Preparing for Emergencies Guidance
This guidance provides advice, considerations, and support from a strategic lens for Health Boards to effectively prepare for emergencies in compliance with relevant legislation.
Section 4 - Planning For Emergencies
This section highlights the wider context within which bodies listed as responders under the Civil Contingencies Act 2004 should plan and prepare for emergencies. It sets out roles and responsibilities at various stages of the emergency planning process in line with these requirements.
Introduction
4.1 The planning process is key to preparing for emergencies. Under the Civil Contingencies Act 2004, Category 1 responders are obliged to have arrangements in place to plan, exercise and review their capability and responses against a range of disruptive challenges, crises, disasters, or emergencies. These obligations involve three key functions as part of the planning process:
- assessing risk
- ensuring that (scalable) plans are in place to reduce or mitigate the effects of the emergency if/when it occurs
- identifying other actions to be taken in relation to the emergency
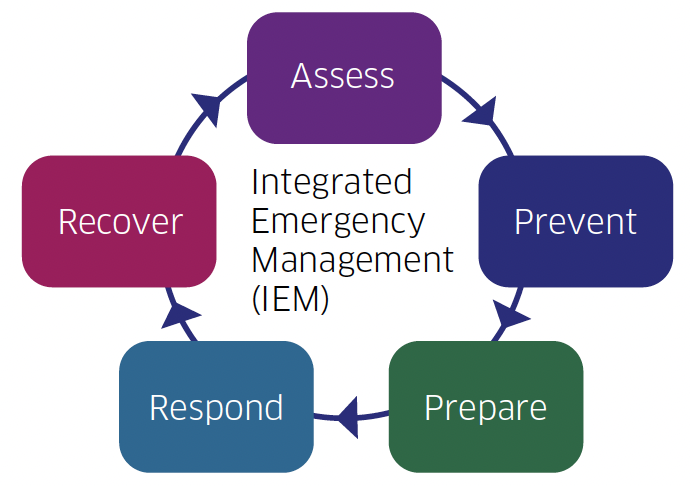
4.2 Health Boards should use the Integrated Emergency Management (IEM) cycle, working together with multi-agency partners via Resilience Partnerships to build resilience. The IEM cycle (below) ensures a constant review of activity and therefore robust preparedness arrangements.
4.3 the planning process should demonstrate that the Health Board has:
- engaged key internal and external stakeholders and partner agencies, particularly Category 1 and 2 responders and voluntary sector agencies that have an emergency response and support capability in developing its Major Incident Plan
- developed appropriate and suitably resourced ‘command, control and coordination’ (C3) arrangements
- established a programme of training, testing, and exercising to ensure effective implementation of their plans
- appropriate incident recording arrangements in place and a system for identifying and sharing learning from incidents
- established a system for reviewing and updating their plans
Roles and Responsibilities
4.4 Health Boards designated as Category 1 and Category 2 responders must ensure they comply with the legally mandated duties of the CCA associated with their designated status. As such, they should ensure they are able to contribute to a co-ordinated response to major incidents, regardless of their nature or scale.
4.5 Non-designated Health Boards should consider how they may be affected by emergencies. While there is no legal duty on them to adhere to these regulations, failure to adhere will disrupt their normal operations and therefore, every effort should be made to adhere as if a designated Category 1 or Category 2 responder. Failure to do so could result in criticism - for example at a public inquiry. Non-compliance is not simply about potential criticism at an inquiry, but that their day-to-day operations will be more affected if they do not follow regulations, best practice, and have effective measures in place.
4.6 The specific duties of Health Boards identified as Category 1 responders under the CCA are to:
Assess risk
4.7 Risk assessment (of hazards, threats, and vulnerabilities) is the first stage in organisational resilience and business continuity planning. All Health Boards should ensure internal corporate risk management processes include risk to continuation of services that single and multi-agency plans are evidence-based and proportionate.
4.8 They must develop and maintain an internal/organisational Risk Register and actively participate in the development of multi-agency Local and Community Risk Registers produced by the Regional Resilience Partnership in the context of national risk registers.
Maintain Emergency/Major Incident Plans
4.9 Health Boards must produce and maintain major incident/emergency plans for a range of potential scenarios based on their assessment of possible and major incident scenarios. They must also actively engage with other resilience partners/organisations to ensure that the role of the NHS is appropriately reflected in multi-agency plans for various major incidents/ emergencies.
Maintain Business Continuity Management Plans
4.10 Business Continuity Management (BCM) is an essential activity in establishing an organisation’s resilience by enabling it to anticipate, prepare for, respond to, and recover from disruptions and to have a clear understanding of dependencies with other organisations.
4.11 All Health Boards must have in place robust up to date BCM plans to help maintain their key functions in the event of a major incident or significant disruption. BCM plans should identify:
- management arrangements aligned to relevant risks
- critical/prioritised services, analyse the effects of disruption and the actual risks of disruption and actions to mitigate them
- activation procedures and escalation processes
- recovery steps to ensure the service can return to operation
- how the plan(s) will be maintained and reviewed
- how the plans(s) will be communicated to and accessed by staff
For further information on BCM see Appendix 2.
Communicate with the public
4.12 Category 1 Health Boards must have communication plans that can:
- at the planning stage: inform the public of the risks and threats being prepared for and, in general terms, of their potential responses if they occur
- at the response stage: warn, inform, and advise the public using different types of messages and a variety of methods appropriate to the needs of the audience
For further information, see the guidance on communication in Section 5.
Share information
4.13 Information-sharing is an integral part of civil protection and interagency cooperation. Health Boards must share information with other categorised responder organisations and their Major Incident Plans should be available in the public domain, accepting that sensitive or confidential information cannot always be shared with partner agencies and/or the public.
4.14 Careful consideration must be given to the type of information that is required to plan for a major incident and what information can be shared in the context of the CCA and the Freedom of Information (Scotland) Act 2002 while maintaining confidentiality.
4.15 Health Boards must ensure that there are free-flowing, informal channels of communication and information-sharing with other agencies involved in civil contingencies work. It is important that Caldicott Guardians advise on disclosure of information and are available to support and guide staff.
4.16 Different Health Boards have different roles in sharing and disseminating information. A Territorial Health Board will need measures to communicate patient safety information and advice to those directly affected by an incident, whereas a non-territorial Health Board will need to prepare advice for the general public. All Boards should, in line with their regular duties and risk assessment processes, consider their potential roles in various types of incidents and prepare to co-operate with other Boards in fulfilling these.
Co-operate
4.17 Health Boards designated as Category 1 and 2 responders must cooperate with other responders. The principal mechanisms for multi- agency cooperation are the Regional/ Local Resilience Partnerships (RRP/ LRP). Category 1 responder Health Boards should be represented on these multi-agency groups by staff at an appropriate level within the organisation, as follows:
RRP Chief Executive or a delegated Executive-level Director (Territorial Health Board); Regional Director or Deputy Director of Scottish Ambulance Service (SAS)
LRP Resilience Manager/Resilience Advisor/Senior Manager (Territorial Health Board); Regional Head of Service or Area Service Manager (SAS)
4.18 Other Health Boards, such as NSS and PHS, which may not be directly represented on these groups should – wherever needed - continually consult with Health Boards on any issues relevant to planning for, responding to, or recovering from an incident. This engagement can be bilateral or multilateral as appropriate.
4.19 It is important that Health Boards, especially those within the same Resilience Partnership area, develop capacity and capability for specific incidents especially those that may have a longer-term impact on service provision, by collaborating with each other. Primary care and other relevant contracted service providers, IJBs, local authorities and voluntary agencies should be involved in these planning processes, as appropriate, so that they are aware of the Health Board’s plans and/or its expectations in the event of a major incident.
Legal frameworks, Public Inquiries and Civil Action
4.20 NHS legal obligations and duty of care for patients does not change during major incidents or emergencies that are likely to generate high profile media attention or scrutiny. In such situations it is likely that legal investigations and challenge such as criminal investigations, Fatal Accident and/or Public Inquiries or Civil Action may follow. These may occur a long time after the incident.
4.21 When planning for major incidents, it is essential that Health Boards have arrangements in place to record the decisions made and actions taken and store all the records and documentation safely for future reference should they be required for evidential or audit purposes.
Contact
Email: health.eprr@gov.scot
There is a problem
Thanks for your feedback