Neurological care and support - framework for action 2020-2025: midpoint progress report
The midpoint progress report marks the halfway point in the 5 year framework. It highlights key achievements, challenges and future priorities for improving neurology services as we continue to implement the framework.
Progress Report
Progress is reported under each of the five aims in the Framework. Funded projects are a key part of delivering the Framework aims and many straddle a number of commitments. Selected case studies are used to illustrate impact, and provide a snapshot of the breadth and range of the work that has taken place across all of the projects. A full listing of all funded projects is included in Appendix 3.
From 2022 onwards we will prioritise:
- Establishing local networks for practice sharing, learning and improvement in neurological services;
- Developing strategies to ensure long-term sustainable impact of funded projects, including those that support mental wellbeing;
- Understanding how we can collect more reliable data on prevalence;
- Piloting approaches to work force planning for Allied Health Professionals (AHPs) in neurology;
- Piloting competency frameworks for neurology Clinical Nurse Specialists;
- Working to address gaps in neuropsychology and neurophysiology;
- Continued roll out of Scottish Epilepsy Register to improve patient safety and assess the potential use of this approach for other neuro conditions, and;
- Working with the development of National Care Service, Rehabilitation Framework, Workforce Strategy and other linked strategies that contribute to development of service improvement.
Aim A. Ensure people with neurological conditions are partners in their care and support
The Framework includes the 'pyramid of support', in which the first (largest) tier aims to empower people living with neurological conditions to self-manage their condition effectively within their communities.
Graphic text below:
Pyramid of Support
- Specialist support/Condition-specific
- Generic and neurological health and social care and support
- (Supported) self-management, peer support and information provision.
- Carer resources/signposting
Patient and carer information
Public-facing information about neurological conditions is being developed for the NHS Inform website, to support education and self-management. Information on multiple sclerosis, Huntington's disease, epilepsy, migraine, Parkinson's disease and dystonia is being revised. New content is being developed on myasthenia gravis, transverse myelitis, post-polio syndrome, ataxia, Tourette syndrome, multiple spinal atrophy, muscular dystrophy and progressive supranuclear palsy. Future work is also planned for cerebral palsy, motor neuron disease and functional neurological disorder.
We supported the Neurological Alliance of Scotland (NAoS) to produce three new 'What to Expect' information guides for carers on Anticipatory Care Planning, advocacy services, and becoming a new carer. These were endorsed by the Coalition of Carers and are available at the NAoS website: Neurological Alliance of Scotland (scottishneurological.org.uk).
Five projects have developed or are developing patient information to support people to better understand their conditions. One of these covers a range of neurological conditions, two cover acquired brain injury, one functional neurological disorder, and one non-epileptic seizure.
University of Edinburgh, Chest Heart Stroke Scotland, NHS Lothian, Pogo Studio, Edinburgh Headway - Tailored Talks is an innovative digital presentation platform which delivers comprehensive information to patients and carers with a wide range of neurological conditions. This supports shared decision-making, consent and signposting. Content is now available for 20 neurological conditions and this will continue to grow as individuals using it identify areas of unmet need. A process of training clinical staff to use the system is moving forward.
The effectiveness of Tailored Talks has been demonstrated through incorporation into the stroke pathway, supporting conversations with patients and relatives, helping them to work through choices between striving for survival with a high likelihood of severe long-term disability, or focusing on optimising patient comfort.
Supported Self-Management
Ten funded projects have developed supported self-management services across a range of conditions. Two for multiple sclerosis (MS), one for Parkinson's, one for spina bifida/hydrocephalus, one aimed at carers, three for epilepsy and two for all neurological conditions. All of these have been led by third sector organisations.
The key focus of these projects has been on meeting mental and physical wellbeing needs through interventions such as physiotherapy, yoga, counselling, meditation, clinical support, or social activities. They have been responsive to individual needs including in addressing the impacts of COVID-19. They have provided online and face to face support, including one-to-one and peer support.
MS Society: Wellbeing Hub benefits a pan-Scotland community, namely people living with and affected by multiple sclerosis. It provides a variety of virtual activities to help support the MS community with their emotional and physical health. These include tailored 1:1 physiotherapy, counselling and information, through to group activities including Pilates, MS Warrior Programme, meditation and much more. The project is delivering a suite of 1,129 livestream sessions (639 up to March 2022) benefiting around 780 unique individuals across Scotland. People can try 'taster sessions' before committing to a full series/course and the project is developing partnerships to trial a blended model of delivery to include in-person sessions. Participants completed emotional and wellbeing evaluations before and after participation demonstrating improved scores in a number of areas including life satisfaction and anxiety. Wellbeing hub (Scotland) | Multiple Sclerosis Society UK (mssociety.org.uk)
"I wasn't dealing with any of my emotions before the counselling and now I know how to. It was a big help that [the counsellor] knew and understood MS and from the start I felt comfortable with her. Thank you all. I recently took part in the MS Warrior programme. I bought some dumbbells and have now remembered how much I loved doing weights at the gym."
Most of these projects work with statutory providers to encourage referrals, and in some cases have developed data sharing agreements to improve referral pathways. Qualitative evaluation of their benefits for service users has been very positive and they often address previously unmet need. This meets the aspirations articulated in Realistic Medicine to 'create the conditions that help people make informed choices and express their views about their treatment and care options, based on what matters most to them'.

The MS Centre Mid Argyll specialises in support for people in rural and remote areas and has been funded to extend its 'Lifeline' services to people affected by various neurological conditions across Argyll and Bute. These gentle movement classes have been provided as part of a programme that combines online and in-person support.
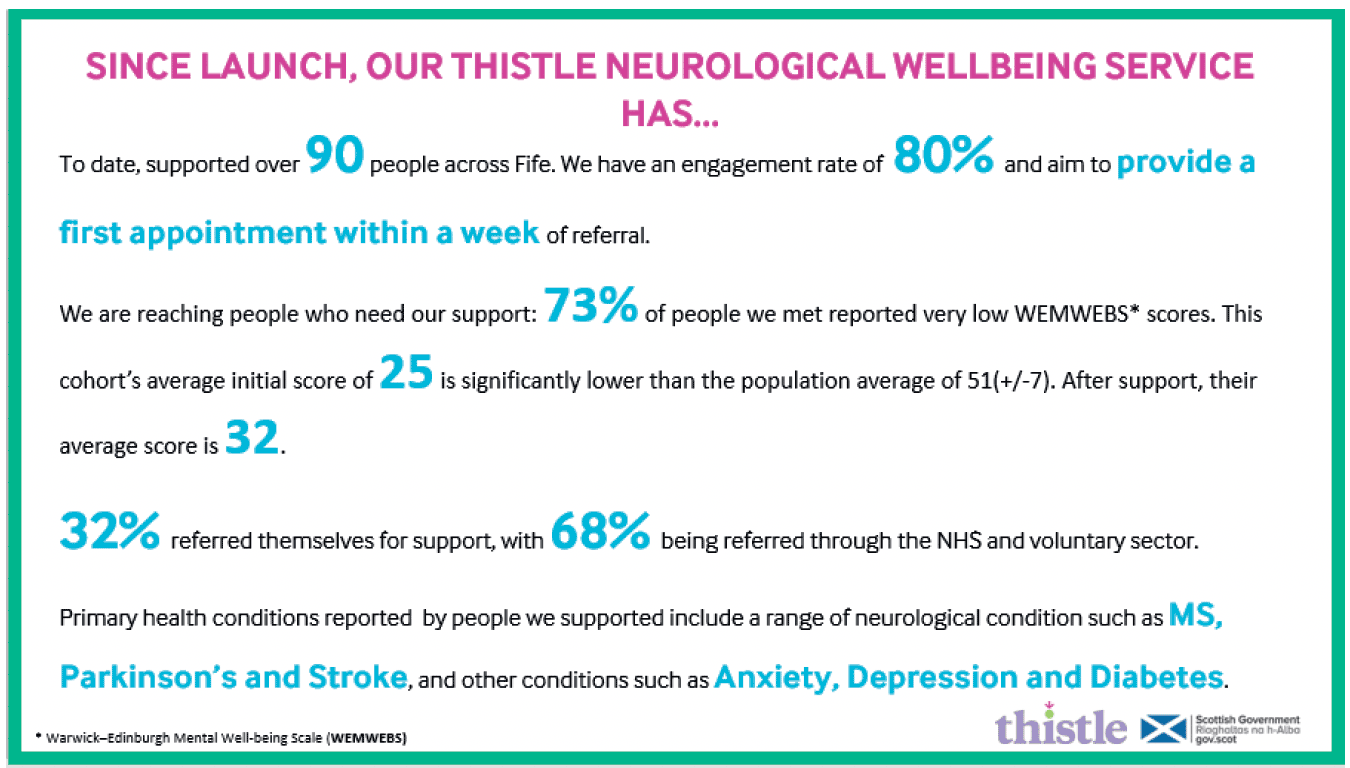
Thistle Health and Wellbeing: Neurological Wellbeing Service has developed a self-management programme for people in Fife living with a neurological condition, and their carers. This helps them to take control of their lives by developing coping, confidence, and resilience, helping them to be less isolated and more connected to their communities.
A data-sharing agreement has been put in place with NHS Fife, allowing referrals to the programme which offers specialist, condition specific support, including a 10-week lifestyle management course and the opportunity for peer support. This delivers person-centred rehabilitation, focusses on early intervention, and addresses key aspects of physical function, mental health, and wellbeing, while accounting for social determinants of health, health inequalities and trauma.
People living with neurological conditions are also able to self-refer for support by emailing referrals@thistle.org.uk
"I love the people on the course, and it's great to speak to people in similar situations. Yes, I would recommend this course to others. I just wish I had this at the beginning of my condition".
"What would your advice be to someone at the same point you were at 10 weeks ago? I would say sign up without hesitation, it will help enormously".
"One of the things that I'm determined to be is not the guy with the Parkinson's, what the course has taught me is, asides from meeting like-minded people is that you can actually become more than just your illness"
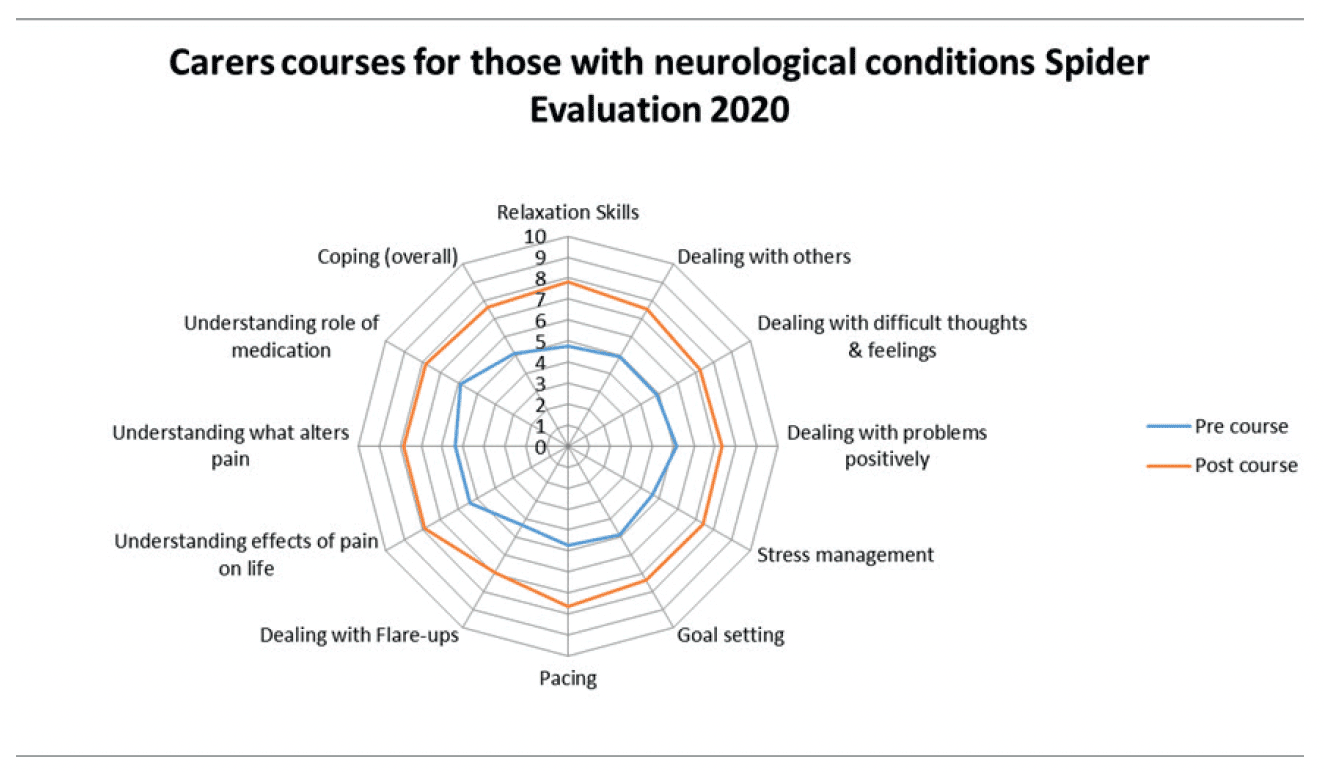
The Pain Association received funding to deliver online carers sessions with a 96% course completion rate – this spider diagram shows evaluation pre- and post-course.
Spina Bifida Hydrocephalus Scotland: Healthy Ageing Hub. A Wellbeing Matrix that incorporates 'health personas' as a tool for decision support, focusing on wellbeing rather than ill health. The project has extended its Mental Health and Wellbeing Counselling service and developed the Wellbeing and Ageing Hub with a range of resources to provide support.
MyCarepod is an app that allows people to engage remotely with those providing care, improving the quality of communication during consultations. Development of a data-sharing agreement with NHS Lothian allows the project to test the app in a clinical setting. Service users will now be able to contribute to their own health record by entering data which they can then share with their GP and specific consultants. Early discussions are under way with the aim of replicating this approach in other NHS boards in the future, as part of a long-term goal to provide integrated health and social care for people with spina bifida/hydrocephalus. Once testing is complete there are 1,039 potential users of the app.
Participants from Quarriers Lifestyle Management discuss their experiences. This project uses a 'House of Care' model where people can define what is important to themselves, work collaboratively with their team of healthcare workers to develop their own strategies for change and identify allies and supporters once they leave the William Quarriers Epilepsy Centre.
Challenges
The majority of these projects rely on staff costs, meaning that long-term sustainability is a challenge. Many are seeking direct funding from statutory organisations and other sources to ensure longevity. The Scottish Government will continue to support engagement between third sector and statutory partners to promote the benefits of these models of service delivery.
Aim B: Improve the provision of co-ordinated health and social care and support for people with neurological conditions
Five funded projects support statutory bodies to develop collaboration across sectors to improve integrated care and support for people with neurological conditions. These are in Tayside, Midlothian, Angus, Orkney, and Forth Valley. Improvement focusses on areas such as optimising referral pathways, better networking of and information on local services, and establishment of collaborative improvement groups.
Angus Health and Social Care Partnership: Neurological Enhanced Community Support is developing a proactive and comprehensive wrap-around support service for people with a movement disorder, to prevent crisis management and optimise wellbeing for as long as possible.
Combined assessments by specialist and community nurses provide a coordinated support package for patients from both secondary and community care. The test area approached 20 people with 12 agreeing to take part. Areas of co-ordinated care include polypharmacy reviews (11), referrals to 3rd sector and peer support (4), referral to allied health professional support (6), orthotics / assessment for an electric wheelchair (1), counselling (1), increase in frequency of review by MS Nurse (5), change of prescription (2), MRI scanning (1), consultant review (3), offer of Disease Modifying Therapy (1), continence referrals (1). Social prescribing and carers support has also been offered.
The programme is being developed with a collaborative steering group consisting of senior Health and Social Care Partnership staff, carer organisations, community care and improvement leads. Qualitative feedback from patients and staff is currently being gathered and will provide evidence to support the spread and adoption of this approach to other localities. Proposals to embed specialist nurses within both secondary care & primary care are being developed.
One project has developed a best practice model for people as they transition across care settings. One is building and testing the implementation of flexible support services combining virtual and in-person multi-disciplinary therapy for people with cerebral palsy.
Anticipatory Care Planning
We worked with Healthcare Improvement Scotland (HIS) to facilitate an online learning event to raise awareness of and build confidence amongst health and social care staff in Anticipatory Care Planning for people with neurological conditions. This was attended by over 280 people. We created a Neurological Anticipatory Care Planning webpage with HIS featuring useful tools for healthcare professionals and videos of the webinar presentations. ACP and neurological conditions - ihub | Health and social care improvement in Scotland - Anticipatory Care Planning and Neurological Conditions
NHS Ayrshire & Arran, Cerebral Palsy Scotland, ARC Housing: Development of neurology specific principles of good transition. This project sought to develop principles of good transition across the lifespan of people with neurological conditions, and used a range of methodologies. A systematic review of current literature completed within the first phase informed the second phase in which data was gathered from those who have experienced transition (e.g. life-stage transitions across health and social care, education, employment) to inform future models of care.
The outcomes confirm that transition is associated with a range of negative emotions. Barriers to successful transition include the lack of holistic approaches to care: lack of choice, assumptions, lack of pathways, lack of access, lack of support and lack of co-ordination. People living with a neurological condition feel disempowered and experience a lack of empathy, lack of compassion and a lack of understanding.
Examples of more positive transitions included: adaptable and flexible approaches to care and support; personalised care planning with involvement of the service user in key decisions about their care; use of an asset-based approach; including technology enabled solutions where appropriate.
Accessible outputs from this work will lead to wider adoption across all groups of people who access, deliver and advocate for improved services. The outcomes will also be sustained through academic publications, in anticipation of informing national and international guidelines.
Review of Neurological Framework Funding
Following the second round of funding in March 2021, we reviewed and adjusted the scope of the neurological fund to focus on delivery of integrated services, long term sustainability and scalability. A third round of awards was announced March 2022. New projects awarded funding are:
- Epilepsy Scotland - Electronic, community-based screening for depression, anxiety, and suicidality in people with epilepsy, and provision of appropriate support interventions.
- Migraine Trust / NHS Grampian - Work with pharmacists to help people with migraines manage their symptoms and treatments more effectively.
- NHS Greater Glasgow & Clyde and Partners - Partnership Delivery Group to ensure enhanced patient experience and to support people to live well.
- PAMIS - Buddying system to introduce postural care to individuals with neurological conditions and families and help them connect with appropriate services.
- Quarriers, Epilepsy Connections, Lanarkshire Epilepsy - A national epilepsy collaborative across the third sector and NHS Scotland to bring about greater consistency in patient experience and improve pathways for care.
- Strathcarron Hospice, Talking Mats Ltd, SCSC - Visual framework to help people with neurological conditions express their views about Anticipatory Care Planning.
Challenges
Projects have often faced challenges of staff capacity to engage in improvement initiatives. One project hasn't been able to start due to recruitment challenges. Whilst time is needed for these projects to make changes and improvements to systems, the approach to whole system change is one that needs to be scaled up and embedded through a network of people providing leadership at a local level across Scotland.
Digital technology has been used by a number of projects to support the Framework's aims and commitments. These include training resources for staff; patient and carer information; self-management tools that enable engagement with healthcare professionals before and after appointments; data gathering and healthcare surveillance systems; and engagement with service users using video technology. Digital platforms have great potential to be scalable, with hosting and maintenance often being the main ongoing costs. In some cases, funding for this has not yet been identified, and we will engage with colleagues in digital healthcare to explore potential solutions to this. Some digital platforms have potential to be adapted to use in other neurological conditions.
Aim C: Ensure high standards of effective, person-centred, and safe care and support
We have recruited a multi-disciplinary cross-agency working group to develop and implement a quality assurance programme for the General Standards for Neurological Care and Support. This is being led by HIS and will support health and social care providers to identify what they are doing well and where they can improve. A self-assessment and peer review process will be developed and tested in 2022-2023 and implemented in 2023-2024. This group of NHS, Health and Social Care Partnership, third sector leads and people with neurological conditions will consider how generic neurological standards can inform a condition specific approach to national and local improvement.
A data search of the primary care data system (SPIRE) has been completed. Analysis is taking place and will be published in the summer of 2022. This will provide much more reliable prevalence data on neurological conditions than ever before. The request was delayed for months due to technical and pandemic related issues. The data will be used to inform more effective service planning.
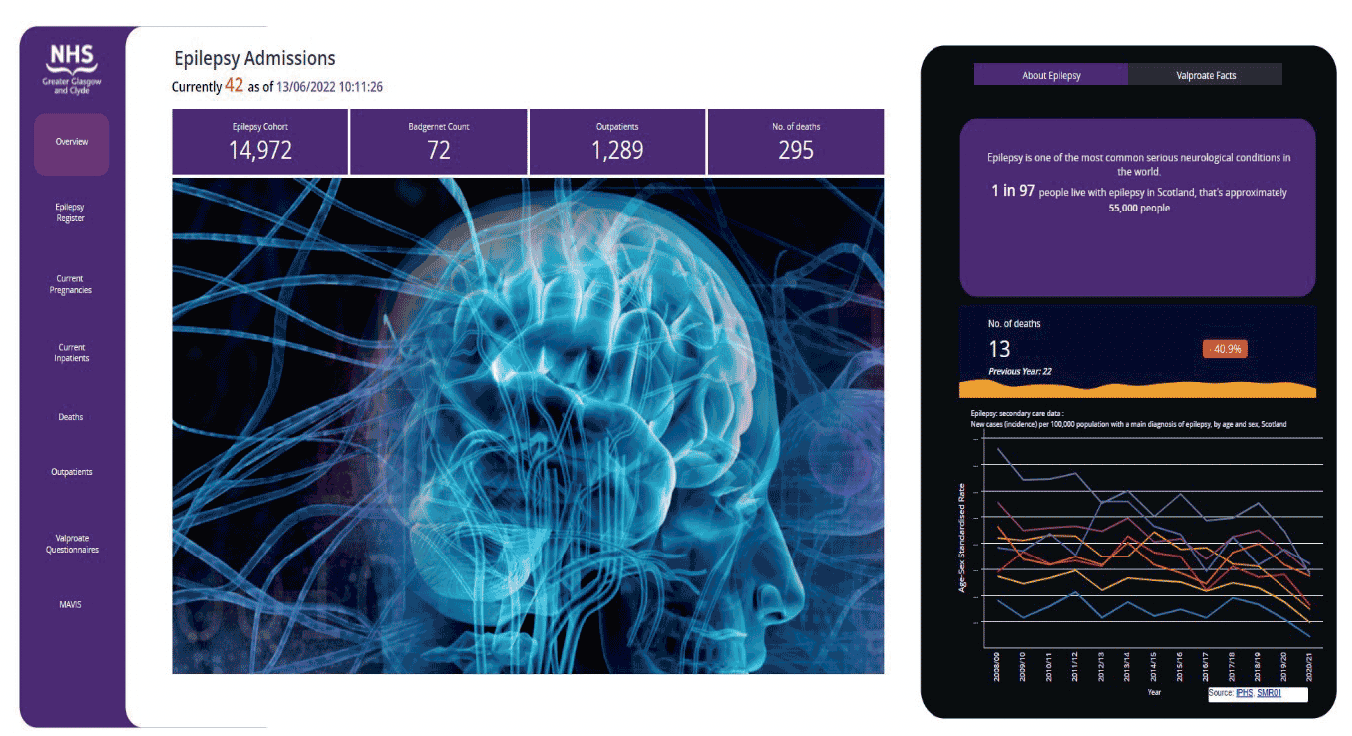
Commitment 12 of the Framework aims to gather better data regarding neurological conditions. The Scottish Epilepsy Register project, funded through the Framework, is focussed on improving data collection and patient safety. We have scoped with medical neurologists proposals for improving availability of data and as a result of this, developed proposals to scale up and consolidate the work of the Scottish Epilepsy Register. The benefits of this project are illustrated in the case study below and may ultimately serve as a replicable model for other neurological conditions.
We funded the Neurological Alliance of Scotland to facilitate Scotland's involvement in a UK-wide patient experience survey for neurological conditions and analyse the data. 834 people in Scotland participated and mental health, waiting times, person centred care, and support for children with neurological conditions were key areas of improvement identified. This will be repeated bi-annually to track comparisons over time that will inform framework progress. In doing so we will continue to work with the data, to understand the underlying factors contributing to it, and to listen to lived experience in developing solutions.
NHS Greater Glasgow & Clyde: Scottish Epilepsy Register uses routine health data to improve the care of people in Scotland living with epilepsy. This clinical platform quickly alerts healthcare professionals to a 'key event' experienced by the patient. At the time of writing, we are able to:
Identify women with epilepsy at a time of booking during pregnancy, ensuring timely review and support, as there can be pregnancy-related risks regarding the condition and its treatment. All women are contacted shortly after booking (prior to this, 30% of women were never seen during pregnancy)
Evaluate adherence to anti-seizure medication using the novel MAVIS app. Applying this to women with epilepsy during pregnancy identified more than 50% had stopped their medication prior to booking. This allows healthcare professionals to discuss with women the importance of medication during pregnancy and the risk of untreated epilepsy.
Identify the frequent use of unscheduled care and hospital admissions by people with epilepsy, and target care to those at greatest risk of harm.
Identify serious adverse events, including death, allowing healthcare professionals to support next of kin in a timely manner.
It is anticipated that this healthcare improvement project will be shared with colleagues in NHS Lanarkshire, Ayrshire and Arran and NHS Tayside within the next 6-9 months. Our hope is that this will act as primer to create a comprehensive Scottish Epilepsy Register.
The Scottish Government is supporting research to identify improvements in care and treatment for neurological conditions. The following have commenced or will report during the period of the Framework:
- doctorate study looking at new and effective approaches to diagnosis and treatment of ME/CFS;
- identification of the top 10 priorities for future research on ME/CFS;
- Decode ME;
- Future MS - personalised approaches to clinical management of multiple sclerosis;
- SPRINT-MND/MS - 12 PhD's recruited and the final cohort due to complete in 2022;
- 2 Postdoctoral scientists working on MND at the Edinburgh Labs of the UK-Dementia Research Institute;
- Precision-MS: Integrating Precision Metrics of Brain Health into Early Treatment of Multiple Sclerosis, and;
- Research into new treatments for motor neurone disease, and Duchenne muscular dystrophy (DMD) (awarded March 2022).
Challenges
The data commitment in the Framework is ambitious and includes challenges around accurate recording of disease coding, lack of integration of data systems across care settings, and cultural commitment amongst staff in valuing the need for accurate data. We plan to address these through proposals to scale up the Scottish Epilepsy Register and by linking with work to improve electronic patient information systems.
Aim D: Ensure equitable and timely access to care and support across Scotland
Two funded projects have worked to improve care pathways. One to scope expertise for progressive supranuclear palsy (PSP) & Corticobasal Degeneration (CBD) (see below), one to test a model of Advance Physiotherapy thus reducing referrals to consultants.
The Centre for Sustainable Delivery (CfSD) supports implementation of proven approaches to health pathways at a national level. A continuing focus is on encouraging adoption of Active Clinical Referral Triage (ACRT) and Discharge Patient Initiated Review (Discharge PIR).
ACRT ensures that a senior decision maker reviews all of the relevant information following referral to secondary care. Patients who will not benefit from a secondary care appointment are returned to primary care with advice (to the patient and/or GP) at the beginning of their wait. This supports timely access to secondary care for those patients who will benefit from it.
For Discharge PIR, rather than offering routine return appointments at the convenience of the health care system, patients are discharged, but know how to re-access care, support and advice as is relevant to them and their clinical need.
There has been a significant amount of work championing sensitive and appropriate adoption of these approaches in neurological services in Scotland. Centre for Sustainable Delivery is working with Public Health Scotland to establish a standardised way of capturing data in relation to ACRT and Discharge PIR, which will provide a better understanding of the scale, spread and potential further opportunity of these approaches.
We published guidelines for clinicians on conducting virtual appointments in neurology, covering use of different technologies and their suitability for assessing a range of neurological conditions: >Digital Consulting in Neurology | TEC Scotland. We delivered an online seminar for Allied Health Professionals to support the launch of this guidance attended by 38 people. The introduction of effective virtual appointments, where appropriate, will contribute to improving timely access. We will evaluate the reach and impact of this guidance.
PSP Association (PSPA): Service mapping of health and care staff for people with PSPgressive supranuclear palsy (PSP) & corticobasal degeneration (CBD). This plotted connections that people and their families can expect throughout the progression of their disease and identified gaps in provision, duplication, and unhelpful processes. It enabled dedicated time to make contact with all relevant health and care professionals known to PSPA. It resulted in good quality learning and relationship-building with new contacts in the care of people with PSP & CBD, including some areas where there were no previous contacts.
It introduced PSPA and its resources to patients and professionals, to improve recognition of the conditions and help those affected to access the right services at the right time. PSPA's guide for GPs and primary healthcare teams, 'Red Flag' symptom posters and a guide for occupational therapists were also updated.
Aim E: Build a sustainable neurological workforce fit for the future
Four projects have been funded that build staff capacity and knowledge. One for rehabilitation, one for myalgic encephalomyelitis(ME)/chronic fatigue syndrome (CFS), one for functional neurological disorder (FND), and one for acquired brain injury.
We have scoped workforce priorities and work has commenced to address these with a focus on nursing, allied health professionals (AHPs), neuropsychology and neurophysiology.
The Transforming Roles paper on Clinical Nurse Specialists (CNS) was published in 2021. This provides core competencies for CNS roles at level 6 and level 7. An expert group is reviewing how existing competencies for conditions such as epilepsy, MS, motor neuron disease and Parkinson's align to Transforming Roles with a view to identifying challenges or barriers to accessing training to develop and sustain this workforce.
We are testing with neurology in the West of Scotland, a workforce capacity planning tool for Allied Health Professionals that has been developed through the Excellence in Care programme (which aims to ensure a consistent standard and quality of care). This will help to ensure staffing levels are in line with safe staffing legislation. An AHP workforce development matrix will support better training and career development. This will launch later in 2022.
We are linking with a review of scientific neurophysiology training being progressed by the Chief Healthcare Sciences Officer.
Action for ME and partners: Learn about M.E./CFS - informing professional practice in Scotland. Five podcasts for professional medical education on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome have been developed and delivered. A Continuous Professional Development training module has been downloaded 4,261 times (UK wide) and 1,065 times (Scotland-wide; target 500). Qualitative evaluation has been undertaken showing increased confidence in managing ME/CFS, indicating that 78% of participants felt confident after taking the module, compared to 33% beforehand. Learn about M.E. | Action for ME
NHS Lanarkshire developed and are evaluating Goal setting and Action Planning (G-AP) online training resource. Evidence and theory based, the G-AP framework informs goal setting practice in community rehabilitation settings. Consistent with the principals of Realistic Medicine, G-AP supports a person-centred, collaborative approach.
The G-AP online training resource prepares multidisciplinary staff to deliver G-AP in practice. Downloadable resources include a person's record of their goals, plans and progress and an accessible version (Access G-AP) to support people with cognitive and/or communication difficulties. Following a large scale multisite evaluation, the intention is to make the G-AP online training resource freely available to rehabilitation staff working with people with neurological conditions throughout NHS Scotland and beyond. G-AP Weblink
Challenges
The ability to obtain accurate data on workforce numbers presents a significant challenge. Our workforce assessment identified pressures across all areas of the workforce in neurology. Training and development of staff into specialist roles is a challenge that takes time. We have set up the Redesign Project Group to address workforce and care pathway challenges and are linking with colleagues in workforce, nursing, and healthcare sciences teams.
Contact
Email: Clinical_Priorities@gov.scot
There is a problem
Thanks for your feedback