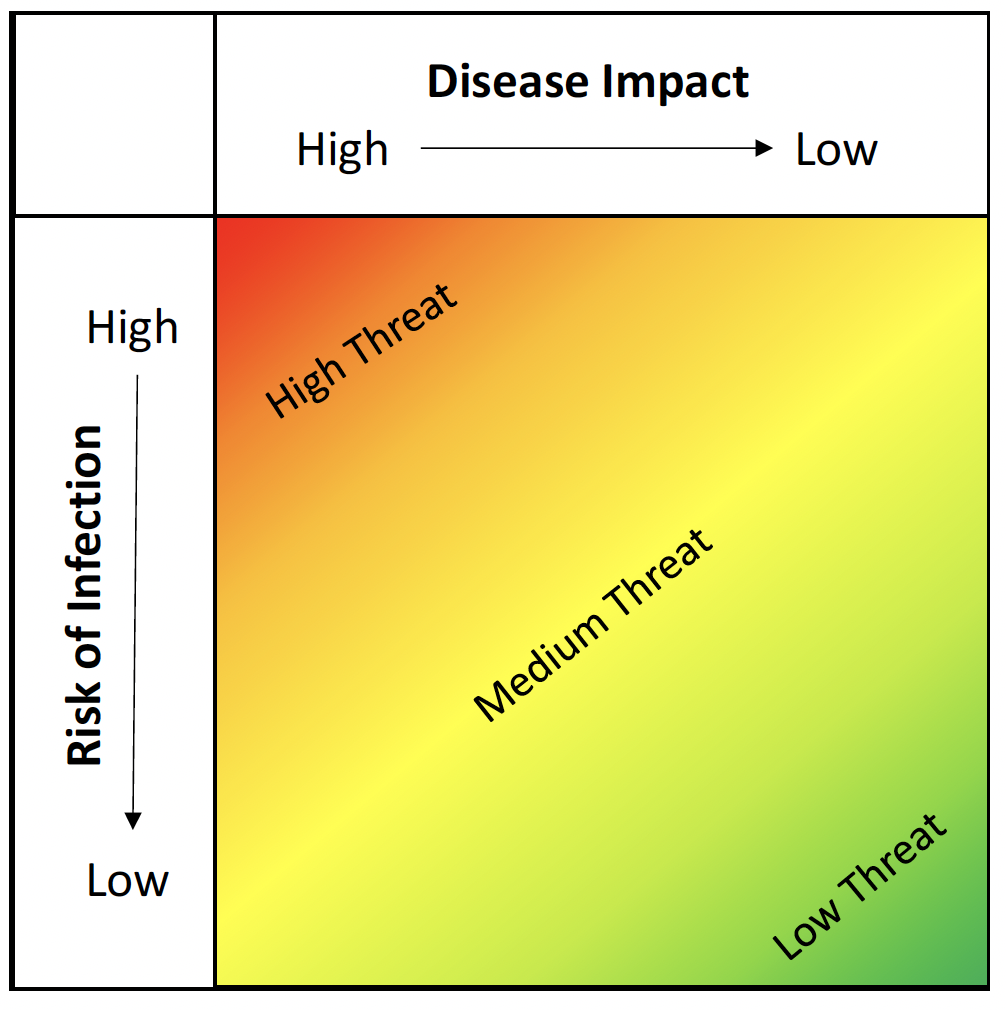
Note: All threat assessments will reflect balanced judgements of all relevant factors at the time. They will assess what would likely happen in Scotland in the near future in the absence of an effective response to a threat.
An example of a 'medium threat' might be a variant being identified in Scotland/UK that was either significantly more transmissible or significantly more severe (but not both) than the current dominant strain (if that strain were assessed as a low threat).
An example of a 'high threat' might be a variant being present that was both significantly more transmissible and significantly more severe, with the threat level increasing further to the extent that the variant evades immunity.
Of course, with an effective response, a threat may be averted, alleviated or delayed until other measures such as surge vaccination or surge testing had been deployed, or allowing time for treatments, adaptations and other capacity to be scaled up. That could mean that the potential threat of a more harmful variant did not ultimately materialise (in the way it would have done without the effective response).
In forming judgements about the threat we face, and the implications of different potential responses, we will take advice and gather information as appropriate from a range of sources, such as the UK Alert levels, and organisations likely including:
- Public Health Scotland / NHS National Services Scotland
- Chief Medical Officer, NHS Clinical Director, Chief Social Policy Adviser, Chief Economic Adviser
- COVID-19 Advisory Group (when activated)
- National Incident Management Team (when activated)
- International and UK advisory bodies - WHO, UKHSA/JBC, SAGE, JCVI etc.
Decisions on responses will be consistent with relevant legislation. They are likely to be finely balanced judgements, made under a degree of uncertainty – for example, because it typically takes some weeks for reliable information about a new variant to emerge, whereas effective responses may need to be implemented on a shorter timescale. If we overestimate the potential harm of a variant then we risk imposing excessive protective measures and causing unnecessary broader harm. If we underestimate the harm of a potential variant then we risk having inadequate protective measures in place, leading to avoidable morbidity and mortality as well as economic and societal impacts, and potentially necessitating more extensive protective measures than would have been needed with an earlier effective response.
The exercise of careful, evidence-based judgement will always be required to ensure that responses are necessary and proportionate and therefore lawful, given the circumstances and all relevant factors pertaining at any given time. To follow a more mechanistic or prescriptive approach in which particular data crossing certain thresholds automatically triggered responses, attractive as that might appear in terms of perceived certainty and future planning, would risk the response being disproportionate and unlawful at the time of implementation. This is because such decisions on making regulations need to take into account all relevant factors.
To illustrate this point, triggers or thresholds based on case numbers might lead to disproportionate decisions if the conversion rate from cases to serious morbidity and mortality reduced. Similarly, triggers based on admissions to hospital or ICU might be disproportionate if there were ample capacity within the NHS to cope with such admissions – so the response to a given variant might differ depending on whether it arrived at the start of the summer or the start of the winter.
In addition, the current wellbeing and resilience of people and organisations, including businesses, that are likely to be subject to any increased protective measures also need to be considered, particularly as impacts accumulate over time. This underlines the 'four harms' approach to weighing up decisions as we acknowledge that mitigating harm in one area might increase it in another. For all these reasons, though epidemiological indicators will continue to inform our decision-making, the application of rounded, evidence-based judgement in deciding a response will remain key.
The purpose of our response would be to slow, and potentially reverse, the spread of the virus and so reduce serious health harm. This might be, for example, to avoid a very high peak that risked overwhelming the NHS, or to buy time for (surge) booster vaccinations or for adaptations to be enhanced so as to reduce transmission or severity, or both. And, of course, regulatory measures are not the only means that we have to mitigate the harm of a new viral threat. For example, enhanced infection controls could rapidly be implemented as appropriate in hospitals and care homes and targeted public health advice could be issued to those at higher clinical risk, alongside more general public health communications and marketing to alert people to the heightened threat and encourage them to voluntarily adapt their behaviour.
Gradated responses reflecting the assessed threat level
We will manage COVID-19 going forwards on the basis of four broad response categories that reflect the assessed threat. Note that the measures within each response category should not be seen as 'all or nothing' but rather as a gradated set of options. So, for example, it would be possible to select one or two measures from a higher response category as a way to increase protection. Or, as part of the process of easing protective measures, it would be possible to release one or two measures but retain others from the category.
The more protective measures that are applied from each response category, the greater the degree of downward pressure on transmission of the virus, but also the greater the associated broader harms to the extent that economic and social activities are disrupted (acknowledging both that escalating harm from the virus would itself disrupt activity and that early intervention may reduce the need for more extensive intervention later).
As noted, applying evidence-based judgement as to the appropriate response level, taking all relevant factors into consideration, will be key. And whilst it may sometimes be the case that making fewer changes over a period is appropriate, to create more stability, at other times it may make sense to have a staged approach to either escalating or easing protective measures – always dependent on a rounded assessment of the relevant factors and circumstances.
The first category of response consists of the routine adaptations to behaviours and settings that are likely to become an essential part of how we all live with COVID-19 going forwards, alongside individuals taking up vaccines when invited to do so and having the testing and treatment regime in place to assess the prevalence and mitigate the impacts of COVID-19. These routine activities and measures will strengthen our resilience for a world in which COVID-19 will remain part of our lives. They are how we expect to actively manage COVID-19 when the threat from the virus is low, as we hope that it will be for long periods in the future. This response level should see minimal if any disruption to economic or social activity.
The second response category consists of temporary, baseline protective measures that would provide an additional layer of protection if we assess there to be an increased risk of COVID, broadly up to a 'medium' threat, that would lead to significant increase in COVID-19 morbidity and mortality. Again, individual or groups of measures, as well as the full set, could be judged appropriate according to the assessed threat.
Judgements around the reintroduction of baseline measures would also take into account the recognised need for stability and to avoid frequently changing rules and advice concerning protective measures. It would depend on a rapid assessment both of the transmissibility and severity of the variant and of the current state of resilience to the virus (e.g. strength of adaptations, available hospital capacity, likely vaccine and treatment effectiveness etc.). In some circumstances no escalation of response may be judged necessary for a given threat; in other circumstances, additional temporary baseline protective measures may be necessary and proportionate.
The third and fourth categories of response would only be applied if we judged that we face a 'high' threat from the virus that, without a significant response, would cause a very large increase in morbidity and mortality. This judgement would take account of other relevant factors, such as the effectiveness of baseline and routine protections and NHS capacity at the time. The choice of measures (or a combination of them) would be determined in light of the characteristics and trajectory of the variant causing the threat and not all of them might be judged necessary and proportionate, according to the threat assessment. We recognise the increased impacts these types of responses have on the economy and society and therefore would only use them when absolutely required.
The third category consists of temporary, targeted protective measures, similar to those that were applied to deal effectively with the Omicron variant. These are likely to involve legal measures affecting certain higher risk settings and activities.
The fourth and highest response level would consist of temporary, extensive protective measures. This would involve legal restrictions and requirements for a wider range of settings and activities but would likely still fall well short of a 'lockdown'. We consider the need to use such extensive protective measures in the future as unlikely. Their use would mean that we judge the virus to pose a 'high' threat to a particularly large number of people, quite possibly because of the prospect of significant immune escape – i.e. evading the widespread immunity now built up in the population – a situation that we hope is unlikely to transpire, but that we must nevertheless be ready for. This judgement would again take into account other relevant factors, such as the effectiveness of other protections already in place and NHS capacity at the time.
The potential types of measures that are likely to be considered in each response category are set out in Table 1. Because we must ensure that any specific protective measure (e.g. a restriction on a particular type of setting or activity) is necessary and proportionate at the time it is applied, all of the information in the table would be subject to detailed confirmation at the relevant time. As noted, individual measures or groups of measures might be deemed appropriate – rather than the full application of every measure in each category. We nevertheless hope that this table provides a useful guide for future planning purposes by giving a broad sense of what type of protective measure might apply in what circumstances.

Whenever temporary protective measures are in place above the routine response level, we will keep them under regular review (e.g. every three weeks) and maintain a close watch on relevant direct COVID, broader health, social and economic indicators so that we are able to ease those protective measures as soon as it is appropriate to do so. We are likely to be monitoring a slightly different set of epidemiological indicators to inform judgements about easing measures, including:
- all available evidence to detect a decline in incidence and prevalence.
- a reduction in hospital and/or ICU bed occupancy.
As noted above, sometimes it may be appropriate to ease responses incrementally instead of jumping wholesale from 'category to category' according to ongoing threat assessment.
We expect that our responses to future threats would generally apply across the whole of the country simultaneously. However, any application of the measures would take into account their necessity and proportionality across the different geographies of Scotland, for example in relation to our island communities, at the relevant time.
Supporting Positive Behaviours and Adaptation
Notwithstanding the threat assessments and categories of response set out in the previous section, our aim should be to manage the virus on a routine - or at most enhanced protective measures - basis as far as possible. Adopting sensible behaviours and making basic, appropriate adaptations will help us to do so.
We must aim to live safely alongside COVID-19 if we can. This will require us to build a society able to balance various risks and it will involve an ongoing ask of the public and organisations to take responsibility for enhancing their safety. This includes embedding many of the protective behaviours and measures we have become so familiar with over the past two years. By doing so, we can lessen the ongoing risk posed by COVID-19 and help mitigate the impacts of more familiar diseases such as seasonal flu and other viruses. This will benefit everyone but would be of particular benefit to those at higher clinical risk.
This section describes our collective progress in terms of adhering to the protective measures that help keep others (as well as ourselves) safe before focusing in on two of the key areas of adaptation that will help us to manage COVID-19 effectively on an ongoing basis: improving ventilation and encouraging hybrid working where appropriate. It then outlines the role of the public sector, and particularly our local government partners, in supporting the positive behaviours and adaptations that we need to embed. And it outlines our communications and marketing work in this area.
Progress
The Scottish Government has continued both to support the public in adhering to rules and guidance, and to work collaboratively with local authorities, businesses, and other stakeholders to promote adherence to protective behaviours.
Since the previous Strategic Framework update, in November 2021, YouGov[23] polling shows continued strong adherence. In terms of self-reported compliance, levels remain relatively high and stable. In January/early February, as in recent months, around two thirds reported high compliance,[24] with over a quarter reporting 'complete' compliance (31% at 4-6 January and 28% at 1-3 February).
A fairly stable majority (65% at 1-3 February) said they feel clear about what is required of people in Scotland as the pandemic continues. Although there were some improvements in adherence to some of the protective behaviours when the additional measures/guidance were in place in early January, this was not sustained. However, levels of adherence are fairly similar now to those seen in November/ December last year. For example, 90% say they do well at wearing a face covering when required (78% very well), 85% say they do well at washing/sanitising hands regularly when out and about (54% very well) and 82% say they do well at avoiding crowded/busy place (48% very well). Levels for other behaviours are lower but also stable compared to November/December.[25]
The Scottish Government has facilitated ongoing stakeholder engagement at both Ministerial and official level with organisations across a range of sectors within the economy, the third sector, trade unions and regulatory partners. A key focus throughout has been on working with business on supporting improved adherence to baseline measures and taking the necessary regulatory actions, particularly in the face of Omicron, to better direct and support compliance from business settings by detailing the reasonable measures expected. Even as the regulatory underpinning reduces, we are committed to working with stakeholders to support safer working and resolve challenges through regular and open dialogue.
Next Steps
COVID-19 will not suddenly go away and it is likely that the virus will present us with further challenges over the months and years ahead. We can all play a part in reducing the risk posed by COVID-19 in a proportionate way; doing so collectively will help us all live safely and in a sustainable way.
Looking forward, we want to progress from people having to adhere to a set of rules that help reduce the spread of COVID-19 towards embedding a set of positive behaviours that people and organisations voluntarily undertake because they believe they are the right thing to do.
To help us to understand the challenges people face, and what action we can take to support people to address these challenges, we are exploring the establishment of a People's Panel. The Panel would enable us to explore the reality of personal responsibility and safer behaviours for people in a wide range of different circumstances. It would also allow us not only to monitor the challenges people are facing over time but also to understand elements that compound the challenges, and, crucially factors that could address these challenges. Working with the Panel would also help to provide us with in-depth understanding of how public health messaging is impacting on behaviour.
Organisations and businesses have changed substantially and invested heavily to create safer and lower-risk ways of working. While the temptation to return to a pre-COVID-19 way of operating may be strong in some parts of some sectors - and, of course, in many respects should be encouraged - the experience of the pandemic demonstrates the inherent uncertainty we will continue to face. To strengthen our long-term response to this virus, future variants and possibly other viruses ahead, we will lead the way in partnership with businesses and organisations to embed proportionate protective behaviours and create a framework for improved public health responses.
The Scottish Government will work with all sectors to support adaptation to enable Scotland's businesses, organisations and the public generally to be more resilient to future shocks. We will also develop business campaigns, clear and accessible Scottish Government guidance, update the compliance toolkit, and support voluntary action to help customers feel safe.
Businesses and other organisations recognise the positive steps taken during the pandemic and the need for them to have greater permanency in its aftermath – such as increased hybrid and flexible working, enhanced sanitisation and hygiene and improved ventilation within the workplace. Beyond this, engagement has started on longer-term adaptations to prepare Scotland to address future public health challenges – with consideration being given to: regulatory reform; business continuity and resilience planning; simplification and improved accessibility of guidance; public health training for employers and employees; and physical modification of premises to reduce the risk of infectious disease transmission.
Adaptation for businesses and other organisations
As set out in the section on Protective Measures most, if not all, COVID-19 legal requirements will no longer be in place when the threat level is low. However while there may be no legal requirements in place it will remain important for businesses to consider what they can do to help reduce the spread of the virus, protect their employees and customers and trade or operate fully in that different environment. These adaptations and behaviours help to keep the spread of the virus low but also provide confidence to customers. A recent survey showed clear signs that hospitality and retail businesses taking steps to make premises safer would make customers more comfortable (65%) and more inclined to visit (63%).[26] Making adaptations may also help businesses by minimising the disruption/ action required should a temporary move to increased protective measures be required.
Creating safer spaces for staff and customers is not an exact science and will vary by sector, premises and business model. However, businesses should consider some of the potential adaptations below in their own business contexts and taking account of their own risk assessments, which they should refresh regularly. We are aware that many businesses have already been adapting in some of these ways and will also have other adaptations which go beyond this.
Increased hygiene
- Ensuring hand sanitiser is available and encouraged to be used
- Ensure soap dispensers are in place and full in facilities
- Regular cleaning of tables etc.
Adjusting premises
- Improved ventilation, including mechanical ventilation where possible (see below)
- Altering premises including using outside spaces where possible
- Encouraging some distancing between customers and staff where possible
Adjusting behaviours
- Increased levels of hybrid working (see below)
- Support staff to isolate when symptomatic
- Encourage face coverings even when not mandatory
- Testing (when available and appropriate)
These measures are not exhaustive and other specific adaptations will help in particular sectors. We will work with sectors to help identify adaptations that work for them. They will help to reduce the risk of the virus and help to keep businesses trading by reducing the likelihood that further protective measures will be required when a new threat emerges. That likelihood cannot be removed entirely, however, and where further protective measures are necessary, they will be temporary and proportionate.
Ventilation and Healthier Buildings
The nature of COVID-19 means we all need to consider, on an ongoing basis, how we: use our buildings and spaces indoors; make more use of outdoor spaces; avoid crowding; and manage flows of people. Good ventilation helps reduce the risk of transmission indoors and even simple actions such as opening windows can be effective.
Progress
We have strengthened our main Ventilation Guidance in relation to carbon dioxide (CO2)monitors, air cleaning/purifying devices and the use of poorly ventilated spaces. We have invested up to £15 million to support this activity in our schools and early learning and childcare settings (this is on top of previous COVID-19 logistics funding of £90m that could be used for purposes including ventilation improvements). Guidance for schools has also been updated including strengthening of the required approach to ventilation and CO2 monitoring. Updated guidance for further and higher education has underlined the continued importance of good ventilation as a key mitigating measure on campuses.
Following our COVID-19 Ventilation Short Life Working Group's initial recommendations, funding of up to £25 million was identified to help small and medium sized enterprises (SMEs) in the highest-risk settings make adjustments to ventilation, including the installation of CO2 monitors and adaptive devices, improvements to natural ventilation and small repairs. The fund went live on 23 November 2021 and pre-work approvals have been given for CO2 monitors, air filter/purifiers, small mechanical ventilation and window repairs.
In taking measures to ensure our public buildings and businesses are as safe as they can be we need to do so in a way that supports our continued response to climate change and our journey towards becoming a net zero nation. We need to consider how we make adaptations to our buildings and spaces that are designed to keep new infections out and control those already present by limiting transmission. Building infection-resilience to keep us safe has never been more important. We will use learning from the pandemic to set out how buildings and settings should operate in ways that keep us healthy and safe, and provide us with good air quality and other protections.
In addition, good public health infection controls will be integral to the creation of safer indoor and outdoor environments. This includes good hygiene and how surfaces such as touchpoints (i.e. door handles) are adapted, to reduce the risk of infection.
Next Steps
- We will act to ensure that necessary improvements in ventilation will be proposed in light of the work of the Short Life Working Group on Ventilation who will provide their recommendations by the end of March 2022.
- We will continue to work across the four nations of the UK, UKHSA and international organisations to promote measures that support bio-secure environments.
- We will work with partners to develop, by the end of April, a pilot scheme that encourages those who manage buildings and settings, in the private and public sector, to display by way of signage the protective measures they have in place.
- We will review building regulations and explore how buildings of the future can have infection-resilience built into their designs.
Hybrid Working
Supporting staff to work from home, where possible and appropriate, has been an important mitigation in reducing the risk of transmission both in the work environment and during travel to and from work. It is set to remain as one of the ongoing behaviours that will help to manage COVID-19 effectively for the long term.
Progress
In addition to the public health benefits of working from home, a number of studies have noted perceptions of increased productivity among employees albeit contingent on technology/connectivity.[27] However, we also recognise that working at home does not come without cost to workers, employers and the broader economy, for example businesses reliant on office trade particularly in city centres. Wider research has noted that the absence of workplace interaction, breakdown of support networks, isolation and loneliness can cause negative impacts on social wellbeing. These points have also been made directly by businesses through regular engagement with the Scottish Government. We understand their desire to have staff back in the workplace some of the time and agree that employers and employees, in conjunction with unions, are best placed to establish what works best for them.
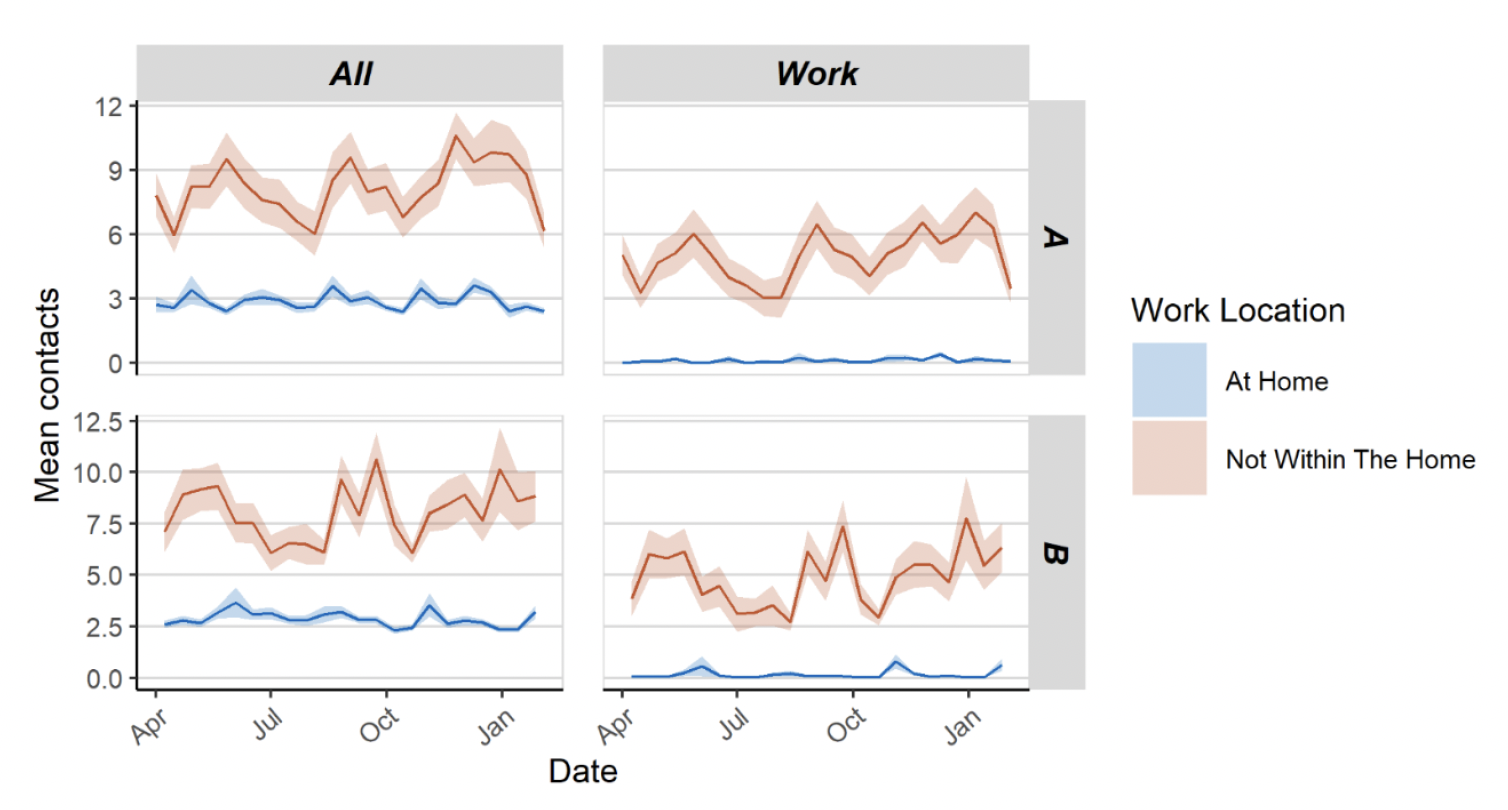
Figure 12 shows the difference in overall contacts and work contacts between those who work from home compared to those who have a workplace outside of the home. Those who do not work from home have higher and more variable contacts than those who work from home - average contacts for those who do not work from home are approximately 2 - 3 times higher than those who work from home. This also shows that contacts within the workplace make up the majority of overall contacts for those who do not work at home.
While many employers have already been engaging with employees on moving to a hybrid working approach, in line with what is appropriate for their business, customers and staff, we continue to encourage a greater degree of working from home than pre-COVID-19, where this is possible and appropriate. Employers have a legal duty to make workplaces safe and to conduct risk assessments; this is particularly important for those at higher risk. The needs of those in the highest risk category should be taken into consideration when planning hybrid working – including people who might prefer home working, or those keen to return to the workplace.
Next Steps
A wide variety of working models have been explored by organisations in consultation with their workforce, such as hybrid models of home and office-based working. Working from home remains an important mitigation in reducing the spread of the virus particularly when there may be more community transmission. We will continue to strongly encourage employers to work with their employees to consider, for the longer term, hybrid working models. These may of course have benefits that go beyond the need to control the virus and for organisational resilience such as attracting and retaining talent, supporting wellbeing, environmental benefits and the growth of local businesses outside of urban centres.
We recognise that employers are best placed to understand how their operations work most effectively and their employees' and requests for flexible working, based on consultation with staff and unions. We trust organisations to make balanced and risk-assessed decisions and we also recognise the need to consider the wider impacts working from home may have such as mental health, retail and investment in city centres.
We will continue to work with employer and business organisations and trades unions to understand the wider and longer term impacts of hybrid and flexible working as evidence and practice develops. This will help us to understand not only the economic and individual impact of hybrid working but the challenges and opportunities, the barriers to participation, the support available and recommended and where hybrid working supports our wider ambitions.
The Public Sector and the Role of Local Authority Regulators
We will work collaboratively with local government and other public sector partners to lead by example in adapting public services and spaces to be as safe as possible. There is an important role for encouraging and facilitating innovation, for example in more creative, safer and sustainable use of indoor and outdoor spaces.
Reflecting and learning the lessons of what has been most effective in supporting people, communities and businesses to adopt protective behaviours will be critical. Government at all levels will have an important role to play in capturing these lessons and maintaining the knowledge and capacity to respond to future challenges created by COVID-19.
We will continue to work collaboratively with the Convention of Scottish Local Authorities (COSLA), local authorities and other regulators who will provide critical insight into the adaptation work and the future approach to supporting safer behaviours. This includes learning and using their role as planning and licensing authorities to enable safer behaviours.
We will work with regulators to adapt our risk-based approach and ensure that they have the necessary resources to support the promotion of safer behaviours with adaptations normalised into our business communities, while having the necessary powers to address an increase in the spread of the virus at a national and local level where it poses a challenge to public health.
Communications
Scottish Government communications have supported public adherence and positive behaviours throughout the pandemic: providing vital public information on what is required as protective measures change, encouraging sustained behaviour change and delivering more targeted strands of activity to support specific audiences and needs.
Progress
November/December 2021 was a period when people were expected to be socialising and mixing more than normal. Vaccine immunity was diminishing for certain cohorts and infection rates remained high. The 'Living Safely' communication strategy - developed from audience insight and designed to help establish a longer-term social norm for protective behaviours – was already in place. With the arrival of Omicron it was adapted to be more directional and to reflect the updated asks of the public. It was delivered through the 'Living Safely This Winter' campaign, focusing on the behaviours we all needed to adopt over the festive/winter period to protect each other and stay safe.
Supporting materials were sent to businesses in advance of the main campaign and marketing campaign toolkits were deployed through public sector, third sector and private sector networks to reflect 'Living Safely' messaging. A number of other communications campaigns supported the public during the winter period, including:
- Right Care Right Place: to help the public access the healthcare they need through the right channels.
- An education campaign: to promote the importance of both ongoing testing and testing prior to returning to places of education in January 2022 (delivered via social media platforms, Parent Club and Young Scot).
- A number of COVID-19 recovery campaigns including ongoing activity to provide practical and positive advice to the general public about how to look after their mental wellbeing during the pandemic and a 'Tenancy Rights' campaign to protect renters from eviction and mistreatment.
Next Steps
Opinion polling in January and February[30] showed a continual increase in optimism among the general public from the situation in December, and at 45% (4-6 January) there was slightly more positivity about the year ahead than seen in January 2021 (40%). Although decreased to the lowest level seen, around two-fifths were still worried about the situation (43% at 1-3 February), and the wider impacts (anxiety, loneliness, effect on mental health, financial worries) were still much in evidence.
Qualitative research carried out on 11 January[31] made clear the fatigue and weariness that is felt, both with the pandemic and ongoing protective measures. However, this research also suggested that many people are generally accepting of the need to continue to adopt certain protective behaviours while COVID-19 poses a threat - seeing them as commonsense, practical actions that enable life, as they would like it, to carry on.
Opinion polling on 1-3 February[32] confirmed the qualitative findings: 76% agreed that they are happy to follow some rules and guidance if that means they can do the things that matter to them, while only 11% disagreed. This audience insight and qualitative feedback confirmed that the 'Living Safely' communication strategy remains powerful and valid. In the short term this is being delivered through 'Living Safely for Us All' which reinforces the importance of adopting the key behaviours on a sustained basis – to establish a safe positive norm of living safely with COVID-19.
The vaccine booster campaign is also live across a range of channels to encourage those (in targeted groups) who have not yet had it to come forward for their booster. Further work to support segments of the population as the pandemic continues and to help them do their best to adapt to the challenges it presents will also be delivered through:
- Ongoing activity to support positive mental health, including development of a new online resource.
- The Supporting Parents of Teens campaign, developed to help parents and carers support their teens though common emotional challenges, many of which have been exacerbated by the pandemic.
- Further phases of the Money Support Scotland campaign, designed to address systemic inequalities made worse by COVID-19 - signposting to trusted partners able to offer free, impartial financial advice.
We will supplement these campaigns with communication through social media, press briefings and wider communication channels from government and partners.
For the longer term, the 'Living Safely' communication strategy is under review and will be updated. Based on audience insight, the adult tone reinforcing behaviours by providing the rationale for doing them, which is currently in use, will continue to form a core part of the approach. The focus will be very much on embedding the required behaviours into our everyday lives using clear and simple messaging to help the public understand what they can choose to do and why. Any future activity will be informed by ongoing research and evidence. There also continues to be a focus on developing and improving content on the Scottish Government website to support public understanding of, and compliance with, public health guidance.
Communications will also support the wider COVID-19 recovery, and collaboration with organisations such as Scottish Enterprise, Young Scot and Black and Ethnic Minority Infrastructure in Scotland will continue, as will engagement with a range of organisations that can help to disseminate messaging to those they represent.
Helping to Manage COVID-19 Internationally
Progress
Following a review of the international travel requirements, the four nations agreed on 24 January to reduce and simplify requirements for travellers entering the UK. The main changes came into force on 11 February. The changes mean that eligible 'fully vaccinated' travellers are no longer required to take any tests before travelling to, or after their arrival in, the UK, and only have to complete the Passenger Locator Form (PLF) beforehand. For international travel purposes, 'fully vaccinated' means having completed a primary course of the vaccination. The PLF is to be simplified by early spring 2022. All children under 18 benefit from the same privileges as 'fully vaccinated' adults, regardless of their actual vaccine status.
Protective measures have also been eased for unvaccinated passengers, who are now required only to complete the PLF, take a pre-departure test and book a day two PCR test. Additionally, they will no longer have to self-isolate upon arrival in the UK.
Next Steps
While there are currently no countries on the red list of highest risk countries and territories, the UKHSA continues to monitor international data and will escalate any concerns to the four nations in line with a revised agile global scanning risk assessment process. Further consideration will be given in late February/early March to alternatives to Managed Quarantine Service hotels for any travellers arriving from a country that is on the red list in future.
The next phase of the review of international travel measures will focus on what the response should be to the identification of a future variant of the virus. This will include the definition of 'fully vaccinated' in an international context and the development of a border contingency toolkit being carried out by the UKHSA. We will continue to seek clinical input, and discuss on a four nations basis, before making any changes.
The UKHSA has recently updated its risk assessment methodology for Border Surveillance. It will continuously monitor threats, but will now provide summary reports for UK Government departments and Devolved Administrations on a fortnightly basis, or faster if any particular concerns come to light.
In the longer term, the UK aims to enhance global surveillance capabilities to maximise detection of variants. This includes working with the WHO and other public health bodies on the International Pathogen Surveillance Network (IPSN), supporting a small number of regional hubs and countries bilaterally to build genomic sequencing capability and capacity (New Variant Assessment Platform, NVAP) and continuing to offer rapid sequencing capability where needed. Scottish Government Ministers are committed to working with the UK Government, other Devolved Administrations, and delivery partners in developing robust surveillance architecture.
We will retain robust contingency plans for new variants which present significant risk to public health. To inform our longer-term strategy we are working on a four-nations basis with business and other stakeholders to move away from a 'one-size-fits-all' red list approach to a more agile set of contingency measures for dealing with reasonable worst-case scenarios, based on analysis of the advantages and disadvantages of previous measures. This review will also explore options to move away from relying on managed quarantine hotels to a home isolation model.
International Vaccination
We place great importance on Scotland being a good global citizen. Since the start of the pandemic we have worked with our partner countries in the Global South to support their response to the pandemic.
Progress
We have invested £3.5 million of our International Development Fund in COVID-19 response initiatives in Malawi, Rwanda, Zambia and Pakistan. We have provided support for vaccine preparedness, delivery, distribution, roll-out and online healthcare education to counter hesitancy through UNICEF, who work in conjunction with our partner country governments. In 2021 we also provided oxygen concentrators and ventilators to our African partners to support their COVID-19 responses and additional supplies of medical equipment and products, including vital Personal Protective Equipment (PPE) through the NHS Scotland Global Citizenship Programme. In addition, we funded an oxygen plant facility installed at Chitambo Hospital, Central Province, Zambia, with provision for all clinics and health centres in the surrounding area.
We continue to support collaboration between the University of Glasgow's Immunology Department and the Kamuzu University of Health Sciences in Malawi, including new COVID-19 funding in 2021 for immuno-phenotyping and genomic sequencing, which will help to identify new variants and improve disease control.
Next Steps
We will:
- Offer to share Scotland's experience in delivering a mass vaccination programme with the Governments of Malawi, Zambia and Rwanda.
- Provide crucial COVID-19 medical supplies to partner countries wherever we can to support the treatment of the illness.
- Provide multilateral partners with assistance to ensure effective vaccine programming in our African partner countries, including a £1.5 million contribution to UNICEF in this financial year specifically to target support for COVID-19 vaccines.
- Work in collaboration with multilateral agencies and partners in the Global South to call for improvements in vaccine equity globally, and continue to invest funding in initiatives to support equitable access to COVID-19 vaccines in Sub-Saharan African partner countries.
Supporting People at Highest Risk and Reducing Health Inequalities
A key element of our overall strategic approach going forwards must be to support and protect people who are at higher risk from COVID-19 – either because of their own health conditions or because they are less able to take preventative measures. Related to this we must ensure that we have both effective Personal Protective Equipment available and Infection Prevention and Control procedures in place. More broadly – over the medium to long term - we can help the population to become less vulnerable to serious health harm from COVID-19 if we can reduce some of the long-standing health inequalities, which is where many of our current efforts are focused.
Supporting People at Highest Risk
Throughout the pandemic we have provided bespoke advice, information and support to help protect the approximately 180,000 people identified as being at highest risk from COVID-19.
We must adapt to living with COVID-19 while remembering that those who have been on the Highest Risk List may need more time, care and consideration to get back to a more normal way of life. There is strong evidence to show that the vaccine is offering significant protection and preventing people on the highest risk list from becoming severely ill if they are infected with COVID-19, however understandably many may feel particularly fearful about what adapting to 'living with the virus' means for them.
We know that many people, who may be at higher risk or more anxious, may be worried as we lift restrictions. Therefore, we will for the time being continue to provide guidance and support to those who may feel more vulnerable, and communicate that, for many people initially considered to be at highest risk from COVID-19, that is no longer the case.
Given the wide range of circumstances and health conditions of people on the Highest Risk List, ensuring personalised advice and support is available to each individual on the list is an important part of this transitional period. GPs and clinicians who best know the circumstances of those people at highest risk will continue to be the first port of call for individual clinical advice. For some time now, we have advised people on the Highest Risk List to follow general population-wide advice and guidance unless advised otherwise by their clinician, and we will now consider if people need to continue to be on a Highest Risk List.
Progress
Our successful vaccination programme has helped us prioritise and protect vulnerable groups, in line with JCVI guidance. This includes over 90% of the people with severe immunosuppression who received a third dose prior to their booster so they could reach similar levels of protection to the general population. We will continue to communicate how people's risk has changed as a result of the vaccination programme and Omicron causing less severe illness across all groups.
As a Government, we have regularly engaged with people at highest risk since the pandemic began to understand the specific needs and considerations of this group, and more than 13,000 highest risk individuals responded to our most recent survey by Public Health Scotland.
Having listened to people on the Highest Risk List we have launched a scheme to allow anyone who feels anxious to signal to others that they would like extra space and care taken around them in public places. The Distance Aware scheme was developed by the Bevan Commission and adapted by the Scottish Government as a voluntary initiative designed to complement any other protective measures which remain in place. It is open to anyone who feels this would give them greater confidence for whatever reason when they are out and about in public places and the workplace.
We know that the mental and physical health of people at highest risk from COVID-19 has been particularly affected, which is why we are working to develop support for those who need additional help to recover, to reconnect with people and things they were doing before the pandemic, and to benefit from the lifting of protective measures.
We are also asking employers to consider the individual needs of people on the Highest Risk List as they implement hybrid working models. We have developed workplace guidance specifically for people at highest risk, including employer responsibilities, at mygov.scot/covid-highest-risk/work.
Many people on the Highest Risk List, including people who were asked to shield in the early stages of the pandemic, have told us about how isolated and lonely they have felt. We have funded a free support service run by the British Red Cross, called Connecting with You. It is available to all people aged 18 or over in Scotland who are experiencing issues associated with loneliness and helps people to rebuild their independence.
Next Steps
We will continue to ensure people at highest risk know where to turn if they need further guidance. Clinicians and GPs will continue to provide advice tailored to the personal circumstances and conditions of each individual on the Highest Risk List as they would have before the pandemic. We will:
- provide further advice and information to support this group, particularly on issues related to mental health and loneliness;
- working with our Clinical Advisory Group, to provide support to those who no longer need to be on the list where the evidence indicates that they are no longer at highest risk; and
- continue to respond to scientific and clinical advice regarding COVID treatments, making sure that those who we know will benefit most from them are able to access them; and,
- continue to look at ways to identify and support people who may be at highest risk, taking into account potential new variants and emerging evidence.
Our aim is to ensure that people who have been on the Highest Risk List are supported, empowered, and included throughout this calmer period into a more normal way of living. It has been nearly two years since we asked people to shield, and it is crucial that they are now supported to benefit from the lifting of restrictions as much as everyone else.
Adult Care Homes
People living in adult care homes, many of whom are older and/or are living with multiple long-term medical conditions, have been severely affected by COVID-19 due to the high risk of exposure to infection and higher clinical risk of severe disease and mortality. In response to this higher risk, a range of protective measures has been recommended to limit the spread of COVID-19 including those on visiting in and away from the home. The non-COVID harms from these protective measures include diminished mental wellbeing, reduced mobility and lack of family connection.
People living in care homes, which are essentially their homes, should be supported to enjoy fulfilled, meaningful lives free from restrictions as far as possible. Even during outbreaks, unless there are exceptional circumstances, the care home should support residents seeing friends and family and participating in activities in and away from the home. Where protection measures do need to be in place these should be proportionate and only be in place for the shortest possible period.
The ongoing response to COVID-19 will need to provide flexibility for local responses to outbreaks, and support effective and consistent risk assessment that balances the risks from infection with the harms caused by restrictions, and the wider impact on the system of care home closures.
Reducing risk and improving outcomes in care homes will depend heavily on enablers of workforce, technology and data, and ethical commissioning. That will be essential for the sector as it recovers and renews from COVID-19 and looks to the future with the creation of a National Care Service.
Progress
Policy and guidance to support care home residents and staff are based on clinical evidence around the risk to people in vulnerable settings. At the start of the Omicron wave, a number of precautionary protective measures were introduced including daily LFD tests for staff in care homes, household limits on visitors and continued promotion of vaccination including boosters, which will have contributed to a lower rate of transmission and death compared to previous waves (booster uptake for care home residents is currently at over 90%).
The named visitor policy during COVID-19 outbreaks has been implemented with growing support from the sector, and this has assisted the wider implementation of Open With Care visiting guidance and also ensured that the majority of care homes continue to support visiting during the Omicron wave.
Challenges remain and the harms associated with restricting visiting and other routine activities have influenced the recent decision to remove precautionary self-isolation for care home residents on admission to care homes who have not had COVID-19 or not been a contact, and to reduce isolation periods for residents who are COVID-positive or have been a contact from 14 to 10 days.
However, there remain some protective measures in care homes which differ from the general population. This is due to evidence of increased risk to those living in a communal setting where many individuals are living with frailty or multiple long-term medical conditions or are elderly with an immune system that is less effective against COVID-19.
Nevertheless, we want care homes to return to normality as soon as possible so it is important that any protective measures are reviewed regularly, with the aim of bringing them into line with those for the general population.
Next Steps
The future management of COVID-19 in care home settings will continue to build on what has been learned about the critical importance of infection prevention and control (IPC) and PPE, and the benefits of vaccination. Having a proportionate response that reduces harms to wellbeing and health, will help to ensure that care home residents are supported to live their lives as free from restriction as possible.
We will improve healthcare outcomes for care home residents by developing, delivering and facilitating the implementation of a new healthcare framework led by our Clinical and Professional Advisory Group (CPAG) for adult social care. It will be a blue print for the health and care system that will focus on prevention, anticipatory unplanned care through to palliative care, and will take account of the evolving impact of COVID-19 for the foreseeable future. A critical enabler will be the effective and seamless working of multiple-disciplinary teams that put people at the centre.
Health outcomes for people with learning disabilities have been particularly affected by COVID-19. A new subgroup of CPAG will explore how to support care homes and other settings to improve outcomes and reduce ongoing risk from COVID-19 and associated harms.
We will work with PHS and ARHAI Scotland (Antimicrobial Resistance and Healthcare Associated Infection) to agree thresholds for declaring outbreaks, with a national risk assessment tool that supports consistency and confidence in local decision-making. It will also provide transparency for those working in the sector, residents themselves and friends and families. We will continue to learn from the experience of preventing and managing outbreaks through a follow-up exercise to the Root Cause Analysis report published in November 2020.
We will work with ARHAI Scotland, NHS Education for Scotland (NES), Scottish Social Services Council (SSSC) and the Care Inspectorate to ensure the workforce has the right tools, training and support to adopt the IPC standards.
We will work to ensure that residents are supported to see the people who are important to them and to participate in activities within and outwith the home. In addition we will continue to implement our commitment to deliver Anne's Law through the following non-legislative and legislative measures. These include:
- working with the Care Inspectorate to update and strengthen the Health and Social Care Standards and have proposed two new standards with a strong focus on choice and visitation rights; and
- continuing to work with stakeholders on the Open with Care visiting guidance to emphasise that visiting should be as normal as possible.
We will continue to promote and monitor vaccination, including boosters, for residents and staff. Social care staff should also receive a vaccination for flu on an annual basis. We will review testing arrangements for staff in care homes and review isolation periods for care home residents who have COVID-19.
Infection Prevention and Control
Progress
Infection Prevention and Control remains an important part of our management of the virus. We developed guidance in a responsive manner with rapid literature reviews of evidence conducted by NHS Services Scotland Antimicrobial Resistance and Infection Prevention and Control (ARHAI) and supported by the Clinical Nosocomial Review Group (CNRG) commissioned by the Chief Nursing Officer.
The existing National Infection Prevention and Control Manual (NIPCM) was supplemented by additional addenda for specific health and social care settings. These were revised to become a single Winter Respiratory Infections Addendum.[33]
Infection Prevention and Control guidance was developed on a UK four nations basis and reflected in our own Scottish guidance.
The pandemic demonstrated a need for enhanced IPC in community settings and in acute settings, with some aspects of routine surveillance and monitoring being paused to allow staff to focus on meeting the IPC needs required by the whole health and social care sector.
Provision of PPE was initially challenging both in supply and in staff knowledge of its use. We worked collaboratively with ARHAI to support a range of policy areas with IPC expertise to inform decisions on appropriate PPE requirements and education to support its use. We worked with ARHAI, the Care Inspectorate, Healthcare Improvement Scotland and staff to support education and communication regarding COVID-19 modes of transmission and PPE requirements through the use of webinars, posters and social media campaigns.
Next Steps
With a largely vaccinated population and with further treatment options available to us, the level of risk presented by infection with the virus reduces. ARHAI will withdraw the Winter Respiratory Addendum and return to the NIPCM and business as usual. We have proved that we have the expertise and ability to respond quickly to changing levels of threat posed by this and any other potential infection should the need arise.
We will continue to work on a four nations basis to inform and develop IPC guidance for Scotland. We will continue to develop policy and guidance for health and social care settings in a collaborative manner with ARHAI, PHS, Occupational Health, PPE policy unit and others.
We will seek to use sound IPC principles as an enabler to safe and compassionate care wherever it is delivered. We will ensure that IPC guidance and access to IPC expert support is available across health and social care. This will be especially critical as we develop a new National Care Service.
We will refocus on reducing avoidable healthcare associated infections and antimicrobial resistance through resumption of surveillance and quality improvement programmes. We will work with colleagues to reduce avoidable harm through inappropriate or over use of PPE. We will work with NHS Education Scotland to strengthen IPC knowledge in the workforce at all levels. The learning we have gained through the pandemic will inform future service design and even the design of the buildings we deliver services in.
Personal Protective Equipment (PPE)
The Scottish Government will develop, throughout 2022-23, a new approach to how the public sector procures and supplies PPE in Scotland, with this coming into operation in 2023.
We will plan for new approaches to pandemic PPE which will ensure that we learn from experience, promote innovation, and have strong, sustainable foundations for any future epidemic or pandemic. To ensure that we are prepared for any future requirements for PPE, we will:
- ensure future PPE pandemic supply and develop a strategy to ensure Scotland is ready for a future pandemic whenever it may occur;
- work to protect the new Scottish PPE manufacturing capacity and capability;
- oversee the implementation of positive changes to the provision of PPE in Scotland and make PPE more sustainable;
- work to minimise wastage and maximise the benefit of PPE purchased; and
- ensure all areas have considered the lessons learned, and apply this knowledge throughout the work being undertaken.
Reducing Health Inequalities
As Scotland emerges from the COVID-19 pandemic we urgently need to address the pre-existing health inequalities that have been exposed and exacerbated. The pandemic has produced uneven impacts across a range of outcomes for a number of groups. These include households on low incomes or in poverty, low-paid workers, children and young people, older people, disabled people, minority ethnic groups and women. These groups also overlap, which may compound the impacts for some.
We have a national mission to increase how long people in Scotland live in good health, focusing on those facing the most disadvantage. We need to do much more to support people in the most deprived areas, where healthy life expectancy is 24 years lower than in the least deprived.
Reducing health inequalities is therefore at the heart of our COVID-19 Recovery Strategy. It is also a key consideration in the remobilisation and redesign of our health and social care system. So as we renew and recover as a society, we will ensure the necessary resource is directed at addressing health inequalities and their underlying causes.
Our inclusive COVID-19 vaccination programme and our inclusive approach to Test and Protect are both examples of where we have built strong foundations that will contribute to enhancing our public health response and ensure it is equipped to continue managing COVID-19, support our recovery from it, and address longer-term population health challenges. But there is more to do and we will grasp the opportunity to address many of the deep rooted health inequalities COVID-19 has exposed. Work on enduring transmission will have an important role in the understanding of factors leading to, and possible mitigations of, enduring transmission in Scotland to reduce inequality impacts.
The impact of the pandemic is driving increased demand and complexity across all services and particularly in the most deprived areas. General Practice supports people in hearts of communities who may not be in touch with other services. It has a unique and key role to play in addressing health inequalities and tackling child poverty: improving population health and employability
We plan to build on our policies of providing social and financial inclusion support and advice under the General Practice roof (through Community Links and Financial inclusion Workers) through the work of the Primary Care Health Inequalities Short Life Working Group.
Taken together, this work will support patients experiencing multiple and intersecting socio-economic inequalities to improve health and wellbeing outcomes and employability.
We are taking bold population-wide approaches to reduce the significant harms of tobacco, alcohol and unhealthy food and drinks. Examples of this include:
- Bringing forward legislation to restrict promotions of less healthy food and drink
- Tackling alcohol consumption and harms, particularly among high-risk groups
- Developing a refreshed Tobacco Action Plan and continue to provide £9 million a year to health boards to fund smoking cessation services in the most deprived areas
- Doubling investment in sport and active living to £100 million a year by the end of the Parliament ensuring more people can enjoy active lives, improving physical, mental and social health.
We are also tackling inequalities in the uptake of health screening. Screening is one of our most important prevention tools, so it is vital that everyone who is eligible to take part has a fair opportunity to do so.
We recognise that factors that impact on people's health and wellbeing go beyond what the health and social care system itself can deliver. Understanding that socioeconomic inequalities drive health inequalities, our public health efforts are complemented by wide-ranging cross-government action. This includes actions to end poverty; increase fair access to employment, education and training, and improve our physical and social environments.
An intelligence-led approach to tackling racialised health inequalities
Minority ethnic groups have been disproportionately affected by the economic impacts of the pandemic because of their employment and household circumstances.[34] Minority ethnic people are also at greater risk of severe illness and death from COVID-19. Analysis in November 2021 showed that compared to people with White Scottish ethnicity, deaths amongst people with Pakistani ethnicity were 3.7 times as likely to involve COVID-19. Inequalities were also found for people with Chinese ethnicity (1.7 times as likely), Indian ethnicity (1.7 times as likely) and Other Asian ethnicity (3.0 times as likely).
We are determined to show leadership and address the systemic racialised inequalities. We also know that we need focused and robust actions. Improving equity in healthcare for minority ethnic groups has been at the heart of our work since the pandemic began. In response to the emerging evidence on the uneven impacts of COVID-19 on minority ethnic communities, the Scottish Government convened an Expert Reference Group on COVID-19 and Ethnicity. The Group provided advice and recommendations on data, evidence, risk and systemic issues. In September 2021, the Scottish Government published its Race Equality Immediate Priorities Plan setting out an 18-month work plan to ensure that minority ethnic communities have a fair recovery from the pandemic.
Good progress has already been made on several of the health focused commitments within the Plan. In particular, we have made significant strides to embed inclusion into our COVID-19 vaccination programme as well as our future vaccination and immunisation programmes. This includes ethnicity data being collected which will further support the planning of services and outreach.
Within Scotland, improvements are needed in ethnicity data quality in order to accurately assess the impacts of COVID-19 on minority ethnic populations. Further work is underway across Government to improve the collection and use of ethnicity data to better understand and address inequities in health access and outcomes for minority ethnic communities in Scotland.
A place-based approach to tackling inequalities at local level
We are working with local communities to cultivate person-centred approaches aimed at preventing ill health and reducing inequalities by addressing their root causes. By making smarter use of public health data and our public health workforce we can inform local level decision making. This will ensure that, together, we can improve the health and wellbeing of communities who experience the greatest inequalities. This will include supporting our health and social care providers to become active 'anchor institutions' and build wealth in their community. We are looking to embed community-led health improvement into local public services through, for example, social prescribing.
We are exploring how to wrap services around families and developing a model of family support based on integrated multi-disciplinary teams. These teams will provide accessible drug and alcohol services, community mental health services and family support wrapped around Deep End GP practices alongside support to help people enter and remain in employment.
Mitigating Broader Harms and Supporting Recovery
This section of the Framework outlines action to support both the mitigation of harm and broader recovery across our businesses, health and social care, and other public services. The information set out below is not exhaustive and highlights progress and next steps across a number of areas of activity that are being developed in further detail within our COVID-19 Recovery Strategy.
Business
Progress
Since the start of the pandemic, we have worked with businesses to support them through some of the most challenging times, during which the need to reduce transmission of the virus affected their ability to operate. We recognise that businesses across Scotland have gone above and beyond in adapting to the challenging circumstances brought about by this global pandemic in order to reduce the risk to their staff and customers.
To date, businesses have benefitted from more than £4.4 billion in support from the Scottish Government. This includes direct grant funding to businesses that were closed or required to change their operations while restrictions were in place, and targeted funding for businesses in sectors most significantly impacted.
It also includes COVID-19 non-domestic rates reliefs which have saved businesses around £1.6 billion in reduced rates bills since 1 April 2020. The Scottish Government has offered 100% COVID-19 rates relief for the past two years without any cap, and we were the only government in the UK to do so. We are preventing a cliff edge return to full liability for businesses in the retail, leisure and hospitality sectors on 31 March 2022, by continuing relief at 50% for the first three months of 2022-23, capped at £27,500 per ratepayer, which will help businesses recover.
To date we have spent almost half a billion pounds more in support of Scottish businesses than the funding we received from the UK Government for that purpose.
Throughout the pandemic we have revised and streamlined guidance working closely with sectors affected. Since the move beyond Level 0 in summer 2021 we have removed much of the sectoral guidance and instead focus primarily on one set of safer workplaces guidance.
We have also included all businesses in Scotland with 10 or more employees in workplace testing. Any business enrolled in the scheme can access free LFD tests. More than 750 businesses have signed up for workplace testing in Scotland, covering approximately 120,000 employees.
Next Steps
The Scottish Government committed a further £375 million support package for businesses impacted by the necessary measures introduced to control the spread of the Omicron variant. This package includes £200 million reprioritised from the Scottish Government's expected consequentials budget and £175 million made available by the Treasury.
From this funding package, £80 million has been allocated to the COVID Economic Recovery Fund. This will give councils the flexibility to target funding to their local businesses and communities and will support economic recovery across the country as we move to a new phase in the pandemic.
There is currently no budget cover in financial year 2022-23 for further business support, so providing similar support if future restrictions were introduced would require additional funding from the UK Government to be made available.
Many businesses have already made changes to the way they operate to reduce the risk of transmission including changing the physical layout of their premises, making use of outdoor spaces and reducing the risk of crowding.
We know that improved ventilation can make an important contribution to reducing the risk of transmission, and we have made £25 million available through the Business Ventilation Fund to help businesses with the cost of improving ventilation in their premises.
Businesses more likely to be affected by temporary protective measures, should harmful variants occur, may need to consider the impact of reduced revenue at times as part of their planning.
We will continue to refine guidance based on the current position, providing clarity on what is expected of businesses so they can plan effectively.
NHS Resilience
The NHS has experienced significant pressure as staff have worked tirelessly to deliver care and treatment to the people of Scotland. The focus has been on: maximising capacity; improving outcomes for patients; caring for staff and improving access to and discharge from hospital. Our NHS will remain ready to adapt and respond to COVID-19 while taking forward work to deliver recovery.
Progress
The NHS Recovery Plan was published in August 2021 and will be the cornerstone of our work to respond to the significant non COVID-related health and social care needs which have continued to build up over the last two years. A key aspect of our recovery will be accelerating innovation and the transformation of services supported by the Centre for Sustainable Delivery.
Within the NHS Recovery Plan key actions are set out that will support recovery through:
- maximising staffed capacity in hospitals and community services by continuing to extend the redesign of urgent care and hospital at home, increasing the availability of self-care with remote monitoring and digital technologies;
- increasing workforce through recruitment; improving education, training and development, including the accelerated recruitment of 1,500 additional staff for the National Treatment Centres;
- extending and optimising planned care capacity, to tackle the growing backlog in elective and cancer treatments as well as diagnostics, including endoscopy services, as set out in our recent Endoscopy Plan;
- innovation and redesign of services to help staff deliver high quality care and treatment by allowing more people to manage their condition at home and to be able to carry out pre and post-operative assessments remotely; and
- increasing the use of digital technology to enhance accessibility to services.
The Plan also sets out how we will create transformational and lasting change in mental health services, across acute and primary care sectors including investment to expand capacity in Child and Adolescent Mental Health Services (CAMHS); scaling up new digital treatments and therapies to ensure these are also accessible in rural areas; and expanding access to frontline services which benefit people with dementia and their families after a diagnosis.
In primary care, in addition to our existing commitment to deliver 800 additional GPs by 2028, we will support the extension of Board-delivered pharmacy and nursing support in all 925 of Scotland's General Practices to help to alleviate pressures on GP services while ensuring we all get the care and support we need from a qualified professional.
While we have made some progress, the recent wave of Omicron has impacted on the NHS Recovery Plan and we will work closely with our NHS Boards and their social care partners to deliver on the key priorities.
That transformation work will sit within and alongside a longer-term comprehensive programme of reform being taken forward through the Care and Wellbeing Portfolio and its four constituent programmes: Integrated Planned Care; Integrated Unscheduled Care; Preventative and Proactive Care; and Place and Wellbeing. This programme is being designed, in collaboration with partners across the public and third sectors, to respond to the impact but also the opportunities that have arisen during the pandemic. To deliver a more sustainable health and care system it will focus on improving population health and tackling inequalities and not just dealing with symptoms.
Next Steps
We will take the learning from the response to the recent wave of COVID-19, and nurture and support the creativity and innovation of our staff, to deliver improved resilience and long-term sustainability across our health services.
Work on technology enabled care and the development of virtual capacity has been developing rapidly and offers benefits in terms of both immediate resilience and longer-term recovery. There are a number of community-based pathways currently under development, including remote health monitoring services designed to help as many people as possible to safely manage their COVID-19 symptoms at home, supporting early detection of deterioration and reducing pressure on hospital bed capacity.
A key element will be taking forward the work on delivering care as close to home as possible, moving more acute care and support beyond hospital walls, supported by a programme to expand and increase Hospital@Home services. Working with Healthcare Improvement Scotland, we will be providing support to 20 partnerships to start or expand Hospital@Home over the coming months. The Hospital@Home model reduces the disruption to patients' existing formal and informal care and support arrangements through the addition of acute-level care delivered by multidisciplinary teams of healthcare professionals in patients' homes.
Combined with existing programmes, such as the Interface Care programme that aims to avoid unnecessary admission by optimising ambulatory care and Redesign of Urgent Care, these innovative approaches will enable the NHS to adopt a more flexible response to fluctuations in demand and ensure care is delivered as close to home as possible.
Investment in support for staff wellbeing is an essential and vital component of recovery. We are supporting: a National Wellbeing Programme, including a dedicated hub and helpline; Workforce Specialist Service and psychological interventions and therapies; along with time and training for staff to support each other as teams, and practical support like rest spaces.
Alongside compassionate leadership, we also recognise that staff working in specific areas may need more tailored support and work is under way to meet the particular needs of staff in areas such as intensive care, nursing, primary and social care.
Primary Healthcare
Progress
Nine out of ten contacts with Scotland's healthcare services are with primary care services. General practices, community pharmacies, dentists as well as NHS24 and the Scottish Ambulance Service are working tirelessly to meet people's needs. To support these services to meet the increased demand:
- We have provided £15 million sustainability funding to GP practices to support effective hybrid working including more face to face, extra GP sessions and practice nurse time to help clear the backlog.
- We are investing an additional £20 million in dentistry through increased fees to incentivise dentists to see more patients as well as £5 million of funding for ventilation improvements and £7.5 million for the purchase of new dental drills.
- We are rolling out the Pharmacy First Service designed to encourage everyone to visit their community pharmacy as the first port of call for all minor illnesses and specific common clinical conditions.
- We have provided investment of £20 million to help the Scottish Ambulance Service to increase service capacity, improve response times and improve staff wellbeing.
- We have provided increased funding of £20 million to NHS 24 to help the service to increase its workforce as a result of the increased demand and changing service that it provides, including a new call centre in Dundee which opened in December 2021.
Next Steps
As we move into recovery, primary care services will focus on sustaining high quality services, supporting more integrated working with other health and social services, offering more care closer to people's homes and reducing health inequalities. We will do this through:
- Investing £170 million in 2022/23 to provide patients with easily accessible support from a wider range of healthcare professionals through their general practice such as pharmacists, community nurses and physiotherapists.
- Stepping down the COVID-19 Community Pathway from the end of March. Acknowledging the impact this will have on GP practice workload we will continue to support Practices as they manage acute COVID cases. For now, the GP Escalation Framework will remain in place and a further £15 million sustainability funding, announced in November 2021, will be made available this year
- Delivering up to £40 million a year for accessible mental health support directly through doctors' surgeries, providing support needed early and reducing specialist intervention later on.
- Taking further innovative action to prevent ill health in our most vulnerable citizens, flowing from advice of our primary care experts group on tackling health inequalities.
- Developing and introduce a new pharmacy woman's health and wellbeing service providing greater access to advice, guidance and treatments for conception, contraception and menopause.
- Investing upwards of a further £6 million to support patient access to dental services locally in 2022/23. We will also increase the ChildSmile in the community programme, providing an additional 41 Dental Health Support Workers nationally to support our work in minority ethnic communities.
- Delivering a more consistent model of NHS community eyecare and audiology services. This includes a National Community Glaucoma Service to safely manage lower risk glaucoma outside of hospitals, a National Low Vision Service, and Community Audiology Service to help ensure everyone can get the help they need to cope with sight and hearing loss when they need it. These services will be piloted in 2022/23 and fully rolled out over the course of this Parliament.
- The increase in NHS 24 staff will also help NHS 24 to play their part in the Redesign of Unscheduled Care. Currently, people who feel they may need to attend A&E but whose condition is not immediately life threatening are being asked to use the 111 service.
- Supporting the Scottish Ambulance with their Demand and Capacity review. The investment of £20 million to support this will result in almost 300 new ambulance staff by April 2022, a mixture of paramedics, newly qualified paramedics (NQPs) and technicians. New and extra ambulances and associated vehicles will also be introduced in the coming months.
Mental Health
Progress
The past two years have tested the resilience of everyone in Scotland. There will have been very few of us who did not, at some stage, feel a strain on our mental health. It is crucial to understand that the mental health impacts of such a traumatic time will continue to emerge and evolve. The longer-term mental health effects will continue to be felt by many of us, across various levels of need. This will include mental ill-health in some cases.
Our Transition and Recovery Plan was published in October 2020 and set out our strategic response to the mental health effects of the pandemic. It contains over 100 specific actions, and is supported by a £120 million Recovery and Renewal Fund. This will transform services, with a renewed focus on prevention and early intervention.
The actions laid out in the Plan were based on data and evidence to help us identify where targeted action was required including:
- The Institute for Fiscal Studies (2020) reported that pre-pandemic there was an existing deterioration in population mental health and wellbeing, which is likely to continue as we learn to live alongside COVID-19.
- The Scottish Mental Health Research Advisory Group reported that one of the early impacts of COVID-19 was a higher level of distress. Over time, there is expected to be a worsening incidence of mental health disorders. Rates of traumatic reactions, substance misuse, self-harm and suicide are expected to increase.
- Studies have shown that there are groups in the population who are at higher risk of experiencing negative mental health impacts due to COVID-19. These include younger adults; women; those living on low incomes and individuals with pre-existing mental health conditions.
Our Scottish Mental Health Tracker Study has continued to monitor the mental health impacts of the pandemic.
Next Steps
In addition to the work we set out in the Transition and Recovery Plan, we acknowledge that there now needs to be an enhanced and specific focus on mental health as we move forward. In the next phase of our thinking about the harms that have been caused by COVID-19, it is imperative that good mental health is seen a core part of recovery. We will specifically consider any potential impacts on mental health and wellbeing (both positive and negative) of any decisions we take as we adapt.
We will:
- Acknowledge the impact on mental health that has been, and continues to be, felt across Scotland.
- Ensure that improving mental health and wellbeing is an underpinning principle as we take strategic decisions.
- Ensure that evidence on the likely effects on mental health is specifically assessed as part of any future decision-making. The likely negative effects on mental health of any future protective measures will be weighed against the public health benefits of doing so.
- Ensure that face-to-face mental health services, including group therapy and emotional support, are able to continue, as fully as possible, under any future protective measures that are required. Subject to any measures required for the safety of participants, we want services to continue to be as adaptable and flexible to best meet people's needs.
- Continue to work closely with Health Boards to improve delivery of, and access to, services.
- Refresh our Mental Health Strategy during 2022, including a consolidated set of mental health commitments to reflect the current mental health and wellbeing needs of the people of Scotland. The new Strategy will be based on the latest data and evidence, and will include measures for helping individuals to thrive, as well as laying out how the system will respond whenever anyone asks for help for their mental health. This will ultimately ensure that people can access the right support, wherever and whenever they need it.
- Publish a new long-term Mental Health Workforce Plan to ensure we continue to grow and empower the workforce to respond to evolving need.
- Adapt and evolve our policy approach as the nature of the longer-term impacts on the mental health of the people of Scotland become clear. These impacts could include serious mental ill-health, however, earlier intervention is our opportunity to ensure this is not the case wherever possible.
- Ensure access to support for anyone experiencing periods of distress or crisis, as well as support for those with ongoing needs. Across our policies, we will focus on recovery and we will further embed trauma-informed approaches across all services and sectors (supported by our National Trauma Training Programme).
- Ensure our policy approach includes a strong focus on prevention and early intervention, so that the right help is available for anyone who needs it.
- Capitalise on the increased focus on mental health and wellbeing by promoting the importance of wellbeing, particularly in the community. This will include promoting self-help measures to help people build their own resilience and further expanding the help available in the community.
Bereavement and Loss
COVID-19 has taken a heavy toll of lives in Scotland, as it has across the world. In addition, during the height of the pandemic, the need to adopt COVID-19 protective measures denied countless friends and relations of those who died the opportunity to be with their loved ones at the end of their lives – whether caused by COVID-19 or other reasons. Traditional bereavement rituals have been interrupted and for many the grieving process has been protracted or intensified.
We must acknowledge the sacrifice and loss felt by so many and find ways to commemorate and to come to terms with our losses. We must also support those grieving and suffering continued emotional trauma as a result. We will look at factors leading to someone suffering prolonged, complex grief and, in collaboration with those with lived experience, ensure the right help and support is available.
For example, the Community Memorials Project, with £4.1 million support from the Scottish Government and administered by Greenspace Scotland, will enable communities to remember in their own way. Communities will be supported by artists to develop projects that help them reflect on the impact of the pandemic. Greenspace Scotland commissioned artists will engage with community groups, faith groups and those hit hardest by the pandemic to shape ideas that benefit communities and reflect local people's experiences of the pandemic.
Social Care Resilience
Throughout the pandemic social care has been under significant pressure and the position across Scotland has been changing rapidly due to staff absences (not all COVID-related), COVID-19 outbreaks in care homes and demand for care.
Progress
As an immediate response, partnerships redeployed staff to ensure safe care within care homes and other services and all partnerships instigated some level of business continuity plans due to substantial and escalating service challenges, prioritising care for those most in need.
All partnerships have made significant efforts to secure additional staff with the appropriate skills and capability to provide the right support for people. A range of short-term actions were taken to cover the festive period, identifying additional staff with existing care or nursing qualifications. Training has also been provided rapidly to give wider staff groups basic skills to enable them to contribute. In the medium term, the priority is to support the ongoing task of recruiting and retaining more care staff at all levels.
In response to these pressures the Scottish Government has announced £300 million in additional funding as part of measures put in place to support current system pressures in the social care sector. The aim of this new investment is to maximise capacity, ensuring flow through the system, and caring for our staff. This included: £40 million for 'step-down' care, so that hospital patients can temporarily go into care homes, or can receive additional care at home support; £62 million to maximise the capacity of care at home services; up to £48 million to increase the hourly rate of frontline social care staff; and £20 million to enhance multi-disciplinary teams, so that more social work assessments can be carried out, and to support joint working between health and social care.
One of our priorities for social care is improving Fair Work practices, to help to retain and attract more workers into the sector, which builds a more stable, resilient and experienced workforce. We are committed to improving the experience of the social care workforce, including increasing levels of pay, which we know is crucial to addressing long standing recruitment issues in the sector. The Fair Work in Social Care Group has also developed a set of recommendations for minimum standards for terms and conditions reflecting Fair Work principles. This extends to the development of local standards that employees should expect. This work is now being taken forward. We are also working with key partners to promote career opportunities and pathways within social care, upskilling and developing the workforce in order to address retention issues and to attract new people to the sector as a rewarding career choice.
Next Steps
We are developing solutions to further ease the pressure across the social care system, including additional support for unpaid carers and those for whom they care. We are encouraging local authorities to make full use of the flexibility offered through Self-Directed Support (SDS), in particular so that family members and friends can be employed as personal assistants by people in receipt of SDS. This has been an important way for people to ensure they have support that suits their needs. Employing family members or friends is some people's preference, and we are considering ways to better enable this in the long term.
As a short-term measure, we are working with local authorities to encourage the provision of support prior to an assessment being carried out. Pressure across the system has meant that people have sometimes had to wait for their support needs to be assessed. Using existing powers in the Social Work (Scotland) Act 1968, if a local authority considers that there is an urgent need for support, it may provide this support before carrying out an assessment. Where it is appropriate to do this, it will allow people to receive support more quickly than might otherwise be possible.
Where support is provided in this way, it is a legal requirement to undertake an assessment as soon as practicable thereafter. Various statutory safeguards exist to protect those in receipt of SDS, and any family members who may be asked to provide support in this way. The safety of the person in receipt of support remains paramount, and social workers and other relevant practitioners will use their professional judgement to identify the most appropriate mechanism to support an individual.
Both of these approaches should help ease the burden on people who receive support and on the system itself by enabling greater flexibility in the provision of support and care.
Resilient Communities
The capability, strength and kindness of individuals, communities and third sector organisations are an essential part of Scotland's resilience to major challenges. From the earliest days of the COVID-19 pandemic it was clear that what individuals, communities and the organisations working with them were achieving together made a significant and very meaningful contribution to the response to the pandemic. We, alongside our partners across Local Government, are committed to supporting this resilience by providing necessary support and advice, and enhancing the integration of the third sector with resilience structures and processes.
Progress
Collaboration on the COVID-19 response has cemented many local relationships and connections and stimulated new ones, at community level. It has been a striking feature of the COVID-19 response that significant support has been largely from locally focused third sector groups, staff and volunteers. There has been a period of rapid learning, creativity and adaptation as people have stepped outside their usual ways of working. This has created important shifts in mind-sets and enabled a broader understanding of resilience to encompass wellbeing as key considerations alongside the economy.
The National Volunteer Coordination Hub (NVC Hub) was set up in February 2021 to provide additional volunteers for the COVID-19 vaccination and community testing programmes. It offers a single national point of contact which complements local arrangements and supports Health Boards where sufficient volunteer capacity is unavailable. It is operated by the British Red Cross, and draws on the volunteer resources of a range of third sector organisations. The Hub model has contributed over 54,500 volunteer hours of support to the range of COVID-19 response programmes across Scotland. The NVC Hub was set up as a short-term arrangement but due to its success is being extended.
Next Steps
The Ready Scotland website will continue to provide practical advice and guidance on how individuals and community groups might continue to support people within their local communities who may need practical assistance owing to COVID-19 variants and outbreaks, and enable those who wish to continue the community groups formed in response to COVID-19 to support any future response.
We will work with partners, across civic society, including our partners in Local Government, to further develop the NVC Hub users' requirements in the longer term and put sustainable arrangements in place to help meet demand for volunteer resources in future national emergencies.
Supporting Families, Babies, Children and Young People
Progress
There has been a lot to learn during this pandemic about the pressures on families, including families where the parents are no longer together. It has underlined the critical value of a holistic, whole-family approach to support, which is rooted in the community and driven by the voices and needs of babies, children and their families.
New and existing inequalities have emerged or been exacerbated, making the lives of many of the youngest in our society even harder and providing less opportunity for them to reach their full potential. Uncertainty and complexity have run through this pandemic. We will seek to reduce this uncertainty, and act to reduce complexity and help families, babies, children and young people access the help they need, how and where they need it.
Preventing further harm to current and future generations must shape our current and future responses, beginning in the earliest years of life. We know the significant pressures that the pandemic has placed on families, and we will be proactive in building multi-disciplinary and multi-agency family support services which enable families to thrive.
At the start of the pandemic, a Collective Leadership Group was formed, with partners from across agencies and the third sector to act rapidly on what was required to be in place to meet the needs of babies and children with the highest level of vulnerability. This group continues to help shape and inform the national and local responses, providing valuable local insight and challenge to inform national planning.
In learning the lessons from recent experience we will ensure that the rights of all children are aligned to what will help them grow and thrive and minimise periods where children's rights are restricted. Including children and young people in decision-making is the best way to ensure responses and adaptations are more likely to meet their needs.
We will continue to review the guidance for all services that support pregnant women, babies, children, young people and families, to reduce the risk of transmission of the virus, alongside balancing the risk of harm to children by becoming 'invisible' to services during periods of restriction. This should include prioritising face-to-face visits, in the home, wherever possible.
We will continue to review the evidence of the impact of the pandemic and the response, prioritising action to support those with additional needs and vulnerabilities to prevent further marginalisation from society. This will include considering the role of the COVID-19 Collective Leadership Group to shape our overall response, alongside other partners, including the NHS.
Lessons learned highlighted the importance of maintaining direct contact with children, young people and their families, through established trusted relationships, to ensure early offers of support are facilitated.
We remain committed to improving the journey of children and young people through the care system. We will continue to support the invaluable work of the Scottish Children's Reporter Administration (SCRA) and Children's Hearings Scotland (CHS) to deliver children's hearings as recovery from the pandemic continues.
Next Steps
We are:
- Investing at least £500 million over the life of this Parliament in Whole Family Wellbeing Funding, to provide whole family support and act as a transformation fund to shift from chronic to preventative interventions as we #KeepThePromise.
- Publishing a Promise Strategic Implementation Plan, by the end of this Parliamentary year at the latest, that sets out the commitments and actions that we will take as Government to Keep the Promise.
- Working to deliver refreshed GIRFEC (Getting it right for every child) policy and practice guidance in partnership with key delivery partners across all sectors. Refreshed materials aim to provide practitioners with the confidence, clarity and practical support to continue to implement GIRFEC which lies at the heart of all our policies and services to support children, young people and families and plays a central role in achieving our collective ambition for Scotland to be the best place to grow up.
- We will publish our next Tackling Child Poverty Delivery Plan in March 2022 which will outline the transformational actions we will take alongside partners to tackle and reduce child poverty in Scotland, in line with the ambitious targets set by the Child Poverty (Scotland) Act 2017.
Early Learning and Childcare (ELC)
Progress
We have supported the Early Learning and Childcare (ELC) and school-age childcare sectors to continue to provide high-quality and nurturing services to children and their families during the pandemic. Key actions we have taken include:
- Working with local partners to successfully implement the expansion of funded ELC from August 2021 despite the challenges of the pandemic, almost doubling the entitlement of all 3 and 4-year-olds and eligible 2-year-olds to 1,140 hours.
- Making up to £35 million of dedicated financial support available to childcare services since the start of the pandemic. On 10 February 2022, the Scottish Government announced a new Childcare Sector Omicron Impacts Fund, which will in total make up to £9.8 million available to provide one-off grants to the childcare sector this financial year.
- On 4 December 2020 we confirmed that qualifying day nurseries will continue to benefit from 100% relief on non-domestic rates until at least June 2023, worth on average £12,000 to each eligible setting.
- Working to roll out the vaccine: coverage of the vaccine is now very high, with rates of uptake of doses 1 and 2 among childcare staff comparable to the general population. Work is taking place to increase uptake of the booster in order to provide maximum protection to everyone working across the childcare sector.
Our ambition for ELC is to deliver the best possible outcomes for children, parents and families by helping to close the poverty-related attainment gap, increasing family resilience through improved health and wellbeing of children and parents, and creating opportunities for parents to access work, study or training.
ELC settings provide an essential service to children and families and are vital in supporting children's learning and development. The context for delivering ELC has changed significantly since March 2020. The work of staff across the sector to deliver care for children over the pandemic has been extraordinary. Despite best efforts, the latest data show that the society-wide protective measures that have been necessary have affected young children's relationships and development, with children from low-income families being more negatively impacted.
Next Steps
Our key strategic aims over the next 12 months are:
- Continued commitment to working in partnership with Local Government and other partners to prioritise children's outcomes and deliver the right balance of specific measures, ensuring a continuing focus on priority groups.
- Re-focusing efforts on sectoral resilience and proofing against pandemic and other shocks, to keep staff, children and families safe across local communities.
- A focus on recovery to support the sector to address the impacts of COVID-19 on children and families, working with partners in Local Government, and wider society.
We will work with our partners in the childcare sector, child contact centres, public health, local government and the regulatory bodies to learn lessons from the experiences of 2020-2022 and agree the principles that will govern our management of the endemic phase and any future public health emergencies.
Building on our established childcare sector Financial Sustainability Health Check and ongoing engagement, we will continue to assess the financial impacts of the pandemic and take further steps to support the long-term sustainability of all parts of the childcare sector. We will work with local government to embed COVID-19 recovery in spending plans for 2022-23 through the specific grant funding for 1,140 hours and the forthcoming Resource Spending Review.
Through the development of our 5-year Childcare Workforce Strategy, to be published later this year, we will work with the sector and skills bodies to support the current and future workforce to deliver high-quality care and learning in a safe and sensitive way, mindful of the impacts of the pandemic. In taking this forward, we will enable the childcare workforce to access professional learning resources and specialist services that will support them as they work with children and families through our recovery from the pandemic. We will also increase support and resources for staff wellbeing by further developing the Team ELC Wellbeing Hub.
In order to ensure additional resilience across the system, we will work with Education Scotland on further development of learning-at-home resources which can be used by staff supporting children who are unable to attend settings and we will work with Parent Club on additional resources and advice for parents.
We will simplify and streamline the suite of COVID-19 guidance for ELC settings, school-age childcare and childminding services to enable a more 'normal' ELC experience for staff, children and families as the virus becomes endemic. This will include work to support practitioners to maximise the use of outdoor space and to increase the amount of time children spend outdoors every day, learning from the experience of the pandemic.
In addition to the Childcare Sector Omicron Impacts Fund, ELC settings will be able to benefit from additional funding of £5 million, which is being made available to make sure ventilation is as effective as possible.
Schools
Progress
In line with advice from the WHO and elsewhere, one of our top priorities has been, and will remain, to keep early learning and childcare (ELC) settings and schools open and safe, and to ensure continuity of the care, education and support they provide to children, families and communities.
Our Reducing Risks in Schools Guidance and COVID-19 safety guidance for ELC settings, school-aged childcare and childminding services set out the protections that local authorities, schools and settings should ensure are in place. Those protections are kept under close review based on advice from the Advisory Sub-Group on Education and Children's Issues, through consultation with the COVID-19 Education Recovery Group (CERG) and other stakeholder groups.
We will continue to review that guidance, and the measures set out within it, to ensure that they support a strategic move over time to managing rather than suppressing the virus, and that they support the best possible outcomes for children. Appropriate and proportionate protective measures – aligned with those across society given the determined level of risk at any stage - will continue to be required to manage the virus. We will engage closely with public health experts, staff, parents and representative bodies in determining those measures and to minimise the operational and educational impacts, while keeping children and staff safe.
Good ventilation remains important in controlling the spread of COVID-19 so our guidance sets out how to ensure a balance between fresh air and warmth. Up to £5 million is being made available to support local authorities to make sure ventilation is as effective as possible, and that any urgent remedial action is undertaken in schools and ELC settings. This is on top of a previous £100 million of COVID-19 logistics funding - £10 million of which was specifically for ventilation and CO2 monitoring to complete initial assessments of all learning, teaching and play spaces.
Next Steps
Our ambition for education in Scotland remains to deliver excellence and equity for all, with health and wellbeing at the forefront of our plans. This builds on the previous recommendation of our International Council for Education Advisers to work towards a 'pandemic-proof' education system.
Our document Education Recovery; Key Actions and Next Steps included a number of actions that will help to turn this aspiration into a reality. For example, in 2022-23 we will commence preparatory work to ready the school estate and the people in it for an influx of new technology from 2023-24 onwards, leading to a fully digitally enabled education system by the end of this Parliament.
Alongside this, based on feedback and learning, we continue to make improvements to Glow services as well as to evolve and improve the National e-Learning Offer (NeLO) to make sure it best supports the changing needs of schools and learners as the pandemic conditions change.
Practitioners are currently supported in the pedagogical and technical use of digital technology for face-to-face, blended and remote learning though a range of professional learning and leadership opportunities provided by Education Scotland.
Since the start of the pandemic we have taken action to ensure additional teachers and support staff are in the system to aid education recovery. We have provided additional funding of £240 million for these staff and school census data show that we now have over 2,000 more teachers in the system than before the pandemic.
This injection of additional resource is providing vital additional support to the education system when it is most needed. Our commitment to increase teacher numbers by 3,500 over the course of this Parliament will ensure that capacity and resilience in the system continues to build over the coming years.
The wellbeing of all children and young people has been a central focus of our response to date. We will work closely with key stakeholders to agree future priorities that will ensure we build on the work already undertaken to ensure children and young people get the right support at the right time, with an updated Additional Support for Learning action plan to be published in spring 2022.
We continue to support our local authority partners with £16 million in funding to ensure that every secondary school has access to counselling services. Our online professional learning resource supports school staff to understand and recognise the range of mental health and wellbeing concerns young people may experience. We have also introduced new guidance to support whole-school approaches to mental health and wellbeing, complementing the work that education authorities and schools already do to support children and young people's mental health and wellbeing. We will continue to work with the Mental Health in Schools Working Group to embed these approaches across Scotland.
We have already invested over £2 million in supporting teacher wellbeing. Support is also available for those in leadership roles which focuses on looking after their own mental health as well as the mental health and wellbeing of their teams. We intend to offer a similar package of wellbeing professional learning to the education workforce going forward, and are working with partners to progress that.
We have continued to prioritise the support of children and young people who need it most, including through an investment of £1 billion to support education recovery and tackle the poverty-related attainment gap. In recognition of the impact of both the pandemic and poverty across Scotland, the refreshed Scottish Attainment Challenge programme will see funding reach all 32 local authorities, with a framework for recovery and accelerating progress, being developed with the system, to support greater progress in tackling the poverty-related attainment gap and improve outcomes for children and young people impacted by poverty.
In addition, we will continue to take forward recent Organisation for Economic Co-operation and Development recommendations, including considering the outcomes of the reform work being undertaken by Professor Muir and the work of Professor Hayward on the assessment and qualifications system. Any major reform of the qualifications system will require careful consideration and will take time to develop and fully implement.
It is our firm intention that exams take place this year, with contingencies for any further disruption. Results for the 2022 National Qualifications will be published on 9 August. Decisions on the approach to the 2023 National Qualifications will be informed by public health advice at the time, and by the views of stakeholders.
Colleges, Universities and Community Learning and Development
Progress
We recognise the impact of COVID-19 on students and staff and continue to work collaboratively with universities, colleges, Community Learning and Development (CLD) providers, trades unions and student representatives, and on the basis of input from the COVID-19 Expert Advisory Sub-Group on Universities and Colleges, to provide support and to develop sector guidance. This has enabled the safe resumption of in-person teaching.
Our financial support to students during the pandemic has been substantial. Over £96 million has been provided via hardship funding, digital access support, mental health support and for student associations. This funding has included:
- A £5 million Digital Inclusion Fund, which was provided to support over 13,500 post-school learners access online learning.
- For mental health, £4.2 million funding has been allocated for the 2021-22 academic year, a £0.6 million increase from 2020-21. In addition, £4.4 million was announced to help college students and staff respond to the pandemic.
We continue to urge students experiencing financial hardship to apply to their college or university for support from the Further or Higher Education Discretionary Funds.
Next Steps
Over the past two years, in-person teaching and learning has been severely restricted and we recognise the harmful impact that will have had on students, staff and society more generally.
Our strategic aims in the weeks and months ahead are:
- To work with colleges, universities, CLD providers and wider stakeholders to manage COVID-19 effectively, and in line with the Scottish Government's overall Strategic Intent, in order to ensure that in-person teaching is the appropriate and desirable position for most courses;
- To work with stakeholders in order to address the impacts of the accumulated wider harms and lost learning on students and learners.
On the basis of advice from the COVID-19 Advisory Sub-Group on Universities and Colleges, we will work with our partners on the Advanced Learning COVID-19 Recovery Group – Chaired by the Minister for Higher Education, Further Education, Youth Employment and Training – to develop a framework, to replace prescriptive sector-specific guidance. This will enable decisions on COVID-safety protocols and measures, beyond any that may be in place across society, to be determined locally and, where possible, collectively. The focus of this framework will be to monitor the wider pandemic context and potential implications for the sectors; provide information, high-level guiding principles and support for the sectors; and to allow local solutions tailored to particular needs and circumstances.
As part of this approach to managing the virus, we will work with universities and colleges to support the development of institution-level COVID-19 Response Committees, where possible retaining existing structures put in place over the pandemic. The Committees – comprising representatives from the institution, trade unions, student bodies and providers of purpose-built student accommodation – will monitor public health advice and the wider context, with a view to adjusting institution safety protocols accordingly. We will work with the Committees to consider appropriate surveillance and monitoring methods.
We will work also with universities, colleges and CLD providers to ensure good ventilation is a key focus across their estates and the buildings they use.
The COVID-19 Advisory Sub-Group on Universities and Colleges has focused much of its work since the start of this academic year on the impact of the pandemic on the wider harms and lost learning on students. Over the next 12 months we will continue to consider these impacts as work intensifies across the Scottish Government on recovery from the pandemic.
We will also work with institutions, the Scottish Qualifications Agency and other professional accreditation bodies to pursue sustainable, alternative approaches to assessment/accreditation which can be used should the public health situation require it.
Housing
The pandemic has underlined the importance of home as a place of safety and of housing for health outcomes more generally. It is important that essential housing services to tenants such as repairs, maintenance, allocations and lettings, dealing with anti-social behaviour, domestic abuse and housing management issues, tenancy sustainment and homelessness prevention work all continue.
Progress
Guidance on the effective provision of housing support and services in the context of COVID-19 has been made available in partnership with the housing sector and frequently updated. This draws on learning from the experience of the pandemic about how to support essential works in homes in a way that keeps staff and tenants safe.
We remain fully aware of the financial difficulties facing many people as a result of the pandemic, and are doing all we can to support them. We have made clear since the outset that taking eviction action against those who have suffered financial hardship should be an absolute last resort, and have put legislation in place requiring private landlords to work with their tenants to manage rent arrears before seeking eviction. Emergency legislation temporarily extended the notice period a landlord must give, and to enabled the Housing and Property Chamber of the First Tier Tribunal for Scotland to take all the circumstances into account in repossession cases and introduced private landlord pre-action protocols (these set out the steps a landlord should take to support a tenant in rent arrears before commencing eviction action). This legislation is currently in place until 31 March 2022 and the Government will shortly confirm its position on extension of provisions to 30 September 2022.
Next Steps
The Coronavirus (Recovery and Reform) (Scotland) Bill sets out our intention to implement both private landlord pre-action protocols and Tribunal discretion on a permanent basis, helping to support the private rental sector in its recovery from the pandemic. We have also provided support totalling £39 million to tenants during the pandemic, including a £10 million Tenant Grant Fund for people at risk of homelessness because of changes to their finances, and money for discretionary housing payments to those needing help with housing costs.
The pandemic has shown what is possible when we work collectively and has increased our determination to end homelessness and rough sleeping. From the outset we worked in partnership with local authorities and the third sector to ensure everyone had a safe place to stay, and the number of people sleeping rough in our cities remains low. Building on our updated Ending Homelessness Together action plan, we are committed to continued action and partnership working to ensure nobody returns to rough sleeping. People with no recourse to public funds will be particularly vulnerable to homelessness when public health requirements change. We will continue to work collaboratively with COSLA to provide local authorities with clarity on their duties and with the third sector to develop a cohesive approach to support those most at need.
We will work with frontline homelessness organisations to continue to explore creative solutions that help people who are homeless or rough sleeping to access vaccinations. We will build on the success of previous initiatives, which included flexible vaccination appointments, drop-in clinics and on-site vaccinations being made available in temporary accommodation locations. We will continue to fund local authorities' Rapid Rehousing Transition Plans (RRTPs) and have committed to further funding for 2022/23 and 2023/24 to enable local authorities to plan over a two-year period. This will encourage a continued housing-led approach to addressing homelessness.
In addition we are currently reviewing the COVID-19 framework to support Gypsy/Traveller communities. Gypsy/Travellers face additional risks and vulnerabilities during the COVID-19 pandemic and living situations may make it difficult for them to limit virus spread and comply with public health guidelines. As we move to a more sustainable level of support, there is an opportunity to embed approaches which would allow Gypsy/Traveller communities to follow public health advice and more easily access the facilities and services that they need.
Transport
Progress
Since the beginning of the pandemic we have taken actions to ensure our operators and delivery partners have continued to provide a safe and reliable transport system for those using our transport network. We have provided over £1 billion since the start of the pandemic to support transport operators to maintain essential services for those who rely upon them. We have also:
- Provided up-to-date guidance for those who operate and use our transport networks;
- Monitored and assessed the demand for travel, in order to support the evidence to adapt the transport system;
- Assessed the COVID-19 transport impacts and measures, including changes to economic and social activity, and subsequent travel demand; and
- Engaged extensively with operators, stakeholders and delivery partners (transport operators, COSLA, regional transport partnerships, poverty groups, the Mobility and Access Committee for Scotland, business umbrella groups and academics) to work collaboratively on our response to COVID-19.
Next Steps
We are now taking forward a broad package of work to ensure that there is a viable and sustainable transport system for the future. As part of this we are developing work to facilitate a safe and confident return to public transport as more people begin to travel between their home and their place of work and as demand for leisure travel also increases. We are:
- Undertaking activities to promote a safe and confident return to public transport;
- Updating operator and passenger guidance to support safe provision and use of public transport services;
- Engaging with operators and delivery partners to promote safe behaviours and the measures required to support our recovery from COVID-19; and
- Monitoring and assessing travel demand and identifying evidence of changes to travel behaviours and public transport demand that have become embedded due to COVID-19.
Justice
Progress
Across the wider justice system, we recognise the operational and service delivery challenges posed by the pandemic, which has had considerable impacts for justice agencies and third sector organisations who play a critical role in supporting those who engage with the justice system. As the criminal justice system recovers from the pandemic, we aim to build a justice system that is fit for the future and build on work already undertaken under the umbrella of the Recover, Renew, Transform Programme to support recovery and reform of the justice system.
Next Steps
The Scottish Government continues to support justice agencies to take action to address the backlog caused by the pandemic. In our January 2022 budget statement we announced significant funding increases for the justice portfolio - funding that is required to deal with the backlog. We have established a justice recovery fund of £53.2 million in the next financial year to be allocated to recovery, renewal and transformation activity across the justice system as we emerge from the pandemic. This will include funding of £26.5 million to the Scottish Courts and Tribunals Service to maintain enhanced court capacity and remote jury centres.
We have previously committed an additional £50 million in 2021-22 to support our Recover, Renew, Transform Programme for the criminal justice system – which has included setting up 16 additional solemn and summary courts from September 2021. The additional £50 million is being used in a variety of ways to increase capacity across the justice system, including the recruitment of additional staff, greater use of digital tools for criminal, civil and administrative justice activity and improved support for victims and witnesses. We recognise the harm caused to victims, witnesses and those accused of crime by delays within the justice system. Justice agencies have been clear that the recovery programme will take several years to address the backlog and we will continue to support that work.
The Coronavirus (Recovery and Reform) (Scotland) Bill will continue certain temporary justice system provisions on a longer extension basis as part of the Recover, Renew, Transform Programme and as a response to the impact of COVID-19 on the justice system, particularly where backlogs have unavoidably built up.
The Scottish Prison Service has, in line with Scottish Government guidelines, gradually and cautiously lifted regime protective measures that were necessary to protect the health and wellbeing of those who live and work in our prisons. A Restoration of Services project supported establishments to return to pre-pandemic regimes by the end of September 2021. Measures remain in place to allow for regime changes where this is deemed necessary in an outbreak situation. The Scottish Prison Service continues to work collaboratively with all health boards to maximise opportunities for providing vaccinations to those in their care. From 26 April 2021, it has enabled greater access to in-person visits in establishments with robust local risk assessments in place and implementation of protective measures for staff, prisoners and visitors. In-person visit provision has continued, and has only been affected when there has been a localised outbreak.
Contact
Email: CEU@gov.scot
There is a problem
Thanks for your feedback